Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Research Article - (2023)Volume 13, Issue 4
Introduction: Low-load exercise training with concurrent venous occlusion (Low-Load Blood-Flow-Restricted Exercise: LL-BFRE) has gained interest in clinical rehabilitation. Various orthopedic patients suffering from knee joint disorders would benefit from either i) maintaining or ii) increasing lower limb muscle strength and skeletal muscle mass. Due to the low load, and concurrent ability to increase muscle strength and promote muscle hypertrophy, LL-BFRE seems relevant to apply in clinical rehabilitation. The aim of the present study was to investigate the feasibility of LL-BFRE as a clinical rehabilitation method in patients suffering from various knee joint-related injuries. A secondary objective was to analyze change in functional performance, knee muscle strength and patient-reported outcomes.
Methods: Patients suffering from i) knee osteoarthritis (n=3), ii) persistent postoperative knee pain, or persistent functional performance deficits after surgery were included (n=9). LL-BRFE was performed twice weekly for 4-8 weeks as unilateral leg press at 30% 1 Repetition Maximum (RM) with partial venous occlusion (40% complete limb occlusion pressure) around the proximal part of the thigh. Timed Up and Go, 30-second chair-stand-test, Thigh Circumference (TC), isometric knee extensor strength, and the Knee Osteoarthritis Outcome Score (KOOS) was performed at baseline and follow-up.
Results: Four patients dropped out due to i) pain aggravation, ii) ruptured Baker's cyste, iii) loss of motivation, iv) personal reasons. Adherence to training was 95.6%. Significant improvements were achieved in both Timed Up and Go and 30 seconds sit to stand (p ≤ 0.03). As did isometric knee extension strength on the affected limb (p=0.05), and 5 RM on the affected limb (p<0.01). Three out of five KOOS subscales improved more than 10 points, while no significant change was seen for thigh circumference (p=0.08).
Conclusion: The study indicates that LL-BFRE is feasible in patients suffering from various orthopedic knee joint disabilities and can be a part of a physical therapy rehabilitation program. Furthermore, the patients achieved both functional improvement, increased muscle strength, and demonstrated clinical meaningful improvements in their experience of knee pain, knee symptoms, and participation in sport and recreation activities.
Venous occlusion; Rehabilitation; Exercise training; Physical therapy; Muscle
Patients suffering from knee pain due to musculoskeletal disorders such as orthopedic surgery, overload- or disuse-related disorders are often prone to skeletal muscle atrophy and weakness [1]. This is often related to pain-related alteration in the habitual activity level and/or altered locomotion in addition to potential postsurgical de- loading, ultimately rendering the patients' musculoskeletal system to gradually deteriorate. That is, a decline in activity induces a fast loss of skeletal muscle mass and function resulting from the unloading and lower neural activation of muscle [2].
Degenerative muscular adaptations due to immobilization from major surgery can affect the patient’s ability to recover to their pre-injury physical activity levels [3-5]. That is, elderly patients are in risk of never reaching preoperative functional performance after surgery [5]. Thus, interventions targeting skeletal muscle hypertrophy and strength are highly warranted for patients unable to maintain their normal activity level.
Heavy-load Resistance Strength Training (HRST) (training load ≥ 70% of 1 Repetition Maximum: RM) is often considered the exercise method of choice to promote muscle hypertrophy and increase muscle strength [6,7]. The American College of Sports Medicine recommends loading intensities of 60% to 85% of 1 Repetition Maximum (RM) to achieve skeletal muscle hypertrophy and strength gains [8]. However, HRST can be contraindicated or, at worst, deleterious in some patients due to postsurgical load restrictions and/or pain restrictions. Thus, to counteract disuse atrophy in these particular patients, alternative methods for promoting hypertrophy and increasing strength is required.
Resistance training with Low Loads(LL) (~30% of 1 RM) performed with concurrent partial Blood Flow Restriction (BFR) of the working limb (LL-BFRE) has consistently been demonstrated to promote muscle hypertrophy and increase strength in both healthy and patient populations comparable to HRST [9-11]. Several mechanisms have been suggested to be involved in the muscular adaptations seen with LL-BFRE [12]: The restrictive pressure applied to the limb during LL-BFRE creates a hypoxic environment distal to the cuff causing a metabolic stress in the working muscles. The hypoxic environment may lead to increased type II muscle fiber recruitment, increased inflammatory and endocrine response, cellular swelling, and elevated intramuscular inorganic phosphate, all of which have been demonstrated to mediate protein synthesis and satellite cell proliferation [10,12,13]. A recent systematic review found LL-BFRE to be safe and effective in improving quadriceps strength in patients suffering from orthopedic disorders such as patients undergoing Anterior Cruciate Ligament-Reconstruction (ACL-R), patients suffering from knee Osteoarthritis (OA), patients suffering from patellofemoral pain, and patients undergoing knee arthroscopy. In line with this, a recent randomized controlled trial, demonstrated that LL-BFRE and HRST were equally effective in improving knee extensor strength in patients recovering from ACL-R. However, the group performing LL-BFRE has greater improvements in patient reported outcomes and a knee joint effusion compared to the group performing HRST [14]. Furthermore, LL-BFRE exercise has been suggested to decrease sensitivity to pain (i.e. exercise-induced hypoalgesia) to similar levels as prolonged high intensity exercise [15]. Thus, the combination of exercising with low loads and concurrent BFR seems attractive to offer to patients with persistent symptoms and reduced functional performance despite several previous unsuccessful rehabilitation efforts.
As the patients included in the present pilot study, had failed several previous rehabilitation efforts prior to engaging in LL-BFRE, the main purpose of the project was to determine the feasibility of LLBFRE in patients suffering from knee pain due to orthopedic knee disorders in terms of adherence. Also, we wanted to determine to what extent objective functional performance measures and measures of mechanical muscle function was feasible to evaluate pre-to-post changes in these patients. Lastly, we investigated evaluated changes in functional performance, knee muscle strength and patient-reported outcomes based on the collected data.
Experimental design
This study was a pilot study with one group where all participants received LL-BFRE. Patients referred to the study was baseline tested, trained for 4-8 weeks twice a week and finally, follow-up tested. Patients performed the first LL-BFRE session on the same day as baseline testing. Follow-up assessments were conducted 3-7 days after last exercise session as shown in Figure 1.
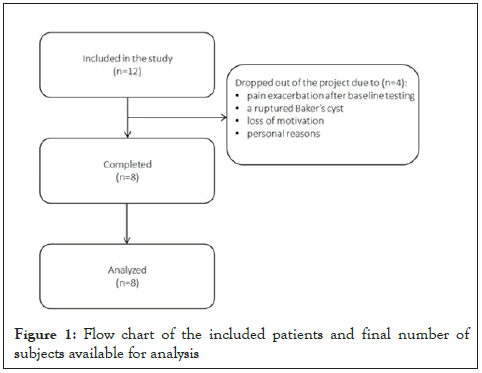
Figure 1: Flow chart of the included patients and final number of subjects available for analysis
Patients were included if they suffered from knee pain due to an orthopedic disorder, were ≥ 18 years of age, and was able to adhere to ≥ 4 weeks of twice-weekly LL-BFRE. Patients were excluded if they suffered from cardiovascular diseases, had a history of previous a stroke incident, diagnosed with unregulated hypertension (systolic >180 mmHg and/or diastolic >110 mmHg), displayed wound healing dysfunctions, had a history of previous thrombosis, suffered from a chronic traumatic nerve injury, suffered from renal insufficiency, were diagnosed with diabetes, were a smoker, suffered from a spinal cord injury or were pregnant.
Eligible patients were referred to the study by orthopedic surgeons and collaborating physiotherapists at Horsens Regional Hospital. Also, patients diagnosed with knee Osteoarthritis (OA) not eligible for knee prosthesis were recruited at two OA seminars held at the hospital. Common to all was that all patients were diagnosed with a knee-related disorder or injury and had engaged in several (at least two) previous unsuccessful rehabilitation efforts (i.e. not reduced symptoms nor improved subjective experienced functional performance). The patients were diagnosed with knee OA, two patients were conservatively treated for Anterior Cruciate Ligament (ACL) rupture, two patients had undergone ACL-R, two patients suffered from patellar tendinopathy, one patient suffered from non-specific knee pain, one had received several unsuccessful knee surgeries due to meniscus resection, and one had received a total knee arthroplasty. Thus, several different diagnoses were allowed to participate in the project, hence reflecting the variety of patients visiting an inpatient hospital rehabilitation clinic.
Intervention
Supervised LL-BFRE was performed twice weekly, with a minimum of one day between each session. We offered the patients to define an appropriate exercise period ranging from 4 to 8 weeks. The reason to offer the patient to exercise for 4-8 weeks was twofold: i) to gain knowledge in the appropriate exercise period from a patient perspective, and ii) because the project was carried out during the spring where many people traditionally tends to spend two to three consecutive weeks of holiday. Thus, to include as many patients as possible, we decided to allow some differences in the exercise period. The reason for choosing a specific exercise period was not registered.
The pressure required to fully restrict blood flow to the exercising limb (Limb Occlusion Pressure: LOP) was determined with a pneumatic, conically shaped, 12 cm wide, rigid cuff (Occlude Aps, Denmark) attached to the patient’s most proximal area of the thigh on the affected side. The patient sat on the examination table with the ankle and 1/3 of the lower limb off the table. Meanwhile a vascular Doppler probe (EDAN Instruments, inc., China) was placed on over the medial tibial artery to capture the auscultatory pulse. The cuff was gradually inflated in 20 mmHg steps until the auscultatory pulse was interrupted (LOP) [16-18].
Training protocol
After 5 minutes of warm up on a stationary bike, patients performed leg press with concurrent BFR of the exercising limb. To gain experience with how to apply BFR-exercise in orthopedic patients with several previous rehabilitation efforts, we decided to offer patients two different LL-BFRE protocol consisting of different initial exercise volumes: Protocol 1 consisted of 4 rounds with 30 repetitions (reps) in round one, 15 reps in round 2, 15 reps in round 3 and to volitional failure in round 4. Protocol 2 started with 3 rounds of 20 reps in round 1, 10 reps in round 2 and to volitional failure in round 3, and gradually increased the total training volume until 30-15-15-to volitional failure was reached as shown in Table 1. The between-round rest period was 30 seconds and both protocols utilized 40% LOP which was maintained during the entire exercise. Three patients performed protocol 2 while the remaining performed protocol 1. Patients started each session on the affected limb. Immediately after last repetition, the cuff was deflated. Subsequently, the non-affected limb performed the same amount of work as the affected limb (i.e. same cuff pressure, load, and deflation after last rep). After the last rep on the contralateral limb, the patients were recommended to stay seated for 2-5 minutes before standing up. All sessions were supervised by a physiotherapist (SLJ) to ensure sufficient loading and progression as shown in Figure 2.
| Exercise variable | Description of the exercise variables |
|---|---|
| PROTOCOL 1 | All sessions |
| Level of LOP | 40% |
| Sets | 4 |
| Load intensity | 30% 1RM |
| Repetitions 1st set | 30 |
| Repetitions 2nd set | 15 |
| Repetitions 3rd set | 15 |
| Repetitions 4th set | To volitional failure |
| Contraction modes per repetition | |
| Concentric | No restrictions |
| Isometric | 0 seconds |
| Eccentric | No restrictions |
| Rest between repetitions | 0 seconds |
| Range of movement | maximum |
| Rest between sets | 30 seconds |
| Rest between sessions | ≥ 36 hours |
Table 1a: Overview of Protocol 1 used in the present study. No progression during the exercise period. LOP: Limb occlusion pressure; RM: Repetitions Maximum. The load was increased if the patients were able to perform more than 15 repetitions in the last set.
| PROTOCOL 2 | Session 1-3 | Session 4-7 | Session 8+ |
|---|---|---|---|
| Level of LOP | 40% | ||
| Sets | 4 | ||
| Load intensity | 40% | 40% | 30% 1RM |
| Repetitions 1st set | 20 | 20 | 30 |
| Repetitions 2nd set | 10 | 10 | 15 |
| Repetitions 3rd set | To volitional failure | 10 | 15 |
| Repetitions 4th set | - | To volitional failure | To volitional failure |
| Contraction modes per repetition | |||
| Concentric | No restrictions | No restrictions | No restrictions |
| Isometric | 0 seconds | 0 seconds | 0 seconds |
| Eccentric | No restrictions | No restrictions | No restrictions |
| Rest between repetitions | 0 seconds | 0 seconds | 0 seconds |
| Range of movement | maximum | maximum | maximum |
| Rest between sets | 30 seconds | 30 seconds | 30 seconds |
| Rest between sessions | ≥ 36 hours | ≥ 36 hours | ≥ 36 hours |
| Progression | The minimal possible load (10 kilo) is added when patients perform >15 repetitions in 3rd set | The minimal possible load (10 kilo) is added when patients perform >15 repetitions in 4th set |
Table 1b: Overview of the protocols used in the present study. Gradually
progressing the training volume per session. Every third session, the
volume was increased until reaching session number 8. From session 8, the
training volume was kept constant. LOP: Limb occlusion pressure; RM:
Repetitions Maximum. The load was increased if the patients were able to
perform more than 15 repetitions in the last set.
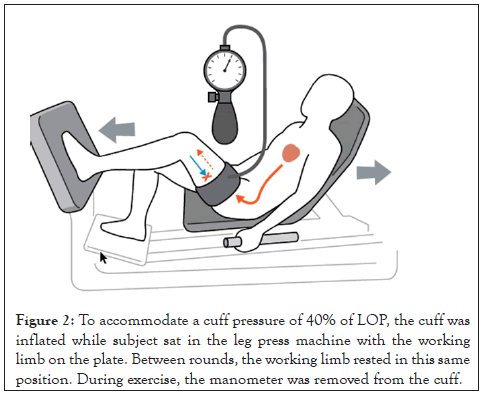
Figure 2: To accommodate a cuff pressure of 40% of LOP, the cuff was inflated while subject sat in the leg press machine with the working limb on the plate. Between rounds, the working limb rested in this same position. During exercise, the manometer was removed from the cuff.
Outcomes
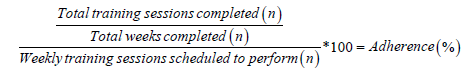
Adherence: At the first visit, the patients estimated how many weeks they intended to participate which were used to calculate the adherence. Acceptable adherence to training was not defined a priory [19]. The adherence was calculated as
Descriptive measurements: Bodyweight, age, gender, and referring diagnosis were registered.
Baseline and follow-up tests: Prior to the physical tests at baseline and follow-up, patients completed the Knee Osteoarthritis Outcome Score (KOOS). KOOS is a patient-administered knee specific questionnaire comprising five subscales: Pain; Symptoms; Activities of daily living; Sport and Recreation; and Knee-Related Quality of Life. Each item is scored from 0 to 4. The raw score for each of the five subscales is the total sum of the associated item scores. Scores can be transformed to a 0 to 100 scale. The scores of the five subscales can be expressed as a composite outcome profile, higher scores indicating fewer problems. KOOS is responsive to change following non-surgical and surgical treatments of the knee [20]. Normally, a 8-10 point change is defined as a clinically relevant change in score [21,22].
The physical tests were executed chronologically as listed below:
Thigh Circumference (TC): With the patient lying supine, thigh circumference was evaluated on both limbs by measurement of thigh circumference 10 cm abobe apex patella to the nearest 0.1 cm [23].
30 Seconds Chair Stand Test (30 s CST): Sit to stand function was assessed using a 44 cm high chair (seat height). Before testing, the physiotherapist demonstrated the movement after which the participant performed two practice repetitions to demonstrate the understanding of the test. From sitting on the chair, the patient performed as many sit to stands with full hip- and knee extension as possible in 30 second with the arms crossed in front of the chest. The patient descended until the buttock made contact with the chair. The patient was allowed to reverse the downward-movement as soon as the participant felt the chair. Thus, participants did not have to bear weight through the buttock. Only repetitions correctly performed (i.e. as described above) were counted. 30 s CST is associated with lower limb strength and functional performance. The 30 s CST is considered a valid and sensitive measure of lowerextremity sit-to-stand function with good to excellent intra- and inter-observer reliability [24].
Timed Up and Go (TUG): The TUG was used to determine functional mobility and assess the time required for patients to stand from a chair (seat height 44 cm), walk around a tape mark 3 meters away, and sit onto the chair at return. The patient was instructed to walk as fast and safely as possible towards a tape mark (and touch the tape mark (with at least one foot), turn around and return to the chair and sit down. Use of armrests was allowed. After receiving verbal and visual instruction. The participant performed two trials of which the fastest trial was used for further analysis. Up to one minute of rest was allowed between trials. Good inter-rater reliability has been demonstrated with the TUG test [24].
Maximum isometric Contraction of the Knee Extensors (MVC KE strength): Unilateral MVC KE strength was measured on both limbs with a Hand-Held Dynamometer (HHD) (JTech Commander Power Track Muscle Dynamometer MMT, USA) as previously described in detail by Jorgensen et al. [17]. Measurements were performed with patients sat on an examination table with the calf hanging beside the examination table resulting in a 90° flexion of both the knee joint and the hip joint. The HDD was positioned 5 cm above the medial malleolus and was fixed with adjustable straps to the examination table to allowing all MVCs to be performed at 90° knee flexion in all patients. The patient was instructed to sit with the hands crossed in front of their chest and to produce as much force as possible into the HHD. Patients received four trials on each leg with thirty second rest between each trial. For analysis, the mean maximal strength of the second, third and fourth trials was calculated and corrected for bodyweight (Nm/ body mass (kg)). Good-to-excellent inter and intra-rater reliability has been demonstrated on group-level in patients suffering from knee OA for maximum knee extensor muscle strength testing with HDD [25].
1 Repetition Maximum (1 RM) leg press strength: 1 RM leg press strength was estimated from a 5-8 RM leg press test (leg press machine: Technogym Element +). Patients performed three lowload warm-up sets starting at 10 kg and gradually increasing the load with 10 kg in each set. The first and second warm-up sets consisted of 12 repetitions, and the third warm-up set consisted of eight repetitions. Between each set, the participant rested for 120 seconds while sitting in the machine with the feet away from the platform. After the warm-up, the load was increased to determine the 5 RM. If the 5 RM could not be determined within three trials (i.e. fourth, fifth, or sixth set), a fourth all-out trial (as many repetitions as possible) was performed. The 1 RM was calculated as: 1 RM leg press (kg) = (1,1307·[5 RM leg press (kg)])+0,66998) [26]. For all patient unable to perform a 5 RM leg press test, the initial exercise loads was set to 20 kg.
Statistical analysis
Descriptive statistics are presented as means (Standard Deviation: SD) or medians with range. Normality was evaluated by graphically plotting the data (i.e. histograms and Q-Q plots). Changes from pre to post-intervention were evaluated using paired t-tests provided the assumption of normally distributed data was fulfilled. The Wilcoxon signed-rank test was used in cases where data did not follow normal distribution. Also the absolute mean change as well percentage mean change is presented along with cohen's d effect size where 0.2=small effect size; 0.5=medium effect size; and 0.8=large effect size. If the result of parametric and non-parametric tests gave the same results, the result of parametric tests was presented. The level of significance was set at 5% (p ≤ 0.05). All statistics were performed in Stata (Stata/MP 16.1 for Windows). The purpose of the project was mainly to determine the feasibility of LL-BFRE in patients suffering from lower limb injuries. Therefore, no power calculations for treatment effects were performed.
Eligible patients
Twelve patients (six women) with a median age 50.3 (range 25-81) and a mean body mass of 79 ± 15 kg were included in the study. Eight (five women) patients completed the intervention as shown in Figure 1. Five patients completed protocol 1 and three patients completed protocol 2. The average LOP was 192 ± 43 mmHg (range 100-280 mmHg).
Adherence
Training adherence for the eight patients who completed their planned training period was 95.6% (8%). When related to a prior adherence, eight of the 12 patients participated in ≥ 90% of the planned exercise sessions. On average, each patient completed 11 sessions (range: 8-16).
Four patients dropped out due to pain exacerbation after baseline testing (n=1), a ruptured Baker's cyst (n=1), loss of motivation due to long-distance commute (¨~50 km each way) (n=1), personal reasons unrelated to the trial (n=1) as shown in Figure 1.
Patient-reported outcomes
Only KOOS Sport and Recreation demonstrated a significant improvement with a concurrent large effect size as shown in Table 2. Both Pain, Symptoms, Sport and Recreation demonstrated a clinically meaningful change and large effect sizes as shown in Table 2.
| Outcome | n | Pre | Post | Mean Change |
95% CI mean change |
P |
|---|---|---|---|---|---|---|
| Thigh circumference: Affected limb (cm) | 6 | 45.3 ± 3.9 | 46.3 ± 5.0 | 1 | [-0.2-2.2] | 0.08 |
| Non-affected limb (cm) | 5 | 47.5 ± 4.6 | 47.5 ± 5.1 | 0 | [-1.0-1.0] | 1.0 |
| Timed Up and Go (sec): | 7 | 11.4 ± 16.4 | 9.4 ± 13.1 | -2 | [-5.0-1.0] | 0.02 |
| 30 seconds sit- to-stand test (repetitions): | 7 | 15 ± 4.0 | 17 ± 4.0 | 3 | [0.5-5.0] | 0.03 |
| Knee extension MVC: Affected limb (N/kg) | 5 | 2.4 ± 0.4 | 3.9 ± 1.2 | 1.5 | [0.5-3.0] | 0.05 |
| Non-affected limb (Nm/kg) | 5 | 3.8 ± 1.0 | 4.4 ± 0.6 | 0.6 | [-0.4-1.7] | 0.2 |
| 5RM leg press: Affected limb (kg) | 2 | 70.5 ± 6.4 | 88.5 ± 6.4 | 18 | [18-18.0] | <0.01 |
| KOOS : Pain | 6 | 66 ± 19 | 77 ± 20 | 11 | [-1.5-23.9] | 0.07 |
| Symptoms | 6 | 62 ± 15 | 71 ± 13 | 10 | [-0.3-20.0] | 0.06 |
| Activities of Daily Living | 6 | 68 ± 28 | 74 ± 23 | 6 | [-3.7-16.4] | 0.2 |
| Sport and Recreation | 6 | 23 ± 20 | 43 ± 26 | 19 | [1.2-37.2] | 0.04 |
| Quality of Life | 6 | 40 ± 13 | 47 ± 26 | 7 | [-15.0-28.6] | 0.1 |
Note: n/m: newton divided by body mass, strength is expressed as kilo
Table 2: Baseline and follow-up outcomes are presented.
Thigh circumference, functional performance and muscle strength tests
No change was demonstrated for thigh circumference on the affected limb nor the non-affected limb with low-to-moderate effect size as shown in Table 2. The participants demonstrated a significant improvement in both TUG and 30 s CST from baseline to follow-up with moderate-to-large effect sizes as shown in Table 2. Also, a significant improvement in knee MVC on the affected limb was found with a high effect size, while no change was found in knee MVC in the non-affected limb as shown in Table 2. Two participants performed both baseline and follow-up 5 RM testing on the affected limb and demonstrated a significant improvement from baseline to follow-up was with a small effect size as shown in Table 2.
Only five patients volunteered to perform pre and post-testing of the knee extensor muscle strength (MVC knee) and only two patients were able to perform both baseline and follow-up assessment of the 5 RM leg press strength without stopping prematurely due to fear of pain exacerbation as show in Table 2.
The main finding of this study was that LL-BFRE seemed viable in a clinical setting in patients suffering from persistent knee symptoms due to various orthopedic knee disorders despite engaging in several previous rehabilitation efforts. However, 4 of 12 patients dropped out, while several patients were unable to perform all follow-up assessment. Thus, choosing the appropriate testing methods, especially mechanical muscle strength evaluation, may require cautious consideration. Only one patient dropped out due to protocol-related issues (knee exacerbation after baseline testing), while none of the patients dropped out due to exacerbation of knee symptoms due to the exercise protocol. Furthermore, the mean adherence rate was on average 95.6% for the eight participants who completed their intended exercise period, resulting in similar adherence to training as previously reported by Ferraz et al. [27] and Segal et al. [28] in patients with knee OA engaging in LL-BFRE exercise protocols.
Mechanical muscle function was evaluated as maximal isometric contraction strength and dynamic 5 RM leg press-strength. As only two subjects were able to perform the 5 RM leg press followassessment, this test may seem contraindicated for patients suffering from persistent knee symptoms despite several previous rehabilitation efforts. Alternatively, decreasing the load to perform a 10 RM test might be more appropriate. That is, Hughes et al. [14] tested 10 RM leg press strength in patients who had received ACL-R with excellent adherence to both exercise as well as testing procedures. Thus, decreasing the load to perform more repetition to concentric contraction failure may be recommended to test dynamic leg press strength in these particular. Also, only 5 participants performed MVC KE at both baseline and follow-up testing, which may question if evaluation of isometric knee extension strength by hand held dynamometry was appropriate in these patients. However, compared to the evaluation of 5 RM leg press strength, our results suggested that MVC KE is more relevant to perform in these patients. The low adherence to both KVC KE and 5 RM leg press strength may reflect the severity of knee pain and symptoms in these patients who prior to participating in the present study had engaged in several unsuccessful rehabilitation efforts This may also be indicated in the KOOS pain and symptoms baseline scores which is far below reference values from a population-based Swedish cohort ranging from 18-84 years of age [21].
A change of +8 points was seen in three subscales (“pain”, “symptoms”, and “sport and recreation”), with all reporting a large effect size. In addition, the minimal important change is considered to be 8-10 points in each KOOS subscale [22], suggesting a meaningful change from baseline to follow-up. This is in line with Ferraz et al. [11] who demonstrated significant changes in patientreported outcomes (WOMAC pain, stiffness and Physical activity) after 12 weeks of LL-BFRE. Furthermore, MVC knee extensor strength increased for the affected lower-limb with a large effect size, while no significant change was seen for the non-affected limb. This might suggest that i) LL-BFRE protocol performed to volitional failure amplified the strength gains compared to the work-matched protocol performed on the non-affected limb or ii) that a workmatched load between an affected (i.e. detrained) limb and a nonaffected (i.e. healthy) limb is insufficient to increase strength in the patients included in this particular cohort study. Also, functional performance assessed by 30-sec CST and TUG tests improved significantly, with moderate-to-large effect sizes. This is in line with both Ferraz et al [27] and Ozaki et al [29] who demonstrated improved 30-sec CST-performance in patients suffering from knee OA after 12 weeks of (36 sessions) LL-BFRE and a faster TUG performance in old adults after 10 weeks of BFR walk training (4/ weekly) [29]. Thus, our results, combined with findings from other studies utilizing BFR exercise methods, indicate that functional performance can be improved with a minimal mechanical stress on the musculoskeletal system.
Strengths and limitations
This study contained several limitations that requires attention. First, the study was largely limited by the heterogeneous group of patients, limiting the generalizability of results from the present study. However, the purpose of this study was to gain experience and knowledge on how to apply LL-BFRE in a hospital setting in patients with persistent knee symptoms despite engaging in several previous rehabilitation efforts. Thus, the variability in patients was considered acceptable as long as patients fulfilled the in- and exclusion criteria.
The lack of a control group as well as the small sample size is considerable limitations to the present study. The small sample size resulted in insufficient statistical power to detect changes while the lack of a control group disabled us to conclude if changes directly reflected the efficacy of LL-BFRE. Also, the low number of participants willing and/or able to perform all follow-up assessment is a major limitation to the present study. Therefore, based on the experiences and results of the present study future studies ought to be careful when evaluating, in particular, mechanical muscle function in similar patient populations.
Despite being a pilot study, aiming at investigating the feasibility of LL-BFRE, we did not predetermine an acceptable adherence before starting the pilot project, hence, limiting our interpretation of the adherence. However, when comparing the adherence rate to other LL-BFRE studies [27,28], it seems that the patients who completed the exercise protocol exhibited a high adherence to LLBFRE. Furthermore, none of the participants dropped out due to exacerbation of symptoms or pain due to the exercise protocol.
Two different protocols were tested resulting in some variations in the total amount of work performed by the patients. This methodological limitation was applied to gain experience with whether patient required to slowly progress the work-load or were able to start the exercise period with a higher work-load. Apparently, no difference in adherence nor feedback from the patients favored protocol 1 from protocol 2. Also, all patients performed the exercise to failure, making the endpoint for each protocol identical (i.e. maximal motor unit recruitment and fatigue).
A strength of the present study was that all patients trained with an individualized restrictive pressure, hence increasing the safety and unifying the exercise stimulus to all participants.
Assessment of pain exacerbation during training was not included in this study. Thus, the amount of knee discomfort during training remains unknown. We did, however, not register any dropouts due to LL-BFRE-related pain aggravation which suggests that LL-BFRE was tolerable for patients involved in this project. At baseline, seven patients were able to perform the 5 RM test while only two patients performed the test at follow-up. This might reflect a fear of pain aggravation and suggest that the patients included in the present study may not have been able to perform HRST.
Clinical application
The present study demonstrated that a single supervised LLBFRE can be applied to patients suffering from persistent knee pain despite engaging in several previous rehabilitation efforts. Furthermore, the study suggested that researchers and clinicians must carefully consider the test methods used as these patients can experience difficulties with performing lower limb muscle strength testing.
This pilot study indicates that supervised LL-BRF is feasible in patients with persistent knee symptoms due to various orthopedic knee disorders despite engaging in several previous rehabilitation efforts. However, a relatively high number of patients did not perform all follow-up assessments, suggesting that the assessment methods was at least to some degree, inappropriate for this particular patient population. Improvements in KOOS subscales, muscle strength and functional performance was demonstrated with moderate-to-large effect sizes. Due to the low number of participants and study limitations the results of the present study require confirmation in a homogenous population in a wellpowered future randomized controlled trial.
The authors would like to acknowledge The Department of Occupational and Physical Therapy and Department of Orthopedic Surgery at Horsens Regional Hospital for their committed involvement in recruiting participants into the study.
The authors reports no competing interests.
No funding received.
All authors contributes to the initial concept of the study, and SLJ recruited and enrolled patients and managed data collection. All authors performed the analysis and interpreted the findings. All authors contributed to the revision of the manuscript an approved the final version.
Ethics approval and consent to participate
Ethical approval was obtained from the Central Denmark Region Committee on Biomedical Research Ethics (journal number 1-10-72-166-18). A written informed consent was obtained before enrolment of participants, and the rights of participants were protected.
Consent for publication
All authors consent to the publication of this study into BMC Rheumatology.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interests
The Authors have no conflicts of interest.
Authors' contribution
Concept/idea/research design: all authors.
Trial registration
Danish Data Protection Agency (Journal No 1-16-02-90-18).
Participants
The study was conducted at the Department of Physical and Occupational Therapy, and the Department of Orthopedic Surgery, Horsens Regional Hospital (HRH), Denmark.
The study was conducted in accordance with the Declaration of Helsinki, and ethical approval was obtained from the Central Denmark Region Committee on Biomedical Research Ethics (journal number 1-10-72-166-18). Approval from the Danish Data Protection Agency (Journal number 1-16-02-90-18) was obtained and all patients gave written informed consent prior to inclusion.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Jorgensen SL, Bohn MB (2023) Blood Flow Restricted Low-Load Resistance Exercise in Patients with Persistent Knee Symptoms despite Previous Rehabilitation Efforts: A Pilot Study. Rheumatology (Sunnyvale). 13: 352
Received: 01-Apr-2023, Manuscript No. RCR-23-22756; Editor assigned: 04-Apr-2023, Pre QC No. RCR-23-22756 (PQ); Reviewed: 19-Apr-2023, QC No. RCR-23-22756; Revised: 26-Apr-2023, Manuscript No. RCR-23-22756 (R); Published: 03-May-2023 , DOI: 10.35841/2161-1149.23.13.352
Copyright: © 2023 Jorgensen SL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.