International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2022)
Background: Neuromuscular electrical stimulation is a rehabilitation method currently used among patients with spinal cord injury, but its results are not well defined yet. The objective of this study is to analyze the contribution of rehabilitation with Neuro-Muscular Electrical Stimulation (NMES) assessing Bone Mineral Density (BMD), quality of life aspects and demographic characteristics, after 10 years under treatment.
Methods and findings: Retrospective longitudinal study between 2008 and 2020, at Spinal Cord Injury Outpatient Clinic, University Hospital, with 24 participants with spinal cord injury in rehabilitation with NMES. Identification questionnaire, Functional Independence Measure (FIM) and bone density exam were used for, respectively, demographic analysis, quality of life and BMD. Data from 2008 were catalogued as Pi and current data as Pa. Student’s T-test was used for statistical evaluation, being significantly relevant when p<0.05. Mean age was 45.3 years old, with 22 male individuals; 14 are paraplegic and 10 are tetraplegic; 13 individuals presented injury by traffic accident, 2 by fall from height, 4 by dive, 4 by firearm injury and 1 by tumor; 11 individuals with cervical-level injury and 13 thoracic-level injury, all with complete disability. FIM average Pi=80.2 and average Pa=84 (p=0.36); BMD of vertebrae L1-L4 average Pi=-0.02 and average Pa=-0.17 (p=0.50); BMD of femoral neck average Pi=-2.1 and average Pa=-1.9 (p=0.12); outcomes: 2 osteopenia and 1 osteoporosis for L1-L4; 18 osteopenia and 4 osteoporosis for femoral neck. Limitations of this study include the small sample of individuals and their difficulty to maintain 10-years follow-up treatment.
Conclusion: Demographic characteristics were compatible to literature, except for the age. FIM score and BMD remained similar to the beginning of treatment with NMES, concluding that there was stabilization of these parameters during treatment.
Spinal cord injury; Bone mineral density; Functional independence measure; Neuromuscular electrical stimulation
People with spinal cord injury present motor, sensitive and autonomic disabilities [1]. In addition to the neurological loss, they could have problems related to self-esteem, loss of functional independence and social isolation. The costs to the national health system and to the government provident funds with diagnosis, treatment, recovery and rehabilitation are high. Spinal cord trauma worldwide incidence is about 10–60 cases per million inhabitants depending on the country [2,3]. In Brazil, the incidence is estimated in around six to eight thousand new cases per year, 80% of which are male. Moreover, 60% of the victims are aged between 10 to 30 years old [1]. Traumatic origin is the most prevalent cause of spinal cord injury according to the literature. Studies done in rehabilitation centers show that traffic accidents are the leading cause of trauma, followed by gunshot wounds. The non-traumatic mechanisms, around 20% of spinal cord injuries cases, comprise infections, tumor growth, metastasis, herniated disc, autoimmune diseases and other etiologies [1].
Reduction in Bone Mineral Density (BMD) is significant in spinal cord injured people, with osteoporosis being a recurrent complication [4-6], These individuals are known to be the population parcel who suffers the most with loss of bone mass, about 1% per week, in specific regions of the body, in the first months after injury [4,7].
Neuromuscular electrical stimulation (NMES) is a rehabilitation strategy used in spinal cord injury [8], which allows individuals to remain in the orthostatic position, also enabling movements, reducing contractures, spasticity, osteoporosis and deformities. There is an improvement in energy efficiency, which increases self-performance aiming to execute activities of daily living [9], what can be quantified by Functional Independence Measure (FIM). The present study aims to analyze the contribution of rehabilitation with Neuromuscular Electrical Stimulation (NMES) assessing Bone Mineral Density (BMD), quality of life aspects and demographic characteristics, after 10 years under treatment. We hypothesized that there is alteration in BMD of spinal cord injured patients with NMES rehabilitation over the years.
Retrospective longitudinal study carried out between January 2008 and January 2020, approved by the research ethics committee of the School of Medical Sciences of Unicamp (Certificate of Presentation for Ethical Consideration: 26667819.7.0000.5404; date of approval: April 17 2020), in accordance with the Helsinki Declaration. The research participants have the guarantee of anonymity preserved (Resolution CNS 466/2012). All experiments were performed in accordance with relevant guidelines and regulations. Participants have given their informed consent for participation in the research study.
Data were collected through questionnaires and medical records completed during the period of clinical treatment with NMES. Data from 2008 were catalogued as Pi and current data, after 10 years of evolution, as Pa. The inclusion criteria were: spinal cord injured individuals with intact lower motor neuron, minimum injury time of 1 year and beginning in rehabilitation programme.
Twenty four individuals from Spinal Cord Injury Outpatient Clinic at Unicamp were treated with NMES associated with a partial weight support system which supports bipedal gait through the use of walkers for paraplegia or suspension equipment for tetraplegia, both allowing for free movements of hip and knee joints [10] (Figures 1 and 2).
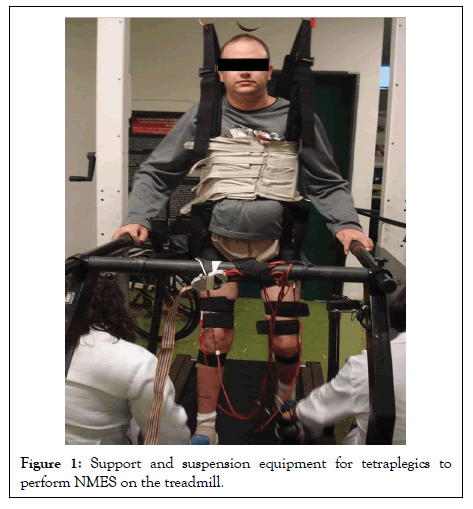
Figure 1: Support and suspension equipment for tetraplegics to perform NMES on the treadmill.
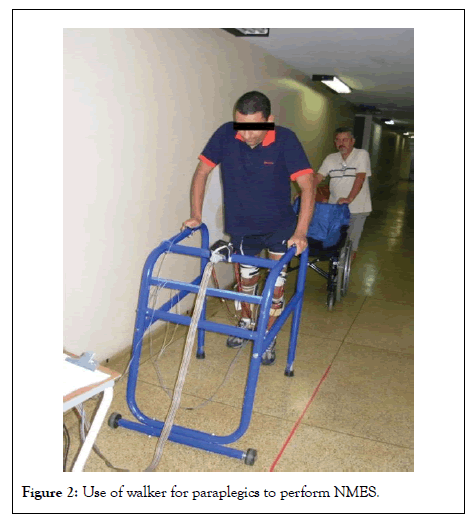
Figure 2: Use of walker for paraplegics to perform NMES.
The feet and ankle joints were protected with ankle-foot orthosis. The quadriceps and tibialis anterior muscles are stimulated towards gait. The stimulator uses four channels yielding a signal of 25 Hz with monophasic rectangular pulses of 300 microseconds at a maximum intensity of 150V (1 kilo Ohm load) along two weekly sessions lasting 20-30 minutes each.
Individuals were investigated about their demographic characteristics (age, sex, injury level, trauma mechanism), ASIA Impairment Scale [11], FIM and bone density.
Bone density and functional independence measure data were compared at the beginning and throughout the rehabilitation period. Demographic characteristics were outlined between January 2020 and March 2020.
The BMD was assessed through bone density exam of the lumbar spine and femoral neck using the dual-energy X-ray absorptiometry method (Luna DPX-Luna Radiation Corporation, Madson, WI). Results were analyzed comparing the standard deviation (SD) of young adult reference ranges (T-Score) [12]: up to-1.0 SD=normal; from-1 to-2.5 SD=osteopenia and; below-2.5 SD=osteoporosis.
Student’s T-test was used for statistical evaluation among the groups and significant differences between the results when p<0.05.
BMD assessment for L1-L4 vertebrae resulted in Pi with an average of-0.02 (varying from-2.1 to 3.5) and Pa with an average of-0.17 (varying from-2.6 to 4.4), where p was 0.50, not having, thus, statistically differences between the paired samples. The analysis of the 24 bone density exams of the femoral neck had Pi with an average of-2.1 (varying from-4.4 to-0.1) and Pa with an average of-1.9 (varying from-4.2 to-0.9), where p was 0.12, not having statistically difference between the paired samples. The analysis of subjects’ individual SD, in most recent bone density exams (Pa), resulted in the following classification: 21 individuals as normal, two as osteopenia and one as osteoporosis for lumbar spine; two individuals as normal, 18 as osteopenia and four as osteoporosis for femoral neck (Table 1).
| Patient | Age | Sex | Plegia | Mechanism Of trauma | Lumbar spine | Femoral neck |
|---|---|---|---|---|---|---|
| 1 | 50 | F | P | fall from height | normal | osteopenia |
| 2 | 73 | M | P | tumor | normal | osteopenia |
| 3 | 45 | M | P | traffic accident | normal | osteopenia |
| 4 | 53 | M | T | traffic accident | normal | osteopenia |
| 5 | 40 | M | P | traffic accident | normal | osteopenia |
| 6 | 44 | M | P | firearm injury | nomal | osteopenia |
| 7 | 37 | M | P | traffic accident | normal | osteopenia |
| 8 | 35 | M | T | traffic accident | normal | normal |
| 9 | 43 | M | T | traffic accident | normal | osteopenia |
| 10 | 33 | M | T | dive | osteoporosis | osteoporosis |
| 11 | 38 | M | P | firearm injury | normal | normal |
| 12 | 68 | M | P | fall from height | normal | osteopenia |
| 13 | 48 | M | P | traffic accident | normal | osteopenia |
| 14 | 50 | M | T | dive | normal | osteopenia |
| 15 | 40 | M | P | firearm injury | normal | osteopenia |
| 16 | 40 | M | P | traffic accident | osteopenia | osteopenia |
| 17 | 48 | M | T | traffic accident | normal | osteopenia |
| 18 | 55 | M | T | traffic accident | osteopenia | osteoporosis |
| 19 | 32 | M | P | traffic accident | normal | osteopenia |
| 20 | 30 | M | T | dive | normal | osteoporosis |
| 21 | 50 | M | P | traffic accident | normal | osteopenia |
| 22 | 52 | F | P | traffic accident | normal | osteopenia |
| 23 | 31 | M | T | dive | normal | osteoporosis |
| 24 | 53 | M | T | firearm injury | normal | osteopenia |
Note: F-female; M-male; P-paraplegic; T-tetraplegic
Table 1: Demographic characteristics of patients.
The demographic analysis showed the mean age obtained for 24 individuals was 45.3 years old (varying from 31 to 73), with 22 male and two female individuals (14 people with paraplegia and 10 with tetraplegia). In relation to the mechanism of trauma, 13 individuals presented injury by traffic accidents (motorcycle or automobile accident or being run over), 2 by fall from height, 4 by dive in shallow water, 4 by firearm injury and 1 by bone tumor Table 1. The average time of injury was 14.8 years (varying from seven to 25 years).
ASIA Impairment Scale classified individuals as follows: four C4A, four C5A, one C6A, two C7A, one T1A, one T3A, two T4A, two T5A, four T6A, two T8A and one T9A.
Regarding the evolution of treatment over 10 years, those individuals analyzed by FIM obtained Pi with an average of 80.2 (varying from 25 to 124) and Pa with an average of 84 (varying from 66 to 106), with p being 0.36, without existing statistically differences between the paired samples.
Brazilian epidemiological profile of spinal cord trauma has male individuals aged between 10 and 30 years old as the injury predominance [1]. The profile observed in this study matches male prevalence, although differing about the age of spinal cord injured individuals which varies from 31 to 73 years old (average of 45.3 years old).
Trauma is the main cause of spinal cord injury, with the principal etiologies being automobile accident, firearm injury and falls [1]. In this study, the 13 injuries by traffic accident, two by fall from height and four by firearm are compatible with the literature. Other mechanisms of trauma are also involved, such as four injuries by dive in shallow water and one bone tumor.
Studies show that spinal cord injury is associated with higher prevalence of cervical-level injury [13-17]. However, the present study differs from those, presenting 13 individuals (54%) with thoracic-level injury and 11 (44%) with cervical-level injury.
The literature points out that the higher increase of FIM scores occurs in the first years after injury and, after approximately five years, the scores stabilizes, existing little improvement in independence level, because it is understood that the maximum level of independence was obtained according to the level injury [18]. Data obtained from the study agree with literature, because there was stabilization of the scores of most individuals.
Regarding bone mass quality, in this study, it was found 79% of osteopenia prevalence and 21% of osteoporosis, on any of the structures analyzed (lumbar spine and femoral neck). These data illustrate how much this population is affected by high degrees of bone loss. Some studies point out that these individuals lose up to 50% of bone density in the first year of injury, which tends to stabilize after the second year [4].
Although the pathophysiological mechanisms of this process are not yet totally elucidated, sublesionals central and peripheral neural denervations seem to have strong influence on bone mass loss, once they act on osteoanabolic metabolism [4]. Other possible mechanisms which may be responsible for this event include the gravity change due to immobilization, the loss of anabolic factors (for example, testosterone and/or circulating growth hormones), the factors in bone local environment (paracrine influences of muscle atrophy) and the presence of catabolic factors at the time of injury (such as administration of high doses of methylprednisolone within a few hours after the acute and/or systemic event and/or the local production of inflammatory mediators or cytokines) [4].
In this study, it was also evidenced that femur is the most affected region by bone loss, with the prevalence of osteopenia approximately 75% and of osteoporosis 17% for femoral neck; and 8% of osteopenia and 4% of osteoporosis for lumbar spine.
In the study of Sabo et al. [19], the authors also found BMD reduced in proximal femur, but not in lumbar spine. This is justified because, in order to avoid bone loss, it is necessary to have normal muscular function and load, variables practically absent in the femur and partially present in the lumbar spine, which supports the load of individual’s body while using the wheelchair [20].
In relation to the effects of NMES treatment on bone density of spinal cord injured individuals, literature does not show a consensus. Studies that investigated its effects on bone are conflicting 21. Several methodological limitations restrict the capability to confirm the utility of this intervention in order to improve the skeletal status [21]. In Forrest et al. [22] the authors observed a decrease of total BMD (1.54%) and regional BMD (legs: 6.72%).
In Giangregorio et al. study [23]. Authors concluded that this intervention is not enough to prevent bone loss, as it was evidenced by BMD reduction for all individuals varying in magnitude from 1.2 to 26.7% for lower limb and 0.2 to 7.4% for lumbar spinal.
On the other hand, in the study carried out by Mohr et al. [24], a 10% increase of BMD for proximal tibia was described, but no difference for femoral neck and spine. In the study of Coupaud et al 13, it was also verified an increase of BMD for distal tibia (5% for right leg and 20% for left leg). However, the results were insignificant for proximal tibia and for the femur. In this study, improvement of BMD of the femoral neck and worsening of BMD of the lumbar spine were found. Even though, data obtained were not statistically significant, preventing us from making statements and comparisons with other studies.
Limitations of this study include the small sample of 24 individuals and their difficulty to maintain 10-years follow-up treatment because of socioeconomic and psychological reasons, functional dependence and comorbidities due to the level of the spinal cord injury. Larger studies should be carried out for better future analysis and adjustments in these factors would help to continue the treatment of these patients.
The demographic profile of patients was compatible to the one found in literature in the characteristics analyzed, except for the age, which is higher among patients in this study. About functional independence measure score and bone mineral density, they remained similar to the beginning of the treatment with neuromuscular electrical stimulation (NMES), concluding that there has been stabilization of these parameters during 10 years of treatment. Our long term results do show that it is feasible to preserve BMD thus avoiding bone fractures, due to disuse osteoporosis in spinal cord injury subjects.
I give permission for images in which I appear to be used by International Journal of Physical Medicine & Rehabilitation for publications and public relations activities. I do not have any objection to upload my pictures in the article entitled "Bone Mineral Density can be kept in Spinal Cord Injured Subjects under Long Term Neuromuscular Electrical Stimulation". In particular, I note that this may include use in print and electronic media, including the Internet and official social media platforms. I have read and understand this notice, and consent to the collection, use and disclosure of my image, including disclosure to overseas recipients, as outlined.
The authors declare that no competing interests exist.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar][Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar][PubMed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar][PubMed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef][Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
Citation: Bittar CK, e Silva RC, Silvestre O, Kimoto EA, de Paula MC, Suguimoto L, et al. (2022) Bone Mineral Density in Spinal Cord Injured Subjects under Long Term Neuromuscular Electrical Stimulation. Int J Phys Med Rehabil.S17:002.
Received: 28-Mar-2022, Manuscript No. JPMR-22-16433; Editor assigned: 30-Mar-2022, Pre QC No. JPMR-22-16433 (PQ); Reviewed: 13-Apr-2022, QC No. JPMR-22-16433; Revised: 20-Apr-2022, Manuscript No. JPMR-22-16433 (R); Published: 29-Apr-2022 , DOI: 10.35248/2329-9096-22.S17.002
Copyright: © 2022 Bittar CK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.