Journal of Osteoporosis and Physical Activity
Open Access
ISSN: 2329-9509
ISSN: 2329-9509
Research - (2024)Volume 12, Issue 5
The appearance of an osteoporotic fracture, also called fragility fracture, is the most serious consequence of osteoporosis due to its clinical implications that lead to functional decline, chronic pain, disability, decreased quality of life, as well as increased morbidity and mortality. A retrospective observational study was conducted in patients over 50 years of age who had suffered at least one fragility fracture at humerus, distal forearm, vertebra, pelvis or hip during a 2-year period in Aragon, Northern region of Spain. A total of 11,986 patients with osteoporotic fracture were obtained, accounting for a crude incidence of 13.29/1,000 inhabitants-year. Most of them were women (75.63%), compared to men (24.37%). A gradual increase in the number of fractures was observed with advancing age, increasing up to 51.84% of the total number of osteoporotic fractures in the group over 80 years of age. Most frequent skeletal site was hip with 30.08%, followed by distal forearm (25.12%), proximal humerus (20.02%) and vertebral (11.34%). Osteoporotic fractures have a high incidence in the population of Aragon, particularly in older women. The data presented will be useful for healthcare and economic planning in the coming years. These fractures entail a high healthcare uptake as well as a substantial impact on healthcare budget, especially in the case of hip fracture. It is essential that secondary prevention measures for osteoporotic fractures, such as Fracture Liaison Services (FLS), are implemented by public health systems.
Osteoporotic fracture-incidence-social; Economic burden-Spain; Fragility fracture; Bone mineral density
Osteoporosis is a chronic disease characterized by an alteration of bone microarchitecture and a decrease in Bone Mineral Density (BMD) that leads to bone fragility and an increased risk of fracture [1,2]. The appearance of an Osteoporotic Fracture (OF), also called fragility fracture, is the most serious consequence of osteoporosis due to its clinical implications that lead to functional decline, chronic pain, disability, decreased quality of life, as well as increased morbidity and mortality [1,3-7]. Fractures most commonly associated with osteoporosis include those located at the hip, vertebra, distal forearm, proximal humerus, ribs, sternum, pelvis and clavicle [8-10]. A Fragility Fracture (FF) [11], results from a mechanical force that, in a healthy subject, would not ordinarily cause fracture, having been produced by low-energy trauma. The World Health Organization (WHO) has quantified these forces as those equivalent to a fall from a standing height or less, or those minor traumas not caused by a fall [12]. According to the International Osteoporosis Foundation (IOF), in 2017 there were about 330,000 new osteoporotic fractures in Spain, so that, from the age of 50, the risk of suffering a major osteoporotic fracture throughout life (vertebra, hip, humerus and distal forearm) is 20% in women and 18% in men [13]. The progressive aging of the Spanish population will increase the incidence of these fractures with the consequent increase in the social, health and economic burden. It is estimated that in Spain the incidence of fractures will increase by around 28% until 2030, which will entail an increase in associated costs of 30% [5,8]. Several studies [1,14-17], have been published on the incidence and epidemiology of osteoporotic hip fractures, but the incidence of osteoporotic fracture in Spain that usually does not require hospitalization has been scarcely published [18,19], due to the scarcity of reliable data. The aim of this study is to determine the incidence of osteoporotic fractures in Aragon, as well as the social and health burden caused in a Spanish region with a very aged population, and to describe the profile of patients with osteoporotic fractures.
A retrospective observational study was conducted in patients over 50 years of age who had suffered at least one first FF during the period from January 1, 2014 to December 31, 2015. In order to consider the fracture suffered as a first recent fracture, patients who had suffered a FF in 4 years prior to the current fracture were excluded. Data were collected from patients diagnosed with fracture using diagnostic codes according to International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-MC) at the skeletal sites of shoulder and humerus (810,811,812), forearm/ wrist (813), vertebra (805,806), pelvis (808), proximal femur and hip (820,821), ribs and/or sternum (807), tibia/fibula, and ankle (823,824). To identify patients with fractures, data were collected from the Big Data Network (BIGAN) clinical management platform of the Aragonese Health Service, a database that records all episodes of patients who attend the emergency services of all hospitals in the public health network of Aragon. For the present study, data were obtained on age, gender, skeletal site of the fracture, seasonality of the event, geographical area where the patient comes from (rural or urban), morbidity with most relevant risk factors that increase the risk of fracture (dementia, rheumatoid arthritis, diabetes mellitus, osteogenesis imperfecta, hypogonadism, chronic renal failure, current use of steroids) and previous or current anti-osteoporotic treatment during the 2 years prior to osteoporotic fracture (zoledronate, alendronate, risedronate, ibandronate, teriparatide, denosumab, raloxifene, and bazedoxifene).
Population data for the study period were obtained from the National Statistics Institute (INE, ww w.ine.es/), official public institution that collects demographic, economic and social statistics. For the statistical analysis, the frequency distribution (absolute and relative) of the qualitative variables studied was calculated. The crude incidence rates stratified by gender and age were calculated, dividing the number of fractures in each year by the Aragonese population according to data provided by the INE for the same study period. The incidence rates were expressed per 100,000 inhabitants/year. This study was approved by the Aragon Clinical Research Ethics Committee (CEICA) of the Government of Aragon on 04/07/2021 and was carried out in accordance with the standards set out in the Declaration of Helsinki. Due to the nature of the study, informed consent was not necessary since the data from the BiGAN clinical management platform of the Aragonese Health Service were purely observational.
A total of 12,967 patients with fracture were obtained, of which, 981 patients with FF in the previous 4 years were excluded to comply with the concept of first fracture (sustained a prior fracture during the previous 4 years (2010-2013), to meet the first index fracture criterion. This resulted in a population sample of 11,986 patients, in the two-year period of data collection. The crude incidence of osteoporotic fracture in the study period was 6,483/ year (13.29/1,000 inhabitants-year).
Distribution by age and gender
A total of 9,065 patients with FF in our study were women (75.63%), compared to 2,921 men (24.37%), with a predominance of FF in female patients (Table 1). Furthermore, a gradual increase in the number of fractures was observed with advancing age, increasing up to 51.84% of the total number of osteoporotic fractures in the group over 80 years of age, compared with the younger patients in our study (between 50-59 years of age) in whom 1,284 fractures occurred (10.71%) (Table 1).
| Population | n=11,986 | Percentage |
|---|---|---|
| Gender | ||
| Man | 2,921 | 24.37% |
| Women | 9,065 | 75.63% |
| Age range | ||
| >80 | 6,214 | 51.84% |
| 70-79 | 2,655 | 22.15% |
| 60-69 | 1,833 | 15.29% |
| 50-59 | 1,284 | 10.71% |
Table 1: Population sample under study, according to age and gender.
Skeletal fracture site
In our series, fracture data were collected at different skeletal sites: Distal forearm/wrist, hip, proximal humerus, vertebra and the rest of the sites grouped under the heading of "other sites" (due to their lower frequency of presentation). Most frequent skeletal site was hip with 30.08%, followed by distal forearm (25.12%), proximal humerus (20.02%) and vertebral (11.34%). When analyzing the relationship between the different skeletal sites and the age of the patients, it can be observed that there was a higher frequency of hip fracture in those patients over 80 years of age (78.84%), progressively decreasing in the younger groups to a scant 2.02% in the 50-59 age group. In the case of vertebral fractures, it was observed in 44.63% in patients over 80 years of age compared to 9.49% in patients between 50-59 years of age. In the case of distal forearm fractures, a more homogeneous distribution was observed between the different age groups, although with a higher frequency of appearance in younger patients (50-69 years), compared with other skeletal sites (Table 2). The average crude incidence rate of hip fracture in people over 50 years of age was 405.4 per 100,000 inhabitants/year, according to population data from the INE for the study period. For vertebral fractures, the rate was 151.59 per 100,000 inhabitants/year; for humerus fractures it was 264.79 per 100,000 inhabitants/year; and for distal forearm/wrist fractures it was 327.16 per 100,000 inhabitants/year. A progressive increase in the incidence of fractures at all sites was observed with advancing age, especially in the case of the hip (Figure 1). As previously described, there was a predominance of osteoporotic fracture in women in the sample studied. Similarly, this observation was confirmed in all skeletal sites of osteoporotic fracture, especially in the case of the distal forearm (with 84.33% in women compared to 15.67% in men) and the hip (72.02% versus 27.98%) (Table 3). If we take into account INE database as a reference to calculate the incidence per 100,000 inhabitants of each site according to gender (Figure 2), it can also be seen that the incidence of osteoporotic fracture regardless of the skeletal site is more frequent in women compared to men, especially in distal forearm fractures.
| Age group | Distal forearm | Hip | Proximal humerus | Vertebra | Other sites |
|---|---|---|---|---|---|
| >80 | 974 (32.34%) | 2843 (78.84%) | 982 (40.92%) | 607 (44.63%) | 808 (50.25%) |
| 70-79 | 779 (25.86%) | 513 (14.23%) | 646 (26.92%) | 393 (28.90%) | 324 (20.15%) |
| 60-69 | 706 (23.44%) | 177 (4.91%) | 445 (18.54%) | 231 (16.99%) | 274 (17.04%) |
| 50-59 | 553 (18.36%) | 73 (2.02%) | 327 (13.63%) | 129 (9.49%) | 202 (12.56%) |
Table 2: Distribution of skeletal fracture site by age groups.
| Gender | Distal forearm | Hip | Proximal humerus | Vertebra | Other sites |
|---|---|---|---|---|---|
| Male | 472 (-15.67%) |
1,009 (27.98%) | 683 (-28.46%) |
410 (-30.15%) |
347 (-21.58%) |
| Female | 2,540 (84.33%) | 2,597 (72.02%) | 1,717 (71.54%) | 950 (-69.85%) |
1,261 (78.42%) |
Table 3: Distribution of skeletal fracture site by gender.
Figure 1: Age-specific incidence rates by skeletal fracture site (per 100,000 inhabitants).
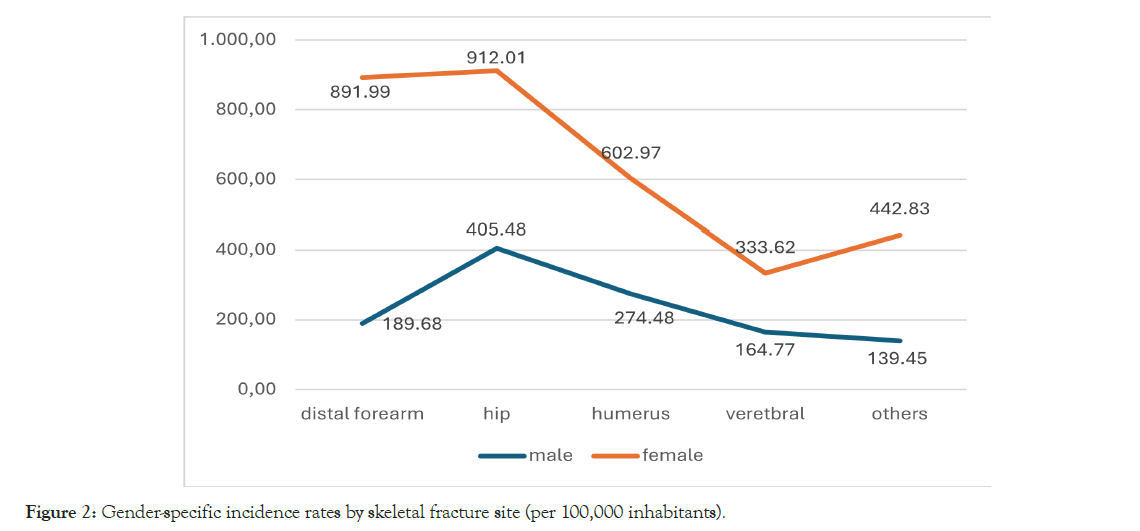
Figure 2: Gender-specific incidence rates by skeletal fracture site (per 100,000 inhabitants).
Home environment and fracture seasonality
Regarding home environment of our patients, it was observed that almost two thirds of the patients lived in an urban area (65.45%). With regard to seasonality of the fracture, no significant differences were found among four seasons, with figures close to 25% in each of them (Table 4).
| Environment | n | Percentage |
|---|---|---|
| Rural | 4,141 | 34.55% |
| Urban | 7,845 | 65.45% |
| Seasonality | ||
| Winter | 2,936 | 24.50% |
| Autumn | 2,993 | 24.97% |
| Spring | 3,031 | 25.29% |
| Summer | 3,026 | 25.25% |
Table 4: Fragility fracture according to environment and seasonality of the event.
Predisposing factors
More than one third of fractured patients (38.3%) presented predisposing risk factors (29.91% presented only one factor, while the remaining 8.39% had more than one concomitant factor), such as diabetes mellitus (20.24%), dementia (10.92%), chronic renal failure (9.36%), current use of steroids (3.85%), rheumatoid arthritis (2.58%), and hypogonadism (1.82%) (Table 5). Finally, only 1,420 patients (11.85%) had taken some type of antiosteoporotic medication in the last 2 years prior to the fracture. The most frequently used drug was alendronate with 33.59%, followed by denosumab (12.53%) and teriparatide (5.8%).
| Predisposing factors | Percentage of patients |
|---|---|
| Diabetes mellitus | 20.24% |
| Chronic renal failure | 9.36% |
| Rheumatoid arthritis | 2.58% |
| Dementia | 10.92% |
| Steroids | 3.85% |
| Hypogonadism | 1.82% |
Table 5: Percentages of patients with predisposing factors.
This study presents data on the incidence of osteoporotic fractures in various skeletal sites for men and women over 50 years of age in a Northern region of Spain. The data show a higher incidence in women, as well as a progressive increase in the incidence of osteoporotic fracture related to the increase in the age of patients, especially in those patients over 80 years of age. This difference has been shown to be due, in part, to differences in BMD and bone architecture as well as to the estrogen deficiency that occurs in women after menopause [20,21]. The overall incidence of osteoporotic fracture in the Aragonese population over 50 years of age was 13.29/1,000 inhabitants-year, a similar figure to that published in the Scorecard for Osteoporosis in Europe 2021 (SCOPE´21) report for Spain globally in the year 2019 (14.8/1,000 inhabitants-year) [22]. In the case of hip fracture, the incidence in people over 65 years of age was 687/100,000 inhabitants-year, showing a significant difference according to gender (877/100,000 inhabitants-year in women and 441/100,000 inhabitants-year in men). These figures show an increased incidence for hip fractures compared with those published in a previous report [15], for the period 2000-2002. This increase in the incidence figures could be related to the higher ageing index of the autonomous community of Aragon (137.7) compared with the national average (113.66) during the study period, according to INE data. It is worth highlighting the high incidence of these fractures in women over 60 years of age. Age is a determining factor in the production of fractures since more than half of the osteoporotic fracture (51.8%) occur in people over 80 years of age and in the case of hip osteoporotic fracture, more than 78% occur in this age group. In relation to the skeletal site of the fractures, 30% of fractures in our series occurred at the hip, a significant higher percentage compared to other reports of around 19%-22% [8,13]. There is progressive increase in osteoporotic fractures in all skeletal sites as age increases, and, in fact, more than 93% of hip osteoporotic fractures occurred in patients over 70 years of age, as described in other previous studies [23,24].
In contrast, wrist fractures show a higher frequency in younger population groups (50-69 years) compared to other skeletal sites in these age groups. Various studies have shown that, after a first osteoporotic fracture, the risk of suffering successive future fractures increases, so the distal forearm/wrist fracture is revealed as a sentinel fracture that should be considered as an indicator of future fractures as the age of the patients increases [25,26]. Hence, the importance of treating these fractures with antiosteoporotic therapy as a fundamental tool for secondary prevention of osteoporotic fracture. A higher frequency of osteoporotic fracture was detected in the urban population compared to the rural population. This could be due to the higher percentage of urban population compared to the rural population in the region or, as some studies have suggested, perhaps because in rural areas, population develops greater physical activity and, consequently, greater muscle mass, which would reduce the risk of osteoporosis, the number of falls and, therefore, osteoporotic fractures, although none of these extremes could be studied due to the lack of reliable data [27,28]. No significant difference was found in the seasonality of the fracture and, therefore, there does not seem to be a relationship with the more adverse weather conditions of autumn- winter, which are assumed to be more prone to the production of traumatic events. The fact that a majority of osteoporotic fractures occur at an advanced age with less mobility may result in the fact that most of the events have occurred inside homes, therefore, unrelated to the external weather conditions.
In a recent report by the IOF [13], fragility fractures were the fourth leading cause of chronic disease morbidity and disability, higher than other diseases such as chronic obstructive pulmonary disease, ischemic stroke, migraine, hypertensive heart disease or asthma. However, the majority of countries reporting information on National Health Priorities (NHP) does not recognize osteoporosis or musculoskeletal diseases as an NHP [8]. With progressive ageing of the population (ageing index in 2023 for Spain of 137.33 and Aragon of 154.28, according to INE data), it is foreseeable that the absolute number of osteoporotic fracture will increase in parallel in the coming years (around 30% by 2034, according to the SCOPE-21 study) [22], contributing to a greater demand for healthcare services and an increase in social and economic costs. Therefore, unless osteoporosis prevention and treatment become a priority for healthcare providers, the growing number of osteoporotic fracture will have a serious impact on society in terms of people’s quality of life as well as increased costs sustained for acute healthcare, rehabilitation and nursing care.
In order to reduce the future incidence of osteoporotic fracture, various measures have been implemented within public health systems: Harmonization of clinical practice guidelines, training of professionals on the treatment of osteoporotic fracture, social awareness campaigns on osteoporosis and fractures, as well as the creation of multidisciplinary units for the secondary prevention of osteoporotic fractures, known as FLS [29]. Setting up secondary prevention units for osteoporotic fracture has proven to be the most effective and cost-effective of all the above initiatives [30,31]. This study has also some limitations. First, it is a retrospective study in which data on fracture diagnosis and comorbidities were collected from a database, which could contain coding errors that could not be detected. Second, it is likely that there was an underestimation of the number of fractures, since other skeletal sites were not considered in the study, neither were periprosthetic femoral fractures considered (whose frequency has increased in recent years as a result of the increase in hip and knee prosthetic replacements in older population). In addition, no data could be obtained for fractures treated in private hospitals, although they represent a minimal percentage compared to public hospitals. Finally, only data on clinical vertebral fractures were collected: It is known that these only represent a third of all vertebral osteoporotic fractures (most are asymptomatic) [32].
This study presents for the first time data on the incidence of osteoporotic fractures in a Northern region of Spain in most frequent skeletal sites. From the analysis carried out, we detected that osteoporotic fractures have a high incidence in the population of Aragon, particularly in older women. The data presented will be useful for healthcare and economic planning in the coming years. In addition to the suffering for patients and their families, the data show that these fractures entail a high healthcare uptake as well as a substantial impact on healthcare budget, causing significant social and economic burden, especially in the case of hip fracture. This burden will increase in the coming years with the progressive ageing of the population, so it is essential that secondary prevention measures for osteoporotic fractures are implemented by public health systems.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]7
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Avino RI, Pazmino PF (2024). Burden of Osteoporotic Fracture in Northern Spain. J Osteopor Phys Act.12:414.
Received: 15-Sep-2024, Manuscript No. JOPA-24-34066; Editor assigned: 18-Feb-2024, Pre QC No. JOPA-24-34066 (PQ); Reviewed: 02-Oct-2024, QC No. JOPA-24-34066; Revised: 09-Oct-2024, Manuscript No. JOPA-24-34066 (R); Published: 16-Oct-2024 , DOI: 10.35248/2329-9509.24.12.414
Copyright: © 2024 Izquierdo-Avino R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.