Journal of Hepatology and Gastrointestinal disorders
Open Access
ISSN: 2475-3181
ISSN: 2475-3181
Review Article - (2022)Volume 8, Issue 1
Burning Mouth Syndrome (BMS) is a chronic, debilitating orofacial pain syndrome causing burning or scalding sensation in the mouth. This disease primarily affects middle-aged and older women who are experiencing hormonal or psychological changes. Most commonly, the affected site is anterior 2/3rd of the tongue. This disease is most likely multifactorial in nature, is typically idiopathic and the exact etiopathogenesis remains unknown. Psychological disorders such as stress, depression and anxiety play a demonstrable role in burning mouth syndrome. High rate of occurrence in post-menopausal women strongly suggest a link to hormonal changes. Patients with BMS also experience oral mucosal discomfort, changed taste sensations, and dry mouth in addition to the burning sensation. So far, there is no standardized treatment for this condition, but a proposed combination of supportive care and medications are recommended. Benzodiazepines are used as first line drug in pharmacological treatment of BMS. Non-Pharmacological treatment includes cognitive behavioural therapy, group psychology, yoga, and meditation etc. The purpose of this review is to acquaint healthcare practitioners with the epidemiology, aetiology, classification, basic features, psychological dysfunction and medical conditions associated with BMS, as well as keeping them informed about current therapy choices, in order to effectively manage this patient population.
Burning mouth syndrome; Dysesthesia; Epidemiology; Glossodynia; Psychological dysfunction; Stomatodynia; Xerostomia
The patients who complains of a burning feeling in their mouth displays one of the most challenging tasks for oral health specialist. If the disease is accompanied by discomfort or pain, it will worsen much more. Pain is a frequent source of misery and impairment that has a major impact on a person's quality of life. Burning Mouth Syndrome (BMS) can be defined as burning or scalding sensation in the normal oral mucosa.
Some researchers have disputed this definition in recent years, stating that it is overly restrictive and that the illness might coexist with other oral problems too [1]. Furthermore, the exact cause of BMS is still unknown because of its complex etiopathogenesis [2].
Because of the variety of clinical manifestations, there is currently no widely recognised description of this condition. International Association for the Study of Pain has stated this syndrome as "burning pain in the tongue or other oral mucous membrane associated with normal signs and laboratory findings lasting at least 4-6 months" [3].
The global prevalence of burning mouth syndrome is unclear because all studies have been conducted on North American and European populations and various diagnostic criteria have been employed in different investigation [4]. In both men and in women, incidence of burning mouth syndrome increases with age. 60-69 years aged women have highest prevalence [5]. The male-to-female ratio fluctuates between 3:1 and 16:1. Oral burning appears to be most common in postmenopausal women, according to the findings of most research published so far [6]. 10% to 40% of women seeking treatment for menopausal symptoms complain of BMS [7]. These percentages contrast epidemiologic studies that revealed substantially lower prevalence rates of oral burning (0.7 to 2.6 percent) [8]. Stomatodynia, Scalded mouth syndrome, Glossodynia, Burning lips, Stomatopyrosis, Glossopyrosis, Oral dysesthesia, Sore mouth were all terms used in the past to describe this ailment. Burning Mouth Syndrome (BMS) is most widely accepted term used in current practice. This condition is mostly affect anterior 2/3rd of the tongue and patient complains of dry mouth and altered taste sensations.
Assessment of patient (categorization)
BMS was categorised into three categories by Lamey and Lewis in 1989 depending on pain severity [9].
Type 1: Patients with type 1(35%) experience burning on a daily basis. The burning is absent when you wake up, but it becomes more noticeable throughout the day, peaking in the evening. Systemic diseases, such as dietary deficits and endocrine abnormalities, are linked to this type.
Type 2: Patients with type 2(55%) is distinguished by burning that occurs on a daily basis. It is present on awakening, but falling asleep at night becomes difficult. Sudden change of mood, changes in dietary habits, altered sleep is seen among patients with this type.
Type 3 : Patients with type 3(10%) is distinguished by remittent burning that occurs only on certain days. Floor of the mouth, buccal mucosa, and throat are usually affected sites. Anxiety and allergic reactions, particularly to food additives, are common in these patients.
Categorization of BMS is by Scala as [10].
Primary (idiopathic) BMS: No local/systemic factors have been found for this disease.
Secondary BMS: Caused by local/systemic factors, and respond well to aetiology-directed therapy.
Clinical presentation
Patients complain of chronic, debilitating pain lasting for 4 to 6 months. Scalding or burning sensations, Numbness or itchiness of tongue and other oral mucosal surfaces has been observed [11]. Pain can gradually or spontaneously precipitate in response to dental procedure.
It is usually restricted to tongue, but it can also affect buccal mucosa, lip, floor of the mouth and palate. Intensity of pain may be mild to moderate, continuous or intermittent in nature. It is usually limited to the oral mucosal surfaces and does not spread to other regions of face. Burning symptom of other diseases gets aggravated when food or liquids are consumed, while the pain of BMS usually subsides when food or liquids are consumed [12].
Mostly it affects anterior two-thirds of the tongue (71-78%), followed by the dorsum and lateral borders of the tongue, the anterior part of the hard palate, the labial mucosa, and gingiva [13].
Many individuals with the condition have no pain throughout the night, but it returns in the middle to late morning at a mild to moderate intensity. The intensity of the burning may rise gradually throughout the day, peaking in the late afternoon and early evening [14].
The majority of studies have discovered that dry mouth and altered taste is seen among patients with BMS. About two-thirds of patients have taste alterations, usually complaints of bitter or metallic taste. Food stimulation can help to alleviate the dysgeusic tastes that come with oral burning.
Aetiology of Burning Mouth Syndrome (BMS)
It can be caused by a variety of local or systemic causes Figure 1, such as Xerostomia, Candidal infection, Menopause, Diabetes, Allergic reactions etc. Psychological issues can also be a devastating aspect in BMS.
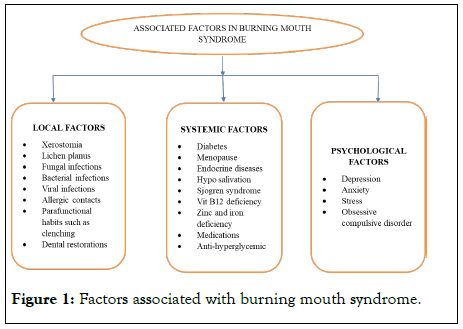
Figure 1: Factors associated with burning mouth syndrome.
Psychological dysfunction
Depression and anxiety are thought to be two frequent disorders that have a major influence in chronic pain in BMS (Figure 2) [15,16]. Rezazadeh, Farahmand, Hosseinpour, Shahriarirad et.al, conducted a study on association of burning mouth syndrome with sleep disturbance, emotional stress and depression. A total of 19 individuals with idiopathic BMS were included in this cross-sectional research, along with a control group that was similar in sex and age but did not have BMS. The Pittsburgh Sleep Quality Index (PSQI), Visual Analog Scale (VAS), Depression, Anxiety, and Stress Scale were utilized as questionnaires. Demographic data was gathered and evaluated as well. Based on the findings, patients with burning mouth syndrome had significant increase in emotional stress, depression as compared to the healthy volunteers. The link between depression and BMS, as well as the improvement of this condition as a result of cognitive-behavioural treatment and antianxiety medications, suggests that there is risk of developing pyschoneurological conditions among patients with BMS [17].
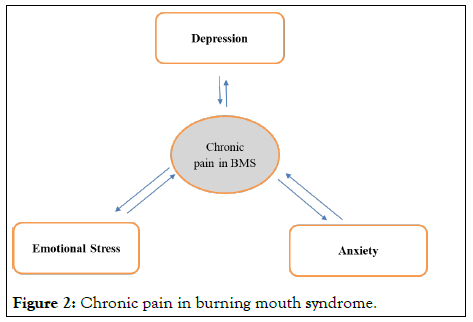
Figure 2: Chronic pain in burning mouth syndrome.
Mental illnesses play a major role in pain regulation, as they can change the pain perception by increasing or decreasing neurotransmission of peripheral pain receptors [18]. BMS has a detrimental impact on patients' quality of life, making its management a challenge for physicians.
Associated conditions
Although no specific medical disease has been linked to burning mouth syndrome, but is associated to wide range of concomitant health problems and chronic illnesses that cause discomfort. High blood glucose levels are common in patients with burning mouth syndrome, although no consistent or causative link has been shown [19].
Damage to the taste-functioning cranial nerves is considered to reduce the inhibition of trigeminal-nerve pain fibres, resulting in mouth burning sensations [20]. Some conditions associated with burning mouth syndrome are hormonal changes, taste loss, dry mouth etc [21].
Hormonal changes: The high occurrence rate in middle-aged females (ages 40-60) strongly suggests a link to female sex hormones. A hormone imbalance, or more particularly, a reduction in oestrogen levels, is the primary cause of BMS. This hormone deficiency can produce decreased saliva production, a metallic taste in the mouth, and a burning feeling. In postmenopausal women with burning mouth syndrome there is compelling evidence of hormone replacement therapy's effectiveness [22]. Volpe observed that after estradiol-based treatment, 12 out of 22 postmenopausal women experienced improvement in oral symptoms [23].
Dry mouth: Saliva is a major local factor that may have a role in the symptoms of burning mouth. Saliva has unique rheological qualities which are essential for maintaining a stable environment within the mouth cavity. Patients with burning mouth have changes in salivary composition and flow, as well as a possible shift in oral mucosal sensory perception, which is linked to dry mouth and taste changes. Salivary viscosity and symptomatology of burning mouth appear to be affected by changes in salivary content.
Taste disturbance: Patients with BMS frequently experience taste changes, which can include altered taste sensations. It’s been demonstrated that at the tip of the tongue, more the density of fungiform papillae, more is the discomfort and pain. People with more taste buds may have pain innervation with higher intensity, which increases the risk of altered taste and oral pain. Some studies found no variations in the density of the fungiform papillae between patients with BMS and controls in other trials [24].
Other possible causes: Angiotensin Covering Enzyme (ACE) inhibitors have been associated to burning mouth symptoms in some cases [25]. Oral burning was found to subside within a few weeks when these drugs were lowered or discontinued. ACE drugs have also been linked to a loss of taste sensibility [26]. Candida infections have also been linked to the development of burning mouth syndrome.
Some researchers have strongly supported the nutritional deficits (vitamins B1, B2, and B6, zinc, and so on) observed in patients with burning mouth syndrome. Some findings indicate a link between burning mouth syndrome and mucosal erosive lesions, geographic tongue and periodontitis. Individuals with unexplained oral symptoms are routinely transferred from one doctor to the next without obtaining adequate therapy. This scenario not only raises the financial burden, but it also has a major emotional impact on patients.
The clinical history is useful in determining whether or not you have burning mouth syndrome. Antipsychotics, Antidepressants, Sedatives, Antiepileptic’s, Analgesics, Sialagogues, oral mucosa protectors and Vitamin-mineral replacements are the most commonly used medicines to treat this condition. Various other treatment modalities Figure 3, such as Behavioural therapies, acupuncture, lasers, Meditation, psychotherapy and electroconvulsive therapy has also been involved; the goal of these medications is to alleviate patients' suffering, enhance the quality of life by bringing their conditions under better control [27,28].
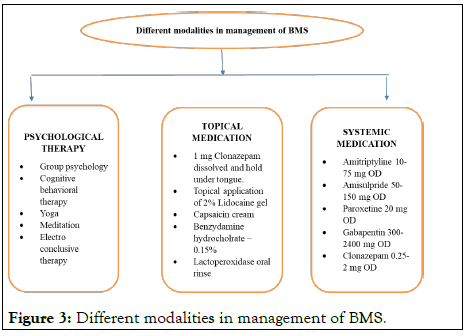
Figure 3: Different modalities in management of BMS.
According to Grushka, the optimum management for the condition is an amalgamation of medications such as gabapentin, baclofen and clonazepam [29]. Capsaicin works by depleting component p, which causes less peripheral burning [30]. Volpe discovered that after estradiol-based therapy, 12 out of 22 postmenopausal women had improvement in oral symptoms. Bergdahl advocated for BMS sufferers to get cognitive behavioural treatment. Following cognitive behavioural treatment, he noticed a decrease in pain severity.
BMS is a serious medical illness that causes a major burden on patients and the healthcare system. It causes significant morbidity to the patients. The actual cause of burning mouth syndrome remains unknown because of its complex etiopathogenesis, therefore it's important to look for and treat a secondary form of the disease. It causes both physiological and psychological stress among patients. It has also been observed that the stress, anxiety, depression and other psychological disorder play a demonstrable role in burning mouth syndrome. To date, there is no specific management for BMS. Medical and psychosocial therapy may be beneficial in symptom alleviation but patient should be made aware that the symptoms will not go away completely but the quality of life can be improved. However, further research is needed to determine long-term prognosis.
Citation: Mohod S, Chandak S, Dangore S, Chhabra KG, Reche A, Patel S (2022) Burning Mouth Syndrome: A Review. J Hepatol Gastroint Dis. 8: 198.
Received: 04-Jan-2022, Manuscript No. JHGD-22-43542; Editor assigned: 07-Jan-2022, Pre QC No. JHGD-22-43542 (PQ); Reviewed: 21-Jan-2022, QC No. JHGD-22-43542; Revised: 24-Jan-2022, Manuscript No. JHGD-22-43542 (R); Published: 31-Jan-2022 , DOI: 10.35248/2475-3181.1000198
Copyright: © 2022 Mohod S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.