
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2023)Volume 13, Issue 5
Thrombocytopenia, defined as a platelet count of less than 150,000 platelets/uL in an adult, can have many causes including medications, infections, nutritional deficiencies, as well as autoimmune disorders. Commonly, drug- induced thrombocytopenia has been reported with heparin, sulphonamides, carbamazepine, and gold for rheumatoid arthritis, haloperidol, ibuprofen, naproxen, phenytoin, platinum chemotherapeutics, and quinidine. We present the case of a 58-year-old female with severe thrombocytopenia attributed to a Calcium Channel Blocker (CCB) overdose, a very rare cause of thrombocytopenia.
Thrombocytopenia; Drug overdose; Calcium channel blocker; Medication
Thrombocytopenia is a rare and fatal side effect triggered by certain medications. Medications that are used in the hospital that may lead to thrombocytopenia include heparin, antibiotics, and pain medications. However, studies have shown that these medications are more likely to cause thrombocytopenia when taken in excess, as opposed to recommended doses [1]. Other common etiologies for thrombocytopenia in the hospital include infections (such as human immunodeficiency virus or hepatitis C), nutritional deficiencies, chronic alcohol use, and autoimmune diseases. Calcium channel blockers are a class of medication used in the management of hypertension and have been reported to cause thrombocytopenia in three other case reports [2-4]. Nifedipine was implicated in one and Amlodipine in two other case reports with anti-amlodipine antibodies confirmed in one of the cases [5,6-12]. However, these cases included patients taking CCBs at therapeutic doses. We are reporting a case of amlodipine-induced severe thrombocytopenia from a drug overdose.
Hospital course
A 58-year-old Caucasian woman with a history of hyperlipidemia, hypertension, and more recent right parietal hemorrhage six weeks prior to her admission presented after a suicide attempt by overdosing with amlodipine, metoprolol, and alprazolam. Two days prior to her suicide attempt, she refilled a thirty-day prescription of amlodipine 10 mg PO every day. She was found unconscious by her roommate. She received calcium gluconate and glucagon; and was managed with a transcutaneous pacer for severe sinus bradycardia with cardiogenic shock. On admission, she developed severe transaminitis. It returned to a mildly elevated state of transaminitis after the second day in the ICU and fluctuated between 60-90 Units/L afterward.
She required hemodynamic pressor support on arrival with an initial blood pressure of 75/60 mmHg in the form of norepinephrine, epinephrine, and dobutamine and was treated with continuous insulin infusion and methylene blue. The transcutaneous pacer was successfully replaced with a transvenous pacer.
Her course was further complicated by acute kidney injury and lactic acidosis that nephrology managed with Continuous Veno- Venous Hemofiltration (CVVH), sodium bicarbonate, and phosphate infusions. The patient was found to have severe thrombocytopenia with a decline in her platelet count from 200,000 cells/uL to 7000 cells/uL roughly 48 hours after her overdose. Fibrinogen level, Coomb’s test, HLA autoantibodies, and heparin IgG were normal. Schistocytes were absent on the peripheral blood smear. Her Hemoglobin, White count stayed within normal limits. Hemoglobin did not experience a similar crash and was stable between 10-12 mg/dL and gradually dwindled during her hospital course. She had leukocytosis which continued to elevate during her entire stay in the MICU.
The patient was managed with platelet transfusions and 50 grams of Intravenous Immunoglobulin (IVIG) (~1 gram/kg) during day days 2 and 3 of her hospital stay in addition to 40 mg IV QD of Dexamethasone from day 2 to day 5. Eventually, the patient’s platelet count began to rebound after reaching a nadir of 7000 cells/uL. Eventually following IVIG and dexamethasone the platelet count rose to 50k cells/uL and stabilized in the 60-80k range approximately 7-8 days from the estimated time of Amlodipine overdose (Figure 1).
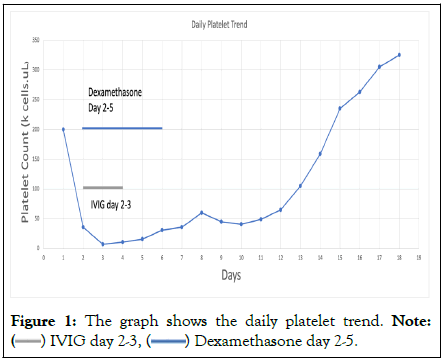
Figure 1: The graph shows the daily platelet trend. Note:
( ) IVIG day 2-3, (
) IVIG day 2-3, ( ) Dexamethasone day 2-5.
) Dexamethasone day 2-5.
Unfortunately, given her recent intracerebral hemorrhagic stroke, the patient experienced renewed bleeding most likely caused by her severe thrombocytopenia, and remained critically ill with poor mentation and inability to wean off mechanical ventilation. At the same time, her course was further complicated by Ventilator-Associated Pneumonia (VAP) with Methicillin-Sensitive Staphylococcus aureus (MSSA) and Klebsiella, as well as multi-organ failure including acute persistent anuric renal failure requiring CVVH. Eventually, her decision maker transitioned her care to focus on palliative measures with compassionate extubation, passing away shortly thereafter.
Thrombocytopenia is a common finding in critically unwell patients with a broad differential including Disseminated Intravascular Coagulopathy (DIC) and Idiopathic Thrombolytic Purpura (ITP). Our patient developed severe thrombocytopenia after overdosing on amlodipine, metoprolol, and alprazolam. Amlodipine has a half-life of 48 hours [10]. In our case, the onset of thrombocytopenia after oral overdose ingestion was approximately 48 hours with a nadir of 7k cells/uL during day 3 of hospitalization.
Platelet suppression or destruction of platelets are proposed mechanisms of Drug-Induced Thrombocytopenia (DITP). In vitro studies have shown that verapamil and diltiazem-and dihydropyridine calcium blockers to a lesser extent-downregulate platelet aggregation via inhibition of alpha 2 adrenergic receptors. CCBs have also been shown to decrease the concentration of thromboxane B2, the inactive metabolite of thromboxane A2, an eicosanoid that has thrombopoietic and thrombotic properties [6]. Rostagno, et al. [6], concluded that there would need to be a complete inhibition of the cyclooxygenase pathway to completely inhibit activation of platelets with thromboxane A2 and that the mild decrease in Thromboxane activity was negligible. However, our patient had recently filled a prescription with 60 tablets of Amlodipine 5 mg and possibly ingested a cumulative dose of 300 mg of amlodipine. We postulate that this dose may have a significant effect on platelet inhibition and degradation via inhibition of Thromboxane A2 production and the cyclooxygenase pathway. In animal models, CCBs upregulate prostacyclin production in dogs, downregulating platelet activity. Dihydropyridine calcium blockers have been shown to decrease platelet aggregation in dogs with vascular grafts [8]. Furthermore, Garbe, et al. [5], demonstrated that amlodipine triggered the production of drugdependent antibodies against platelets too. Autoimmune thrombocytopenia due to medications is under-diagnosed because it may be confounded with idiopathic thrombocytopenia. The pathophysiology is unclear, but it has been proposed that the sensitizing drug augments the binding affinity of the immunoglobulins to platelets. However, the binding affinity is insignificant without medication. Alternatively, the antibodies and medication may create conformational changes in platelet surface proteins [12].
We performed a comprehensive literature review to find three case reports of calcium-channel-blocker induced thrombocytopenia after long term use. Nifedipine was associated with thrombocytopenia in one patient and amlodipine was the causative agent in two others. The dihydropyridine class of calcium-channel blockers has been shown to downregulate platelet aggregation. In previous case reports, the patients were using amlodipine either chronically or acutely. In one case, a 79- year-old male who had been on long-term amlodipine began to suddenly develop hematomas, hematuria, and petechiae [5]. After holding amlodipine for 7 days and receiving 5 days of steroids, the patient’s platelets rebounded from 1,000 cells/uL to 201k cells/uL. It was possible to identify the amlodipine as the causative agent after the thrombocytopenia recurred on restarting amlodipine with confirmation of antibodies directed against platelets [5]. Another case report presented a patient with thrombocytopenia after 2-3 days of amlodipine consumption who had diffuse petechiae and profuse, frequent menorrhagia at a nadir platelet level of 12,000 cells/uL. Removal of amlodipine for 7 days improved the platelet count to 172,000 cells/uL [9]. There has been one documented case report of thrombocytopenia due to nifedipine that caused the platelet level to drop to 20k cells/uL after 20 days on nifedipine. Platelets returned to baseline after holding nifedipine for 10 days.
Another patient developed DITP from dual usage of simvastatin and amlodipine; she presented with multiple ecchymoses on arrival at the Emergency department. Following 17 days of hospitalization prior to returning and 7 days of prednisolone (1 mg/kg), her platelet count normalized. Drug-induced thrombocytopenia was confirmed after restarting simvastatin; the patient had a platelet count of 98k cells/uL and subsequent hives. Afterward, she mistakenly took amlodipine 10 mg once dropping her platelet to 32k cells/uL. She was asymptomatic, and no further intervention was warranted [11].
Amlodipine is a rare cause of DITP. Consequently, DITP may be attributed to Immune Thrombocytopenic Purpura (ITP) [7]. Drug-Induced Thrombocytopenia (DITP) appears suddenly and is often severe, with a risk of major bleeding and death [2]. DITP can develop either from dose-dependent bone marrow suppression or from peripheral platelet destruction [2]. ITP is thrombocytopenia not related to a systemic disease, whereas DITP involves drug ingestion [3]. Early recognition of DITP is essential, especially in critically ill patients, to promptly remove the offending agent [3]. Platelet counts usually recover within 1-10 days after discontinuation of the offending agent [4]. Our patient’s platelet count remained below 150k cells/uL until day 12-13 of hospitalization, conceivably due to an overdose from amlodipine contrasting consumption of a therapeutic dose.
Amlodipine has a half-life of 24-48 hours [10]. The main course of treatment for DITP is steroids and sometimes IVIG [7]. In our patient, the platelet count started to reach normal levels approximately 13 days after her overdose at 159k cells/uL. While the IVIG and the corticosteroids stabilized the platelet count between 70-85k cells/uL, it did not fully recover to normal levels immediately. There may have been confounding variables by other causes such as multi-organ failure-namely transaminitis and bone marrow suppression from cardiogenic shock and sepsis from ventilator-associated pneumonia. However, her thrombocytopenia is likely due to transaminitis or septic shock because her liver functions stayed mildly elevated after the severe transaminitis during her first 48 hours after admission. Bone marrow suppression is less likely because the patient’s hemoglobin dwindled gradually during her three weeks in the ICU, contrasting to the sudden crash of platelets from 200k cells/uL to 7000 cells/uL within 24 hours; this gradual anemia is more likely explained from the extensive blood draws for continuous monitoring in the intensive care unit. Furthermore, her white count had always stayed elevated during her hospital stay. Septic shock is much less likely because the patient developed ventilator-associated pneumonia during day 10 of hospitalization. Despite her infection, the patient’s platelet had a continuous upward trend and recovered to normal limits by day 12, making sepsis less likely. Lastly, this patient never had pancytopenia during her hospital stay which would be consistent with organ failure, bone marrow suppression, or shock.
The patient had progressive bleeding at a previous intraparenchymal hemorrhage that happened six weeks prior to her overdose. Interestingly, our patient did not manifest clear signs of bleeding-hematomas, menorrhagia, petechiae, and ecchymoses-on physical exam, which contrasted with the findings of previous case reports.
To our knowledge, we present the first case of severe thrombocytopenia after an overdose of Amlodipine. In which the duration of the thrombocytopenia was longer likely in the context of a supratherapeutic dose compared to therapeutic doses. Moreover, the diagnosis of DITP was complicated by a broad differential including other causes of thrombocytopenia in critically ill patients. Calcium-channel blockers remain an important but rare cause of thrombocytopenia that must be considered in the diagnostic work-up in order to permit timely discontinuation of the offending agent, preventing severe bleeding and death.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhou AL, Gutsche M (2023) Calcium Channel Blocker Induced Thrombocytopenia in the Intensive Care Unit: A Rare Presentation and Review of the Literature. J Clin Toxicol. 13:545.
Received: 29-May-2023, Manuscript No. JCT-23-24498; Editor assigned: 31-May-2023, Pre QC No. JCT-23-24498 (PQ); Reviewed: 14-Jun-2023, QC No. JCT-23-24498; Revised: 21-Jun-2023, Manuscript No. JCT-23-24498 (R); Published: 28-Jun-2023 , DOI: 10.35248/2161-0495.23.13.545
Copyright: © 2023 Zhou AL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.