Journal of Hepatology and Gastrointestinal disorders
Open Access
ISSN: 2475-3181
+44-77-2385-9429
ISSN: 2475-3181
+44-77-2385-9429
Case Report - (2021)Volume 7, Issue 2
A 37 years of age Caucasian male was eventually reffered to Gastroenterology Department at local hospital with recurrent history of visits to Accident and Emergency (A&E), for chronic history of nausea, vomiting, abdominal pain, unable to eat, failure to thrive and weight loss. With background history of Type 1 Diabetes mellitus on some occasions he was found to be ketoacidotic, while with normal blood sugars on most of the visits to A&E. He underwent thorough investigations with no abnormality found except for abnormal HbA1c. He declined urine drug testing and on further he gave history of using Cannabis in the form of CBD (cannabidiol) Oil 3-4 times per week since age 16. Patient was advised to stop use of CBD oil and educated for better control of HbA1c and neuropathic pain killers. Patient consented for these changes and this resulted in dramatic response with resolution of all the symptoms. Patient currently is strictly abstinent of cannabis in any form. The most populous model suggests overriding of gut Cannabinoid receptors-CB1 (emesis inducing) over the brain receptors (emesis inhibition) and down regulation of Transient Receptor Potential Vanilloid Subtype 1 (TRPV-1) in gut and chemoreceptor-trigger zone, causing nausea and vomiting and some relief with hot showers in patients with long term use of Cannabis.
Cannabis; Hypermesis Syndrome; CBD oil; Cannabiniod(CB1) receptors in Gut; Subtype 1 Receptor (TRPV1).
A 37 years of age Caucasian male was eventually referred to Gastroenterology Department at local hospital with recurrent history of visits to Accident and Emergency (A&E), for chronic history of nausea, vomiting, abdominal pain, unable to eat, failure to thrive and weight loss. With background history of Thpe 1 Diabetes mellitus on some occasions he was found to be ketoacidotic, while with normal blood sugars on most of the visits to A&E.
He underwent thorough investigations with no abnormality found except for abnormal HbA1c. He was investigated with Endoscopy- suggesting mild LA Grade 1 oesophagitis, GET test, suggesting delayed gastric emptying and that led to presumption of possible role of Autonomic Neuropathy due to teen-age history of Diabetes mellitus type 1. His abdominal x-rays reported normal, and CT Scans did not show any significant pathology. He wanted to be managed on out-patient basis, so initially discharged with Nasogastric tube (NG) that did not help. He later had balloon gastrostomy (PEG) and during later Endoscopy booking this was changed with Low Profile 16Fr Mic- Key tube with 3.5 cm stoma distance [Figure 1].
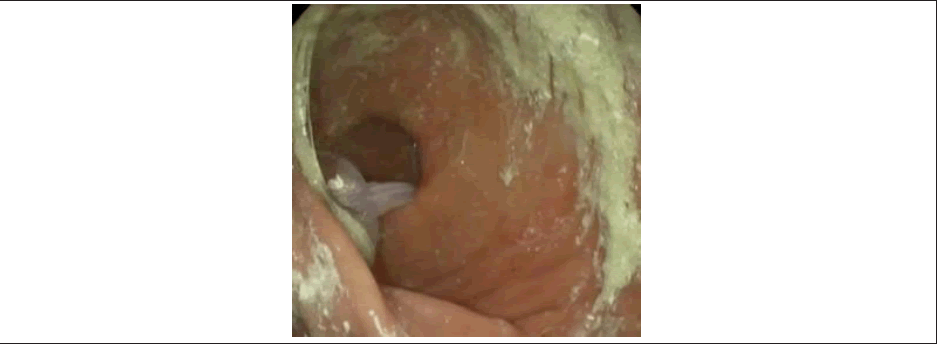
Figure 1: Previous balloon gastrostomy was removed and changed with Low Profile 16Fr Mic-key tube with 3.5 cm stoma distance. Straight forward insertio
Number of times PEG-J tube would come out due to episodes of vomiting [Figure 2,3]. This resulted in number of times repeat endoscopy for reinsertion of NJ and PEG-J tube following episode of vomting to help achieve desired weight while in community with enteral feeding. Although there was gain in weight of about 2 kilograms, the symptoms of nausea, vomiting, and abdominal pain persisted.
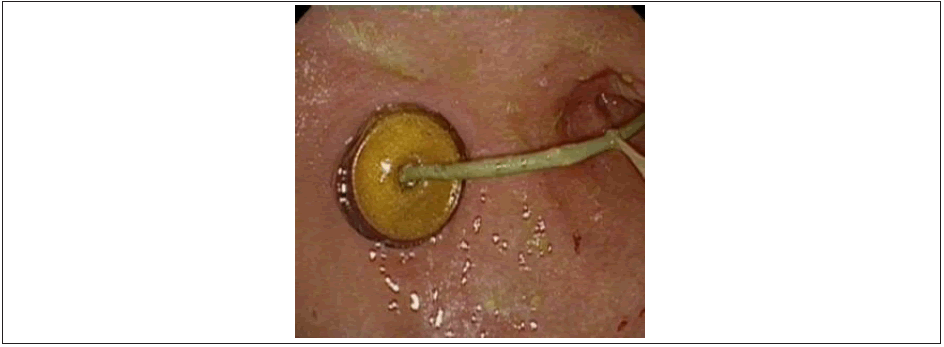
Figure 2: PEG-J tube Insertion.

Figure 3: CT-Abdomen-Pelvis- Coronal view. PEG-J migration into stomach.
The patient was reviewed by the Endocrine and Diabetic Team, and the Neurothesiometer findings suggesting Impaired vibration in legs in particular left leg, along with delayed Gastric Emptying test, favored intestinal failure or gastroparesis, related to Diabetes mellitus type 1 [Figure 4]. However, once all the relevant investigations and management failed, it was decided to approach the patient and insist of urine drug testing, that patient had previously declined.
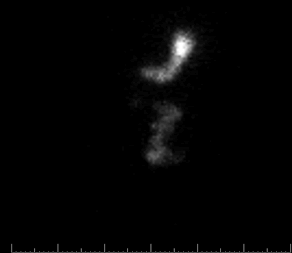
Figure 4: Static Gastric Emptying 120 minutes, suggesting Delayed Gastric Emptying
Again, he declined urine drug testing and on further inquiry he gave history of using Cannabis in the form of CBD (cannabidiol) oil 3-4 times per week since age 16. He noticed initially it relieved his symptoms of tingling and sharp pains in his legs associated with peripheral neuropathy associated with abnormal HbA1c. However, in last 6 years or so, he started having progressively worsening symptoms of nausea, vomiting, unable to keep anything down his gullet and noticed weight loss. He reported some relief in his symptoms with hot showers.
Height 182 cm, weight 72.15kg, BMI 21.7, blood pressure 112/73, pulse 123. Pedal. Pulses palpable in both feet. Neurothesiometer, right 13.5 V, left 29 V.
• 17 normal.
• 17 - 24 suspect neuropathy if other signs are present such as dysthesia.
• 25+ definitely neuropathic).
Urine: Trace of blood.
Blood Tests: Creatinine 57, eGFR over 90, ALP 64, ALT 16,
HbA1c 86.
Patient was advised to stop use of CBD oil and educated for better control of HbA1c and neuropathic pain killers.
Outcome and Follow up
• Periodic review in Gastroenterology Clinic
• Patient reported resolution of all the symptoms of nausea, and vomiting.
• Gained weight and satisfied with the outcome, self- monitors his blood sugars, and compliant with sub- cutaneous insulin administration and reported relief of Neuropathic symptoms with Gabapentin 300 mg twice a day, attends regular check of HbA1c blood tests, and weight and BMI estimation organized by the General Practitioner in the community periodically.
Described first in 2004, by Allen et al, the Cannabinoid Hyperemesis Syndrome is associated with cyclical nausea and vomiting associated with at least weekly use of cannabinoids [1]. Chocron et al [2] have reported Cannabinoid hyperemesis accounting for 6% of patients presenting to emergency departments with recurrent vomiting in one study2. An estimated 182 million people were cannabis users worldwide in 2013. Since in 2016 this number has increased to 192 million [2-6].
Most cases are treatment challenge to the physician and in particular to the A&E, and GP Surgeries, and most get referral to the Gastroenterology department eventually. All the patients have multiple admissions to the hospital, usually thorough gastrointestinal investigations, including invasive. In patients with co-morbid disorders like our patient with type 1 Diabetes mellitus, a further confounding of autonomic diabetic peripheral neuropathy related investigations was additional challenge towards diagnosis and management.
Although the research is on-going on further understanding the causal relationship, the most populous model suggests chronic use of cannabis resulting in antagonistic function of Cannabinoid (CB1) receptors in Gut [7], over-riding the brain receptors, causing nausea and vomiting and opposite of receptor function in the brain resulting in vomiting [8].
The other model is down regulation of Transient Receptor Potential Vanilloid Subtype 1 Receptor (TRPV1), with chronic cannabis use. Located in Gut and Chemoreceptor Trigger zone, down regulation of TRPV1 resulting in symptoms of nausea and vomiting, with augmentation of TRPV1 with other stimulators including hot bath or capsaicin explaining the resolution with hot bath [3]. Taken all information into account, the likelihood of patients reporting to the A&E, with complaints of nausea and vomiting appear with tendency to increase. Clinicians need to be more aware of the detailed history taking, towards creating effective differential towards better patient management.
Common symptoms and history associated with Cannabinoid Hyperemesis Syndrome include (Adapted from Sorensen et al [7] and Chocron et al [2]);
• Severe nausea and vomiting, in a cyclic pattern, (100%)
• Abdominal pain (85.1%)
• At least weekly use of Cannabis (97.4%)
• History of regular cannabis use for >1 year (74.8%)
• Compulsive hot showers or baths with symptom relief (96.8%)
• Young age at the time of presentation (often < 50 years) (100%)
Percentages express the frequency of the characteristics found in the systematic review by Sorensen et al (maximal n=227). Cyclic Vomiting should be considered in patients who do not respond to above measures, especially if case presents acutely with less than one-week duration [9].
We would like to acknowledge and thank the Professors and mentors who guided us throughout our academic paths and also colleagues who privately shared very personal and touching experiences and thoughts that sought for compassionate help in times of troubles, and made us learn, together.
No potential conflict of interest was reported by the authors.
Citation: Mansoor Z (2021), Cannabinoid Hyperemesis Syndrome – CB1 and TRPV1 Paradox’, J Hepatol Gastroint Dis, 7:182
Received: 29-Mar-2021 Accepted: 13-Apr-2021 Published: 19-Apr-2021 , DOI: 10.35248/2475-3181.21.7.182
Copyright: © 2021 Mansoor Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.