Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2022)Volume 13, Issue 3
Vogt-Koyanagi-Harada disease (VKH) is a relatively uncommon entity encountered in Indian clinical ophthalmic practice. Acute angle closure is an easy to miss presenting feature of the disease. Our patient had classical history, symptoms and signs of acute angle closure crisis in both eyes. Ophthalmic evaluation including imaging helped in reaching a diagnosis and marked improvement was noted once corticosteroids were started. Initiation of immunosuppressive therapy helped in stabilizing the ocular lesions and improving visual acuity. Thus one may bear in mind VKH as an important differential diagnosis when faced with a case of bilateral acute angle closure.
Vogt-Koyanagi-Harada (VKH) disease; Bilateral acute angle closure; Uncommon presentation
The Vogt-Koyanagi-Harada (VKH) syndrome is an autoimmune disorder with varied clinical features, both ocular and extraocular. It tends to be concentrated in people of Japanese and Native American ancestry and is predominantly seen in females in their third to fourth decades of life. A long term multi-racial study, [1] reported only 1.3% of the VKH patients to be of Asian Indian ancestry. Acute Angle Closure (AAC) attack as a presentation of VKH is an uncommon entity that poses a diagnostic challenge. Few studies, [2-4] worldwide have reported angle closure as a presenting feature of VKH. We are reporting a case of VKH which presented to us as a bilateral AAC episode.
A 47-year old female presented with complaints of painful diminished vision in both eyes (right>left) associated with severe headache and vomiting episodes since past four days. She had no history of any recent trauma, surgical or anesthetic procedure or drug intake. She had no history of a previous similar episode and reported no significant systemic illnesses.
Her Best Corrected Visual Acuity (BCVA) for distance and near was counting fingers at two meters with N36 in the right eye and 6/18 with N12 in the left eye. The Intra-Ocular Pressure (IOP) recorded by Perkin’s applanation tonometer was 40 mmHg in the right eye and 28 mmHg in the left eye. Anterior segment examination revealed circumciliary congestion, diffuse corneal haze, 2+ cells in the Anterior Chamber (AC), closed angles on slit lamp (Van Herrick grade 0) and sluggishly reacting mid-dilated pupils-all findings more pronounced in the right eye. Posterior segment evaluation could not be done immediately due to media haze. Ultrasound B-scan showed attached retina in both eyes with vitreous opacities in right eye.
Based on the signs and symptoms, she was diagnosed as a case of bilateral AAC. First day treatment on stat dose of Intravenous (IV) 20% mannitol 1 g/kg Body Weight (BW), oral acetazolamide 250 mg 6 hourly, 1% prednisolone acetate 6 hourly and 0.5% timolol maleate twice daily eye drops brought the IOP to 32 mmHg and 24 mmHg in the right and left eyes, respectively. Headache complaint persisted the following day and IOP reduction was much less than expected. Slight improvement was observed in the anterior segment findings however vision remained unchanged. Color vision was found to be defective in the right eye. These findings led us to suspect secondary angle closure.
A dilated retinal examination revealed asteroid hyalosis in the right eye and vitreous haze, blurring of nasal disc margin, tortuous retinal vessels with areas of serous detachments and peripheral retinal exudates in both eyes (Figures 1a-1d). Optical Coherence Tomography (OCT) imaging of the macula corroborated the clinical findings (Figures 2a and 2b). Anterior segment OCT imaging revealed angle closure in the right eye (Figure 3) and highly occludable angles in the left eye. In view of the presence of bilateral panuveitis with serous neurosensory detachments, a diagnosis of probable VKH with secondary angle closure was made. A detailed investigative workup including blood tests, radiographic imaging was ordered to rule out other causes of panuveitis all of which were within normal limits.
After obtaining medical clearance, pulsed therapy of IV methylprednisolone 1 g/day for three days was started and later shifted to oral prednisolone 1 mg/kg BW dose. IOP stabilized after the pulsed therapy with improvement in AC depth and reaction. Steroids were continued along with twice daily 2% homatropine and 0.5% timolol eye drops and patient was discharged in a week. BCVA on discharge was 6/36 in the right eye and 6/12 in the left eye and IOP was 14 mmHg in both eyes. Immunosuppressive therapy was started and patient kept under close follow–up. At two month follow-up, fundus findings had stabilized (Figures 4a and 4b) with normal range IOP and BCVA of 6/12 N8 in the right eye and 6/6 N6 in the left eye.
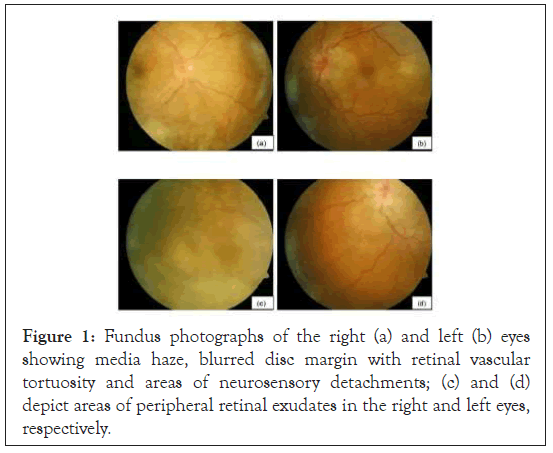
Figure 1: Fundus photographs of the right (a) and left (b) eyes showing media haze, blurred disc margin with retinal vascular tortuosity and areas of neurosensory detachments; (c) and (d) depict areas of peripheral retinal exudates in the right and left eyes, respectively.
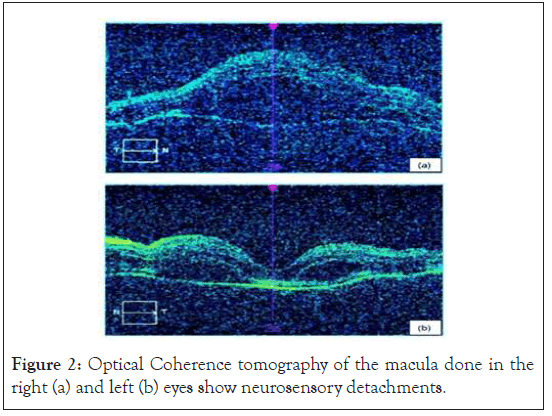
Figure 2: Optical Coherence tomography of the macula done in the right (a) and left (b) eyes show neurosensory detachments.
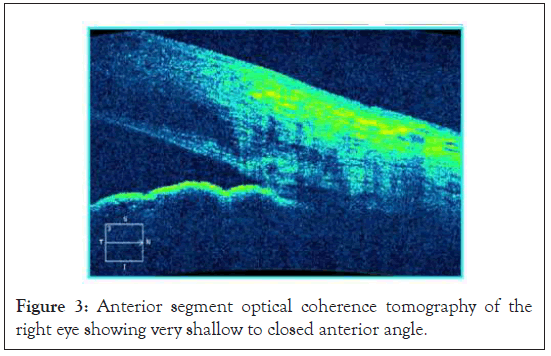
Figure 3: Anterior segment optical coherence tomography of the right eye showing very shallow to closed anterior angle.
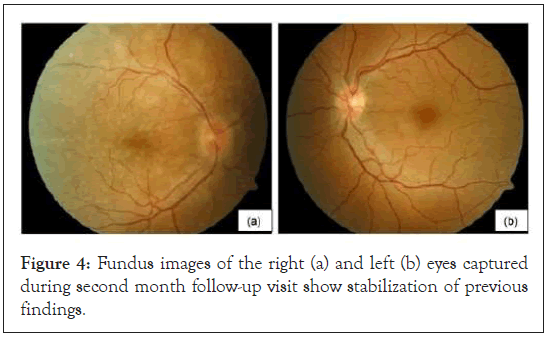
Figure 4: Fundus images of the right (a) and left (b) eyes captured during second month follow-up visit show stabilization of previous findings.
This patient had a typical presentation of an AAC attack. She had no other systemic findings suggestive of VKH and was diagnosed as a case of probable VKH with bilateral secondary angle closure as per the diagnostic criteria [5]. Such cases pose a diagnostic dilemma when being dealt with in routine clinical practice thereby delaying initiation of correct treatment therapy. Studies, [6,7] have noted shallowing of AC, moderate increase in IOP and swelling of the ciliary processes in the early phase of VKH disease. This could explain the cause of occurrence of angle closure in undiagnosed VKH patients as a presenting feature.
AAC is an uncommon presenting feature even in VKH susceptible populations. Yang et al. [2] observed in their study that 1.6% of the VKH patients were misdiagnosed as acute angle closure glaucoma. They had a narrow or closed angle at their first visit with decreased visual acuity. The increased IOP responded well to corticosteroids but not to anti-glaucoma treatment. A study done in China, [3] reported bilateral acute angle closure glaucoma as an unusual mode of presentation in four VKH patients.
There has been a documented case report,4 from the Middle Eastern region where initial misdiagnosis followed by unnecessary interventions led to delay in diagnosis. There have been very few Indian case study reports of AAC as VKH presentation. One study, [8] retrospectively analyzed 448 eyes of 224 VKH patients of Indian origin. Glaucoma at presentation prevailed at 15.8% out of which 21 eyes (29.6%) had angle closure and 9 eyes (12.6%) had acute angle-closure crisis.
Unilateral AAC presentation has been noted in a case report, [9] observing two Indian VKH patients where both patients had the characteristic clinical features of VKH involving only one eye. Another study, [10] reported a simultaneous bilateral AAC crisis in a VKH patient.
All these case reports like ours have a common feature of a knee jerk response of labeling the patients with acute angle closure, with some being subjected to unnecessary interventions for IOP control such as laser peripheral iridotomy. Detailed ophthalmic check-up, imaging tools and a thorough systemic work up allow prompt diagnosis and initiation of therapy which improves the visual recovery prognosis.
Nil
The authors declare that there are no conflicts of interest.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Bhedasgaonkar SS, Manral H, Nadkarni SU (2022) Case Report of an Unusual Presentation of Vogt-Koyanagi-Harada Disease as Bilateral Acute Angle Closure. J Clin Exp Ophthalmol. 13:911
Received: 03-Jan-2022, Manuscript No. JCEO-22-15351; Editor assigned: 05-Jan-2022, Pre QC No. JCEO-22-15351 (PQ); Reviewed: 19-Jan-2022, QC No. JCEO-22-15351; Revised: 24-Jan-2022, Manuscript No. JCEO-22-15351 (R); Published: 31-Jan-2022 , DOI: 10.35248/2155-9570.22.13.911
Copyright: © Bhedasgaonkar SS et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.