
Journal of Perioperative & Critical Intensive Care Nursing
Open Access
ISSN: 2471-9870

ISSN: 2471-9870
Case Report - (2021)Volume 7, Issue 5
A 28 year old pregnant patient with pre-existing comorbidities admitted with fever, shortness of breath, decreasing blood oxygen saturation levels at COVID 19 suspected ward, was shifted to covid area after her- PCR reports came out to be positive. Her symptoms gets worsen, hence started on mechanical ventilation and baby was delivered by emergency cesarean section. Her blood oxygen saturation levels were 80-90% in spite of full ventilator support. Later on RT- PCR report came negative and patient was managed in ICU, where holistic management of patient was and patient was discharged on room air with minimal complications.
COVID 19 infection; RT-PCR; Mechanical ventilation; Blood oxygen saturation level; ICU; Pregnancy
Case Review
A 28 years old gravid female G2P1 with 35 week and 4days period of gestation, known case of hypothyroidism, grade two obesity was admitted (03/06/2021) in COVID suspect ward with complaints of fever, shortness of breath, SpO2 of 87% on room air. RT-PCR covid test was done which came out as positive and she was shifted to covid positive ward. She developed dyspnea and was provided oxygen support through facemask at 6 L/min. Her SpO2 further deteriorated on 06/06/2021, oxygen requirement increased. She was taken on Non-Invasive ventilation support, PEEP 5 with intermittent HFNO (high flow nasal oxygen). She was under continuous monitoring for fetal well-being. Her saturation deteriorated further inspite of giving oxygen support to 60 -70%. She underwent endotracheal intubation, started on mechanical ventilation support, VC- AC mode, Fi O2- 100%, TV- 380 ML, PEEP- 8 mmHg, PS-14 mmHg under sedation and was immediately shifted for an elective LSCS under general anesthesia (in view of fetal well-being and low blood oxygen saturation) done at 38 weeks of gestation (08/6/2021), right internal jugular vein central catheter, ryles tube and foleys catheter was inserted. Baby boy of 3.2 kg, spontaneously crying with good Apgar score was shifted to neonatal intensive care unit for few hours of monitoring. Mother was shifted to covid positive ICU, post LSCS on continuous mechanical ventilation support mode – VC/AC, FiO2- 100%, PEEP- 14, TV- 360, Frequency- 35 breaths/minute, inotropic support – Injection noradrenaline (8/50) @ 4 ml/hour, sedation with continuous infusion of rocuronium, ketamine and fluid therapy, urine output of 50-100 ml/hour and normal blood glucose ranges. Per vaginal bleeding was minimal post LSCS, soft breast, healthy suture line, breast milk was expressed second hourly and was discarded as well as hot fomentation was provided. Her SpO2 ranges between 80-90% on complete mechanical ventilation support (Mode- VC- AC, FiO2- 90%, TV- 360 ml, PEEP- 12 cm H2O. She was on continuous observation, and again RT-PCR covid test was done after 20 days (12/6/2021) of LSCS which came out negative and she was shifted to Non COVID adult ICU. Patient had three proning sessions to maintain oxygen saturation.
On 16/6/2021, patient had Acinetobacter baumani culture positive in endotracheal aspirate, Klebsiella in blood culture and budding yeast cells in urine culture. Patient was diagnosed with ventilator associated pneumonia, septic shock in view of low mean arterial pressure <65 mmHg despite continuous infusion of noradrenaline (8/50) @ 5- 10 ml/hr, Acute respiratory distress syndrome with Pa O2 in arterial blood gas analysis /Fraction of inspired oxygen score of 83/0.50=166 (moderate ARDS). Antibiotics were started as per culture and sensitivity report. She had thick endotracheal secretion with clogging of endotracheal tube and needed prolonged ventilator support for which tracheostomy was done on 21/6/2021; 7.5 mm tracheostomy tube was inserted. For thick secretions, chest physiotherapy and mucomyst 600 mg TDS via ryles tube was started. In AICU, she was kept on mechanical ventilator support on AC/VC mode, fio2 100%, PEEP 12. On 25/6/2021, patient has irregular ECG rhythm, P waves were present hence started on tablet Ivabradine 5 mg BD. She was weaned gradually from mechanical ventilation support as shown in Tables 1 & 2; tracheostomy decannulation was done on 17/7/2021. Ryles tube, foleys catheter, central line removed. Tracheostomy site healed within few days. Started on high protein soft diet orally, and voiding via self. Patient had secondary degree bedsore on lips, forehead, and hips due to prone position that were managed by wound care team using mepilex dressing. Perianal excoriation was managed with antifungal cream for local application. Patient had poor muscle strength, for which regular sessions of physical medical rehabilitation and TENS therapy was started. Patient was bedridden, she was gradually provided with sessions of bed-out, visit to hospital corridor. Patient was discharged from ICU to directly home on 19/7/2021 with oxygen concentrator as an emergency measure with follow up in pulmonary OPD after 15 days.
| Tests | On 03/06/2021 | On 15/06/2021 |
On 15/ 07/2021 |
Reference value |
|---|---|---|---|---|
| Hemogram | 10.9 g/dl | 11.5 g/dl | 10.3 g/dl | 12.3â??15.3 |
| WBC | 7.25 | 16.64 | 11.07 | 4,400-11300 |
| Absolute lymphocyte count (per mm3) | 8000 | 7000 | 2000 | 1000-4000 |
| PLT | 75 [10^3/ul] | 195 [10^3/ul] | 279 [10^3/ul] | 149,000-409,000 |
Table 1: Showing investigations of the patient.
| Test on 03/06/2021 | result | Reference value | Test on 03/06/2021 | Result | Reference value |
|---|---|---|---|---|---|
| AST (SGOT) | 133.1 IU/L | Female < 35 U/L (0 Day-100 Year) | Procalcitonin (D) | 0.367 ng/ml | <0.02 ng/mL |
| ALT (SGPT) | 89.9 IU/L | Female <35 IU/L (1 Month-100 Year) | Serum Chloride | 105 Meq/l | 101-109 mEq/L |
| Serum Urea | 8 mg/dL | Adult 17.00 mg/dL to 43.00 mg/dL (0 Day-100 Year) | Serum Potassium | 3.99 Meq/l | 3.5-5.1 mEq/L |
| Serum Creatinine | 0.63 mg/dL | 0.66 mg/dL to 1.09 mg/dL for Female (0 Year-50 Year) | Serum Sodium | 135 Meq/l | 136-146 mEq/L |
| Serum Total Bilirubin | 0.98 mg/dL | 0.3â??1.2 mg/dL | Erythrocyte Sedimentation Rate | 88 mm/hour | 0-30 mm/hour |
| D-dimer | 0.92Ug/ml | 0-0.5 ug/ml | ferritin (A) | 215 ng/ml | 10-120ng/ml |
| LDH (Enzymetc Kinetic) | 431 IU/L | Female: 0-247 IU/L | IL6 | 37.5pg/ml | <4.4 pg/mL |
Table 2: Showing investigations of the patient.
Investigations
Urine aerobic bacterial culture & sensitivity (10/06/2021) and 25/6/21: No growth (Sterile) after 24 hours of aerobic incubation.
Bronchial aspirate aerobic bacterial culture & sensitivity (10/06/21): Acinetobacter baumannii grown in culture.
Blood aerobic bacterial culture & sensitivity (9/06/2021): No growth of microorganisms (sterile) after 5 days of aerobic incubation.
Blood film morphology on 08/06/2021: Hb: 11.4 g/dL, RBC: Predominantly Normocytic normochromic RBCs with few macrocytes, TLC: Within normal limits. DLC: N=86%, L=11%, M= 03%, E=00%, B=00%, Platelets: Adequate on smear. Manual count=1, 20,000/ul, No haemoparasite seen.
Serial chest Xray images shows haziness allover lung fields, ground glass appearance that started resolving later on in imaging (Figure 1). Post - covid high resolution computed tomography - Diffuse ground glass opacities with patchy areas of consolidation and interlobular septal thickening in bilateral lung parenchyma. Fibrosis with bronchiectatic changes sequelae to previous infection. Bilateral mild pneumothorax. Multiple centrilobular nodules seen predominantly in bilateral lower lobes.
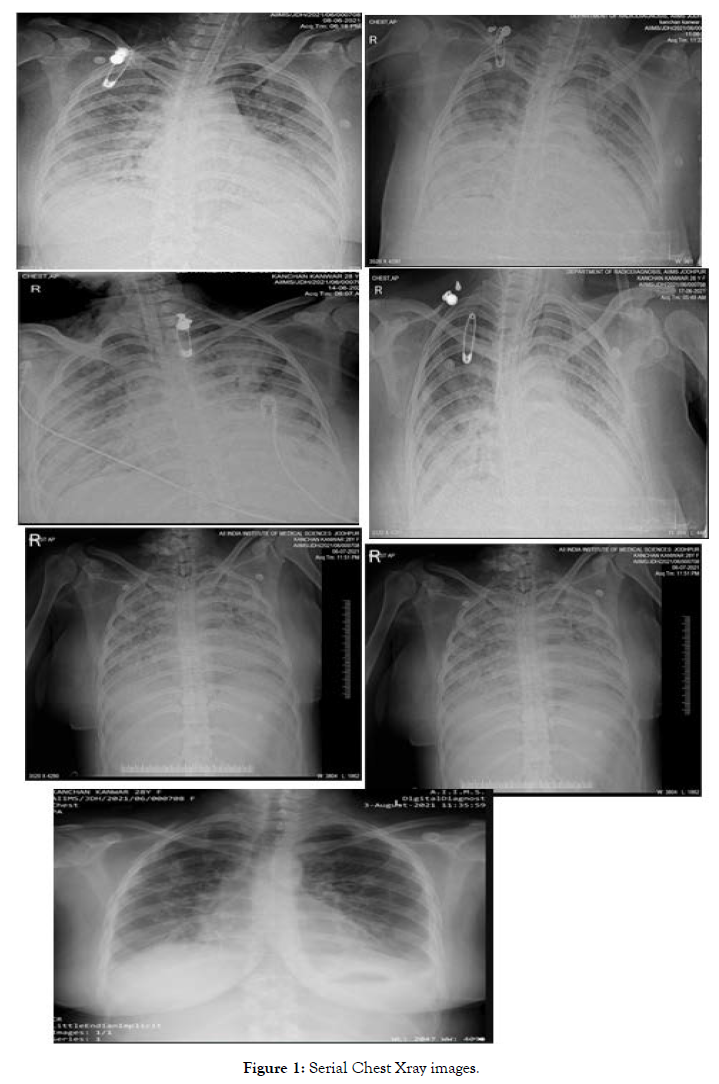
Figure 1. Serial Chest Xray images.
Ventilator Support to Weaning (AICU)
Treatment
Proning: Three sessions of proning for improving the blood oxygen saturation, each lasting for 20 hours were provided to the patient (Tables 3 and 4).
| Date | Airway | Ventilator settings | ||
|---|---|---|---|---|
| Mode | Fio2 | PEEP | ||
| 8/6/21 | Intubated | AC/VC | 100% | 12 |
| 1/6/21 | Tracheostomy | AC/VC | 100% | 12 |
| 25/6/21 | Tracheostomy | AC/VC | 100% to 35% | 12 to 10 |
| 26/6/21 | Tracheostomy tube changed | PC/VC | 45% | 10 |
| 27/6/21 | Tracheostomy | CPAP | 50% | 8 |
| 6/7/21 | Tracheostomy | T Piece | 10lit/min | |
| 7/7/21 | Tracheostomy | thermovent | 2lit/min | |
| 13/7/21 | Tracheostomy | thermovent | Off and on oxygen support | |
| 17/7/21 | Decannulation of tracheostomy done | Room air | ||
Table 3: Showing weaning of the patient.
| Date | Antibiotic | Other drugs | Infusions | Nutrition or IV fluid |
|---|---|---|---|---|
| 03/06/2021 | Tablet azithromycin 500 mg od for three days | Tab Vitamin C TDS for next 7 days Tab thyroxine 50 mcg BBF continued throughout the course |
Allowed orally | |
| 08/06/2021 | Piperacillin and tazobactam 4.5 gram, QID (for next 5 days) Metrogyl 100 mg IV TDS (for next three days) |
Inj. Pantop 40 mg OD BBF Â continued throughout Injection Low molecular weight heparin 0.6ml S/C OD continued till 17/7/2021 Iron and calcium supplementation |
Injection Noradrenaline10:1@4 ml/hr. Injection Fentanyl (500/50) @ 3ml/hr Injection Propofol @ 15ml/hr Injection Ketamine (10:1) @ 1.2 ml/hr | Ryles tube feed â?? high protein, 5 times a day. Ringer lactate 60 ml/hour |
| 16/6/2021 | Meropenum 1 gram TDS (for next 7 days)
Injection colistin 4.5 MIU BD (for next 21 days)
Injection linezolid 600 mg IV BD (for next 7 days)
Injection Minocycline 100 mg IV BD for next seven days |
Inj. Methyprednisolone 40 mg BD for next 7 days Tab thyroxine 50 mcg BBF Iron and calcium supplementation | Injection Noradrenaline10:1@4 ml/hr. Injection Fentanyl (500/50) @ 3ml/hr Injection Propofol @ 15ml/hr Injection Ketamine (10:1) @ 1.2 ml/hr. | Ryles tube feed â?? high protein, 5 times a day. Ringer lactate 60 ml/hour |
| 22/6/21 | Injection Ceftazidime avibactum 2.5 gram IV TDS for next 14 days started empirically in view of raise total leucocyte count, with no fever | Drugs continued | Injection Noradrenaline10:1@4 ml/hr. Injection Fentanyl (500/50) @ 3ml/hr Injection Propofol @ 15ml/hr | IV fluid Kabilyte @ 75 ml/hr |
| 25/6/21 | Drugs continued | Tablet Ivabradine 5 mg BD continued throughout And other Drugs continued |
Injection Ketamine (10:1) @ 1.2 ml/hr. Injection Rocuronium @ 5 ml/hr | IV fluid Kabilyte @ 75 ml/hr |
| 26/6/21 | Drugs continued | Drugs continued | Injection Ketamine (10:1) @ 1.2 ml/hr. Injection Dexmetomidate (500/50) @ 5 ml/hr. |
IV fluid Kabilyte @ 75 ml/hr |
| 27/6/21 | Drugs continued | Drugs continued | Injection Dexmetomidate (500/50) @ 5 ml/hr. | RT feed, Kabipro 3 scoops 200ml for 5 times a day |
| 6/7/21 | Drugs continued | Tablet Dabigatran 110 mg OD for 15 days Tablet pirfenidone 800 mg TDS for 30 days And other Drugs continued |
Off sedation and inotropic support | Orally allowed on semisolid diet |
Table 4: Showing Patient management.
First session done on 13/6/2021
Second session done on 18/6/2021
Third session done on 21/6/2021
Monitoring: Continuous vitals charting and monitoring. Arterial and blood glucose monitoring every 6 hourly. Routine monitoring of complete blood cells, Liver function test, renal function test, Procalcitonin, D- dimer test, Hs CRP, Chest Xray, Blood, urine and endotracheal cultures were sent time to time. Patient was kept in negative balance.
History of past illness: There was no significant history of past illness, accident, trauma, surgery, allergy or blood transfusion. Hypothyroidism present.
Family history: No history of diabetes, genetic or hereditary disease running in the family.
COVID 19 and its Mechanism
In December 2019, there was upsurge in cases of upper respiratory tract infection caused by novel coronavirus small acute respiratory syndrome Corona Virus- 2 (SARS-CoV-2) in Wuhan city, Hubei province in China. Various measures as lockdown, travel restrictions, closure of private and public firms were undertaken despite all these efforts infection travelled across the world. In March, 2020 this disease was declared as pandemic by World Health Organization. This particular virus is a single stranded, positive sense RNA. It binds to the angiotensin converting enzyme 2 receptors. This receptor is found in lung, kidney, heart and intestine. It exerts anti-inflammatory effects by regulating the maturation of angiotensin (responsible for vasoconstriction and blood pressure control). By dysregulating this receptor, SARSCoV2 causes severe lung injury by exerting pro-inflammatory action [1,2]. Other effects are shown in Figure 2.
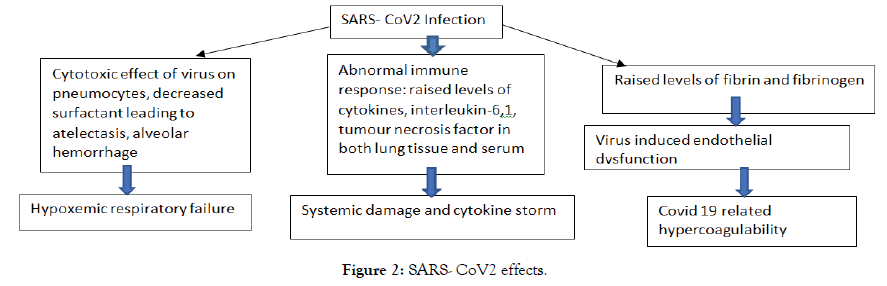
Figure 2. SARS- CoV2 effects.
COVID 19 and its risk factors: COVID 19 infection can affect anyone, but the severe form of infection has been noted in certain groups as – elderly, men, high body mass index, smoking, pregnancy, substance abuse, patients having diabetes mellitus, hypertension, cardiovascular disorders, lung disorders, renal disease, immunodeficiency, autoimmune disorders.
Environmental risk factors: included low education, low socioeconomic status, occupational risks, and contact with animals.
Virus risk factors: included transmissibility through environment, virus mutation and load [1].
Sign and symptoms: Sign and symptoms of infection may appear from 2 to 14 days after exposure. Symptoms vary from person to person. Common sign and symptoms includes - fever, cough, tiredness, muscle aches, difficulty breathing, sore throat, chills, loss of smell and taste sensation, headache, chest pain, nausea, vomiting, diarrhea, conjunctivitis, runny nose, skin rashes, exacerbation of pre-existing disorders [1-3].
Diagnostic Testing
As per ICMR, Real time Polymerase chain reaction remains the Gold standard test for COVID 19. Various open and closed RTPCR platforms as True NAT, CBNAAT are used for diagnosis. Point of care test included Standard Q COVID 19 Antigen detection kit (Table 5). It is a rapid chromatographic immunoassay used for qualitative detection of specific antigens to SARS- COV-2, requiring one nasopharyngeal swab. This test can give results within 15 minutes of putting the sample in the kit. Having high specificity 99.3% to 100% and sensitivity of 50.6% to 80.4%. Considering its high specificity and low sensitivity, it is recommended to use it in combination with RT-PCR in containment zones, health care settings and suspected individuals who tested negative.
| Mild disease | Moderate disease | Severe disease | |
|---|---|---|---|
| Symptoms | Upper respiratory tract infection without shortness of breath or hypoxia | Breathlessness, Respiratory rate of more than 24/minutes SpO2- 90- 93% on room air |
Breathlessness, Respiratory rate of more than 30/minutes SpO2- less than 90% on room air |
| Management | Home isolation and care | Ward admission, Oxygen therapy (non-rebreathing face mask), awake proning | ICU care Oxygen therapy (High frequency nasal cannula, non- invasive or invasive ventilation, proning |
| Monitoring | Temperature, spo2, | Vital sign trends, Work of breathing. Serial Chest radiograph, Computed tomography of chest, Blood tests (Blood count, kidney and liver function test, D- Dimer, C- reactive protein as per patient’s status |
Vital sign trends, Work of breathing. Serial Chest radiograph, Computed tomography of chest, Blood tests (Blood count, kidney and liver function test, D- Dimer, C- reactive protein as per patient’s status |
| Treatment | Tab Ivermectin (200 mcg/kg once a day for 3 days or Tab HCQ (400 mg BD for 1 day f/b 400 mg OD for 4 days) unless contraindicated. Inhalational steroids |
Immunomodulator therapy Anticoagulation |
Immunomodulator therapy Anticoagulation Management of co-morbid illness |
Table 5: Adapted from ICMR, AIIMS/ ICMR-COVID-19 National Task Force/Joint Monitoring Group (Dte.GHS), Ministry of Health & Family Welfare, Government of India.
C- reactive protein, D- dimer, procalcitonin, chest x-ray and CT scan are used to determine the extent and severity of illness [4]
Covid 19 and Pregnancy
As per ICMR, Pregnancy is a state of altered immunity that makes women more prone to develop severe form of infection. There is no evidence suggesting the teratogenic effect of infection. Vertical transmission of infection is probable. There is no recorded case of covid positive status of breast milk and vaginal secretions. Available data do not suggest medical termination of pregnancy or no increased risk of miscarriage because of Covid 19 infection. For breast feeding, women should maintain respiratory precautions and can continue to provide the expressed breast milk to the baby after consultation with physician [5-7].
Algorithm for management of patients with covid 19 infection
For the purpose of management, Patients with COVID 19 infection, are classified into three categories (Table 4).
Treatment modalities for COVID 19 infection
Medical management: Remdesivir (nucelotide analog) is a recommended drug for hospitalized severely ill covid 19 patients, aged 12 years and weighing at least 40 kg. Hydroxychloroquine, Lopinavir- ritonavir, tocilizumab (IL6 inhibitor for management of cytokine Strom) are useful but has failed to show effectiveness not on large scale studies has not recommended.
Oxygen therapy
Patient is provided with oxygen therapy as per requirement, if spO2 is ranging between 90-95%, then nasal prongs and oxygen face mask are used. Oxygen concentration is titrated based upon SpO2 reading [1].
High flow nasal cannula: Large bore nasal cannula used to deliver precise amount of humidified oxygen (50-60l/minute). This method provides patient with independence to eat, interact.
Non-invasive positive pressure ventilation: in this method, full facemask is applied, and continuous positive airway pressure ventilation is used to provide sufficient oxygenation to the patient.
Invasive mechanical ventilation: poses a high risk of aerosol generation and virus transmission. Rapid sequence intubation is to be carried out with utmost precaution in negative pressure rooms. Minimal bag mask ventilation and rapid inflation of pilot balloon is to be done after confirmation of endotracheal tube placement. It is used when other approaches are not improving the oxygenation of patient. Current recommendations suggest early intubation of COVID-19 patients mainly for two reasons: (1) severe hypoxemia with PaO2/FiO2 often <200 mm Hg, fulfilling Berlin criteria of moderate-to-severe acute respiratory distress syndrome (ARDS); and (2) to protect staff from viral transmission. Goal of this therapy is to improve the oxygenation while avoiding the complication of mechanical ventilation, oxygen toxicity and utilising lung protective strategies. Generally, peep- 8 cm H2O, driving pressure <15 cm H2O, and a plateau pressure to achieve tidal volumes of about 8 ml/kg predicted body weight especially in hypercapnic patients is started. The PEEP can then be gradually up-titrated to about 15 cm H2O as needed. Ventilatory parameters for covid 19 pneumonia vary from acute respiratory distress syndrome because of near normal lung compliance. Weaning is done as per patient's respiratory efforts and oxygenation status [8,9].
Extracorporeal membrane oxygenator therapy is reserved for patients suffering with severe ARDS. Maintaining a negative fluid balance, neuromuscular blokade, proning are also found to improve the respiratory failure [1].
Prone position – Patients having moderate to severe acute respiratory distress syndrome are proned. Providing prone position to the patient improves ventilation perfusion ratio, improves lung aeration, increases end expiratory lung volume, and facilitates secretion clearance [10].
Holistic nursing care for pregnant patients suffering with COVID 19
1. Teach patients and their relatives about the importance of respiratory precautions.
2. Basic physiological and psychological needs
3. Provide ventilatory care
4. Chest and limb physiotherapy
5. Medicine administration
6. Harm minimization
7. Aid in proning
8. Prevention of pressure sores
9. Prevention of deep vein thrombosis, ventilatory associated pneumonia
10. Prevention of ICU delirium
11. Maintain join alignment
12. After delivery, monitoring for bleeding per-vaginal
13. Expression of breast milk
14. Hot fomentation of breasts
15. Monitoring of blood gases and weaning as soon as possible
16. Infection prevention
17. Monitoring of Oxygen therapy
18. Assist insertion of invasive lines and further maintaining them
19. Performing nursing care procedures, with special precaution to prevent virus spillage in the atmosphere.
20. Meeting the nutritional needs
21. Encourage breast feeding as per physician’s decision.
22. Discharge instructions
23. Training to use oxygen concentrators
24. Use of incentive spirometry
25. Assessment of fetal well being
26. Neonatal resuscitation
27. New born care and assessment
Managing patients with COVID19 pneumonia is itself a huge challenge. In case of pregnant patient, the need of care increases in many folds, nurses have to keep monitoring them, assessing fetal well-being, preparing and assisting in cesarean section, weaning the patient from oxygen therapy. And most important is harmminimization while caring patient as providing prone position and preventing bedsores etc. So that the patient can progress early to normal activity of daily living.
Citation: Sharma A, Tiwari Y, Jangid J (2021) Case Study: COVID 19 in Pregnancy. J Perioper Crit Intensive Care Nurs 7: 183. doi:10.35248/2471-9870.21.7.183
Received: 09-Sep-2021 Accepted: 21-Sep-2021 Published: 28-Sep-2021 , DOI: 10.35248/2471-9870.21.7.183
Copyright: © 2021 Sharma A, et al. This is an open access article distributed under the term of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.