Lupus: Open Access
Open Access
ISSN: 2684-1630
ISSN: 2684-1630
Case Report - (2019)Volume 4, Issue 1
Antiphospholipid Syndrome (APS) is a multisystem autoimmune disorder characterized by increased risk of small vessel and venous thrombosis and/or pregnancy complications (fetal death in utero, miscarriage), with persistently elevated plasma level of antiphospholipid antibodies. Given the high mortality rate, the term (catastrophic) has been used to describe this life threating condition which is rare and represents about 1% of all APS patients, where development of fatal complication characterize the occurrence of multi organs thrombosis over a short period of time. Our case is 33 years old female patient, grand multipara, diagnosed as a case of CAPS with SLE according to the preliminary criteria for the classification of CAPS. Fulfillment of 3 out of 4 criteria is required for diagnosis of CAPS. The patient was treated with prednisolone, amlodipine, calcium carbonate, hemodialysis, intravenous immunoglobulin (IVIG) which was stopped due to development of allergic reaction. One month later, Rituximab was introduced, then her general condition improved, symptom subsided and hemodialysis was stopped with recovery of renal function. It's important to guide more efforts and studies to emphasize the role of rituximab in CAPS because it may be an effective therapeutic option for treating CAPS patients.
Catastrophic antiphospholipid syndrome; Rituximab; Intravenous immunoglobulin; Preliminary criteria
APS: Antiphospholipid Syndrome; CAPS: Catastrophic Antiphospholipid Syndrome; SLE: Systemic Lupus Erythematosus; IVIG: Intravenous Immunoglobulin; aPL: Antiphospholipid Antibodies; CS: Caesarean Section; RFT: Renal Function Test; CBC: Complete Blood Count; ABG: Arterial Blood Gases; AKI: Acute Kidney Injury; DIC: Disseminated Intravascular Coagulopathy; JVP: Jugular Venous Pressure; NCS: Nerve Conduction Studies; CIPD: Chronic Inflammatory Demyelinating Polyneuropathy; MR: Mitral Regurgitation; LA: Left Atrium; TR: Tricuspid Regurgitation; PASP: Pulmonary Arterial Systolic Pressure; IV: Intra Venous; PPI: Proton Pump Inhibitor; SC: Subcutaneous; SIRS: Systemic Inflammatory Response Syndrome
Antiphospholipid Syndrome (APS) is a multisystem autoimmune disorder, characterized by increased risk of small vessel and venous thrombosis and/or pregnancy complications (fetal death in utero, miscarriage), with persistently elevated plasma level of antiphospholipid antibodies (aPL) [1-7]. aPL include three major antibodies: Lupus anticoagulant, anticardiolipin and anti-b2 glycoprotein. Malignancy, infection and certain types of drugs may play a role in triggering APS, but the exact pathophysiology of this association is not clear yet [8]. Given the high mortality rate, the term (catastrophic) has been used to describe the life threatening condition [9] which is a rare condition and represents about 1% of all APS patients, where the development of fatal complication is characterized by the occurrence of multi organs thrombosis over a short period of time [10-12]. Currently, there are only several hundred cases of Catastrophic Antiphospholipid Syndrome (CAPS) that have been reported since the initial description [13], and there are twenty cases reported for patients with CAPS who received treatment with Rituximab in CAPS registry [14].
A 34-year-old female patient, Para VI + II, married at the age of 22 years in 2006. One year later she had her first pregnancy which was miscarried in the third trimester. Her second pregnancy was ended by emergency caesarean section (C/S) due to fetal distress (alive and well) and the third pregnancy was miscarried too. The fourth pregnancy ended by elective caesarean section at 38 weeks (alive and well). Between the fourth and fifth pregnancy she failed to conceive for 3 years without any obvious cause. The fifth pregnancy was miscarried in the first trimester, and later on, the patient suffered progressive darkening of her skin along with dysphagia to solid food and painful digits for one year. She attended a dermatology clinic on regular base, but there was no noticeable improvement.
Her sixth and last pregnancy was in 2016 when she had a poor antenatal care, and in the third trimester of her pregnancy she developed sudden shortness of breath (SOB), deterioration of level of consciousness and generalized tonic colonic convulsions. She was diagnosed with Eclampsia in Rufa'a teaching hospital and the pregnancy was terminated by emergency caesarean section.
The outcome was a female, small in size, died two weeks later. Three days after, the patient condition deteriorated rapidly and developed anuria, high blood pressure (170/110), generalized body swelling and sings of pulmonary edema. Complete blood count (CBC), renal function test (RFT)+electrolytes (Na, K), arterial blood gases (ABG), viral screening (VS) and urine analysis (UA) were performed (Tables 1A and 1B), which suggest the diagnosis of acute kidney injury and the patient was immediately referred to Medani teaching hospital for hemodialysis.
| Complete Blood Count | Renal Function Test | Arterial Blood Gases | |||
|---|---|---|---|---|---|
| Hemoglobin | 6.9 g/dl | Urea | 110 mg/dl | PH | 7.275 |
| Total white blood cells (TWBC) | 10.5 × 100 cells/mcL | Serum Creatinine | 7 mg/dl | PO2 | 80 mmHg |
| Platelets | 779 × 1000/mcL | Serum Na | 129 mg/dl | Pco2 | 26 mmHg |
| Reticulocytes | 4.10% | serum K | 5.1 mg/ dl | HCO3 | 13.2 mmol/L |
Table 1A: Results of CBC, RFT, and ABG done in Rufa'a Teaching Hospital.
| Viral Screen (rapid test) | Urine Analysis | ||
|---|---|---|---|
| Hepatitis A viral screening | Negative | Albumin | +++ |
| Hepatitis B viral screening | Negative | Pus cells | Uncountable |
| Hepatitis C viral screening | Negative | RBCS | Uncountable |
| HIV viral screening | Negative | ||
Table 1B: Result of viral screening and urine analysis.
The patient renal function improved immediately after the hemodialysis, results mentioned in table 2A and a further investigation showed AKI, DIC with normal computerized tomography scan of the brain results mentioned in table 2B (Figures 1 and 2).
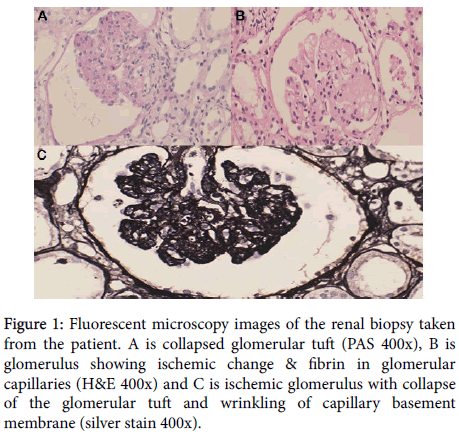
Figure 1. Fluorescent microscopy images of the renal biopsy taken from the patient. A is collapsed glomerular tuft (PAS 400x), B is glomerulus showing ischemic change & fibrin in glomerular capillaries (H&E 400x) and C is ischemic glomerulus with collapse of the glomerular tuft and wrinkling of capillary basement membrane (silver stain 400x).
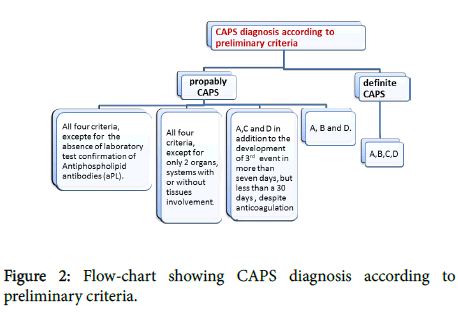
Figure 2. Flow-chart showing CAPS diagnosis according to preliminary criteria.
| RFT, C3, C4, ANA | Results |
|---|---|
| Urea | 85 mg/dl |
| serum Creatinine | 4.9 mg/dl |
| Complement component 3 (C3) | 157 mg/dl |
| Complement component 4 (C4) | 33.8 mg/dl |
| Antinuclear Antibody profile (ANA) | positive (1:80) |
| Anti-double stranded DNA (Anti-dsDNA) anti-bodies | Negative |
| Anti-neutrophil Cytoplasmic Antibody (ANCA) | Negative |
Table 2A: Results of the RFT, C3, C4, ANA after the hemodialysis in Medani Teaching Hospital.
| Imaging | Results |
|---|---|
| Abdominal ultra-sound | Right kidney: 10.3 × 3.7 |
| Left Kidney: 10.3 × 4.3 | |
| Poor cortico-medullary differentiation | |
| Feature of Acute Renal Parynechmal disease (AKI) | |
| Moderate ascites | |
| Renal biopsy | Microscopy of renal needle biopsy shows 10 glomeruli, all glomeruli shows obliteration of capillary Lumina and deposition of fibrin. |
| Silver statins shows collapse of glomerular tuft and wrinkling of glomerular basement membrane. | |
| The tubules shows hyaline casts. | |
| The blood vessels show focal fibrin deposits. | |
| The features are those of micro angiopathy consistent with disseminated Intravascular coagulation. Diagnosis: Renal Biopsy : |
|
| Disseminated Intravascular Coagulation (DIC). | |
| CT brain | Normal |
| Echocardiography | Normal Left Ventricular dimension |
| Global hypokinesia | |
| Ejection fraction: 45% | |
| Dilated left Atrium | |
| Moderate mitral regurgitation | |
| Normal right ventricular | |
| Mild TR | |
| Mild pulmonary hypertension= 35 mmHg | |
| Normal AV and PV | |
| No thrombus or vegetation nor effusion |
Table 2B: Results of the abdominal US, renal biopsy, CT brain and echocardiography of the patient in Medani teaching hospital after hemodialysis.
On 31.1.2017, the patient came to our unit in Omdurman Military hospital complaining of dysphagia, tachycardia, tachypnea, dark tough skin, blood pressure 160/110, raised JVP, massive lower limb edema, active pericardium, heaving apex, pan-systolic murmur at the apex, harsh pericardial rub all over the pericardium and bilateral crepitation up to middle chest zone.
Abdominal examination
Soft abdomen, no rigidity, no tenderness, no superficial mass, there is a longitudinal abdominal scar due to cesarean section, no organ enlargement, ascites +++, lower limb edema +++.
Central nervous system examination
She was conscious, oriented to time, place and person, normal higher functions and cranial nerves, pupils reactive to light, Fundus: disc normal + silver wiring.
Lower limb power was grade 2. Sluggish reflexes with down going planter reflex. She was unable to walk without support. Lupus anticoagulant, anti cardiolipin antibodies and B2-Glycoprotein are negative.
Nerve Conduction Studies (NCS)
NCS findings were consistent with sever sensorimotor demyelinating Poly-radiculopathy CIPD. In conclusion the patient has multi-system involvement as shown in Tables 3A and 3B.
| CBC + BFFM | RFT + electrolytes+ Rheumatologic test | LFT + enzymes | |||
|---|---|---|---|---|---|
| HB | 12.5 g/dl | Urea | 47 mg/dl | serum Albumin | 2.6 g/dl |
| MCV | 85.7 | Serum Creatinine | 3.3 mg/dl | serum Bilirubin | 1.5 mg/dl |
| PLT | 196 | serum K | 4.1 mg/dl | ALT/AST/ALP/GGT | Normal |
| TWBC | 6.3 | serum Na | 132 mg/dl | INR | 1.15 |
| BFFM | Negative | serum Calcium | 10.5 mg/dl | PT/PTT | Normal |
| ANA profile | SS-A native (60 Kda): Strong positive RO -52 : Strong positive |
||||
| Anti-ccp | Borderline | ||||
Table 3A: Test result done to the patient after admitted into Omdurman Military Hospital.
| AKI | Apical wall hypokinesia |
|---|---|
| EF= 45% | |
| Sever MR | |
| L A dilatation | |
| Sever TR | |
| PASP = 50 mmHg |
Table 3B: Results of imaging conducted to the patient in Omdurman Military Hospital.
The treatment consists of I.V. prednisolone 40 mg, I.V. PPI, I.V. furosemide 4 mg, amlodipine 5 mg, calcium carbonate 500 mg, enoxaparin SC as prophylaxis, hemodialysis twice/week and warfarin. She also received two doses of I.V. immunoglobulin but it was stopped after the patient developed an allergic reaction to it. During this period of treatment, which extends to 4 weeks, there was no improvement, and then a 500 mg infusion of Rituximab was given to the patient as one dose/14 days, where she responded well to the treatment after receiving 4 doses of the drug in total. In less than one month after receiving the Rituximab treatment, her general condition was improved, the dysphagia subsided, her lower limb power became grade 4 and she started to walk without support. Also, her lower limb edema was subsided, urine output reached 200 ml/day and her skin went back to its normal condition. The patient continued in hemodialysis (2-sessions/week) for 9 months, and now she is off dialysis. Last RFT showed: Urea 58 mg/dl, Creatinine 2.1 mg/dl, normal electrolytes.
Pathophysiology of CAPS
The pathophysiology of catastrophic antiphospholipid syndrome is an enigma, and until now is not completely understood. Several mechanisms have been advocated, such as the infection theory, molecular mimicry and endothelium activation in the microvasculature and micro-vascular occlusions [15]. It has been proposed that the vascular occlusions are the leading cause that feeds the ongoing thrombosis [16]. It has also been assumed that thrombi are persistently produced and elevation in plasminogen activator inhibitor type 1 diminishes fibrinolysis. This is associated with utilization of the essential anticoagulant proteins such as anti-thrombin and protein C. The micro-vascular occlusion causes wide tissue necrosis resulting in systemic inflammatory response syndrome (SIRS), along with enormous cytokine release from damaged and necrotic tissues [17]. The activated complement system products (C5a, C3b and iC3B), together with pro-inflammatory cytokines and aPL antibodies activate endothelial cells and hence provide a signal that stimulates the release of tissue factors and adhesion molecules. These molecules play a major role in increasing the number of leukocytes and adhesion of the platelets to the vascular endothelium, leading to micro-thrombi formation and local liberation of toxic mediators such as free radicals and proteases. Interaction of the aPL antibodies with cells results in diffuse micro-vasculopathy and multi-organ damage that characterize catastrophic antiphospholipid syndrome (CAPS) [15-18].
Criteria for CAPS diagnosis
Preliminary criteria for the classification of CAPS: 1) Evidence of involvement of 3 or more organs, systems and/or tissues. 2) Development of manifestations simultaneously or in less than a week. 3) Confirmation by histopathology of small vessel occlusion in at least one organ or tissue. 4) Laboratory confirmation of the presence of Antiphospholipid antibodies (Lupus anticoagulant and/or Anticardiolipin antibodies) (Figure 2).
From the above preliminary criteria of CAPS classification, our patient fulfills 3 of the 4 criteria. She had acute renal failure diagnosed by abdominal ultrasound and renal profile, chronic inflammatory demyelinating polyneuropathy according to the NCS, cardiac valves involvement confirmed by echocardiography and a revealed DIC in a renal biopsy as shown in Table 4.
| Diagnosis of probably CAPS in our patient | ||
|---|---|---|
| Fulfillment of the first and second criteria | Involvement of 3 or more systems or tissues or organs (Criteria 1), less than week or simultaneously (Criteria 2) | |
| Kidney | AKI | |
| CVS | sever MR, sever TR, PHTN | |
| CNS | CIPD | |
| Skin | Ischemic necrosis | |
| Fulfillment of third criteria | histopathology conformation of small vessel occlusion in one organ at least (Criteria 3) | |
| Renal biopsy | DIC | |
| Does not Fulfill the fourth criterion | Lab confirmation of aPLs (Criteria 4) | |
| Lupus anticoagulant | ||
| anti-cardiolipin antibodies | Negative | |
| β2-Glycoprotein | ||
Table 4: Illustration of the CAPS criteria shown in our patient who fits the diagnosis of probably CAPS.
The clinical manifestation of CAPS varies between all systems as shown in Figure 3.
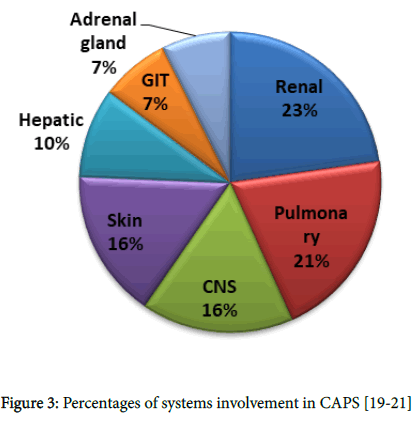
Figure 3. Percentages of systems involvement in CAPS [19-21]
CAPS is a unique form of APS described for the first time in 1992 by Asherson [22]. The optimal therapeutic regimen for catastrophic antiphospholipid syndrome (CAPS) is unknown, and the current management guidelines propose early diagnosis along with aggressive therapies which is essential to avoid fatal complications. Those therapies include intravenous heparin and methylprednisolone in the first line of treatment, plasmapheresis and IVIG in the second line of treatment if no contraindications, followed by cyclophosphamide with or without rituximab specially if associated with SLE [23,24]. All of these drugs have been part of our treatment plan for the patient. Regarding rituximab, there are no studies, guidelines or formal recommendations for it to be used in CAPS treatment, and hence it might be important to guide more efforts and studies to emphasize its role in CAPS treatment.
In the literature, there are plenty of studies and case reports about rituximab being used in treatment of other immunological and oncological diseases such rheumatoid arthritis, psoriasis and non- Hodgkin lymphoma. But in these studies, there are only 11 reports of 13 patients with catastrophic antiphospholipid syndrome treated with rituximab, and they all showed promising results [14,25-35]. Two of these cases had CAPS associated with SLE [28,31], and both met the criteria for probable CAPS but not definite CAPS. Our patient is the first case to be reported with catastrophic anti-phospholipid syndrome (CAPS) associated with systemic lupus erythematosus (SLE) and treated by rituximab (RTX) in Africa. Patients with SLE associated with CAPS have higher death rate than others with primary CAPS. They also show high frequency of cerebrovascular diseases and cardiac valve involvement [36], as evidenced in our patient. We believe that the prolonged course of the disease for our patient had resulted in development of an infection that had probably participated in triggering the patho-genetic mechanisms for CAPS development, and the hypersensitivity reaction of our patient against the I.V. immunoglobulin played a major role in reducing the effectiveness of the therapeutic protocol, and therefore, adding rituximab was the best alternative treatment option.
Regarding the sero-negative antiphospholipid antibodies (aPLs), there are two rare conditions where it shows false result. The first one is based on the size of the clots, where a large thrombus can consume the antibodies in the clots formation and hence the result will be negative (repeating the test three months after the thrombotic event will show a positive result). The second one is when antibodies are directed to some antigens, creating a complex that cannot be tested in the lab.
Rituximab (RTX)
It is an intravenously administered biological drug (chimeric anti- CD20 monoclonal antibody), and its mechanism of action is selective reduction of B lymphocyte.
RTX works by selectively binds to the CD20 antigen in B-cells surface, leading to activation of the cellular mechanism that initiates Blymphocyte cytotoxicity [37].
It triggers the cell death when it binding to the protein CD20 [38]. It was first approved for the treatment of B-cells lymphoma and then for RA and ANCA associated vasculitis [39,40]. Currently, clinical trials propose rituximab as highly effective drug in treatment of lupus nephritis and its effectiveness remains controversial [41].
This case represents the first reported patient of catastrophic antiphospholipid syndrome associated with SLE, treated by rituximab in Africa and Middle East. In this case, a combined management protocol of glucocorticoids, antibiotics and anticoagulation with rituximab shown to be highly effective. The right timing for administering rituximab is still uncertain, and whether its administration at an earlier stage could alter or change disease progression is also unknown. More investigations and studies are needed to augment the effectiveness of this drug in treatment of CAPS and defining the right timing for administration and optimal dosing regimen to be followed.
It is important to identify the possible differences in the effectiveness of rituximab in treating patients of CAPS associated with SLE and patients of primary CAPS in order to determine the possible prognostic factors that could affect the therapeutic decisions and results.
All authors declare that there is no conflict of Interests.
A written informed consent was obtained from the patient for the purpose of this study.
All authors declared that, no fund or financial aid has been received for this study.
The study was supervised by Dr El nour Mohammed El agib, Rheumatologist.
The patient treatment and regular follow up during all the course of the disease was carefully applied by Dr. Noha Ibrahim Ahmed Eltahir, a rheumatology fellow in Dr El Nour M. El agib unit, along with Dr. Ziryab Imad Taha Mahmoud, Dr. Mohammed Elmujtba Adam essa and Dr. Mutwaly Defealla Yousif Haron who also contributed by the scientific writing.
Dr. Habiballa Hago Mohamed Yousif, a nephrologist, took the decision and performed the renal tissue biopsy, and Dr. Azza A. Abdelsatir is the histo-pathologist.
Citation: Elagib ME, Eltahir NIA, Adam MEAE, Mahmoud ZIT, Yousif HHM, et al. (2019) Catastrophic Antiphospholipid Syndrome in Combination with SLE Treated by Rituximab: A Case Report and Literature Review. Lupus Open Access 4: 137.
Received: 02-Mar-2019 Accepted: 11-Mar-2019 Published: 21-Mar-2019
Copyright: © 2019 Elagib ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.