Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Case Report - (2023)Volume 12, Issue 1
Central diabetes insipidus has been described as a rare complication of acute myeloid leukemia in adult patients. This case report details a case of a 6 month old infant newly diagnosed with AML that was complicated by central diabetes insipidus and concurrent cerebral salt wasting syndrome. As far as we know this is one of the first cases of concurrent central diabetes insipidus and cerebral salt wasting syndrome in the setting of AML in a pediatric patient. Our case documented a fluctuation between DI and CSW in a newborn with freshly diagnosed AML, necessitating intensive monitoring of her serum Na and osmolality, urine output, Na and osmolality. Using vasopressin was difficult owing to the frequent fluctuations in the given levels within 24 hours. Importantly, her brain MRI findings in this case were normal. A similar instance was described in adults, but with aberrant brain MRI results.
Diabetes insipidus; Cerebral salt wasting syndrome; Acute myeloid leukemia; MRI; Osmolality
Acute myeloid leukemia has been shown to have a very rare association with the development of central diabetes insipidus. In other case reports, there was shown to be an association with the development of central diabetes insipidus and AML when the individual has abnormalities with chromosome 3 or 7 [1]. The proposed process behind the pathologic origin of central diabetes insipidus is through leukemic cell infiltration of the neurohypophysis [2]. There have been other case reports of combined Cerebral Salt Wasting and Central Diabetes Insipidus in the setting of neurosurgery or traum [3].
We report a case where an individual was found to have AML with a chromosomal 6 abnormality that later developed central diabetes insipidus that alternated with cerebral salt wasting syndrome.
A previously healthy 6 month old female infant, initially presented with new persistent fever and fatigue for three weeks. She was admitted for further workup and found to have macrocytic anemia (8.4 g/dL), leukocytosis 29.2 x10E3/uL with 23.9 x10E3/uL lymphoblasts, and hypernatremia (149 mmol/L). Further workup including a blood smear showed an increase in blasts associated with a megakaryoblastic differentiation. On day two of admission, she developed polyuria, hypernatremia 156 mmol/L, and an increase in serum osmolality to 318 all of which are characteristic of the development of Central Diabetes Insipidus (CDI). She was started on vasopressin which helped improve her serum sodium and had a urine output. A taper of vasopressin was started and her serum sodium began to rise again so vasopressin was restarted. She then began to have a decrease in serum sodium and urine output so vasopressin was weaned gradually. During this time of hypernatremia and high urine output, monitoring her urine Na and urine osmolality reflected DI. In the next 48 hours, she developed hyponatremia to 120 mmol/L and hypokalemia to 2.1 mmol/L and had a urine output of 14.7 cc/kg/hr and all of which are characteristic of the development of Cerebral Salt Wasting Syndrome (CSW). The child fluctuation between DI and CSW occurred over two weeks where she required vasopressin therapy while in DI to Na and urine output replacement while in CSW until she was to be stabilized on desmopressin (DDVAP) subcutaneous injection (Figure 1) of note, the brain MRI was reported normal with no identifiable neurohypophysis.
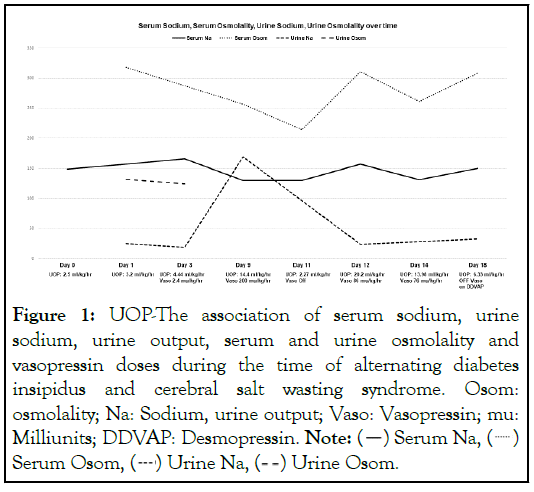
Figure 1: UOP-The association of serum sodium, urine sodium, urine output, serum and urine osmolality and vasopressin doses during the time of alternating diabetes insipidus and cerebral salt wasting syndrome. Osom: osmolality; Na: Sodium, urine output; Vaso: Vasopressin; mu: Milliunits; DDVAP: Desmopressin. Note:  Serum Na,
Serum Na,  Serum Osom,
Serum Osom,  Urine Na,
Urine Na,  Urine Osom.
Urine Osom.
During this time, chromosome analysis showed trisomy 6 and a reciprocal translocation between the short arm of chromosome 11 and the long arm of chromosome 17. The breakpoint for chromosome 11 at 11p15 indicated involvement of the NUP98 gene. According to the WHO classification 5th edition, the NUP98 rearrangement is the key genetic abnormality leading to the development of Acute Myeloid leukemia. Bone marrow aspiration showed that she had non-down syndrome-associated pediatric megakaryoblastic acute myeloid leukemia. An MRI of the brain stem with and without contrast was ordered and showed no neurohypophysis, normal T1 bright spot, and a normal sized pituitary gland. After stabilization she was given rasburicase and initial chemotherapy regimen consisting of cytarabine, daunorubicin, etoposide, and gemtuzumab. Currently, her central DI is being managed through subcutaneous DDAVP injections. After her initial chemotherapy regimen, she underwent flow cytometry and a bone marrow aspiration which showed concerns for residual disease which require bone marrow transplant and HLA testing in her mother.
AML typically follows a bimodal distribution occurring early in life or later in life. Individuals who develop AML typically have an associated genetic abnormality that can direct therapy and help determine possible prognosis [1]. In some pediatric populations, there have been some case reports that show an association between monosomy 7 and the development of a myeloid leukemia [1]. Individuals with these certain genetic abnormalities like monosomy 7 and have AML are at an increased risk of developing central diabetes insipidus and potentially the development of concurrent cerebral salt wasting [1].
The development of central diabetes insipidus with AML usually carries poor prognostic factors [4]. The theory as to why individuals with AML can develop central diabetes insipidus is thought to be from leukemic infiltration of the pituitary gland [2]. As seen in a case report by Surapolchai, MRI of the brain will show a loss of the bright spot in the posterior pituitary due to the leukemic infiltration which causes the subsequent decrease in production of ADH [1]. This loss of ADH is what drives the development of central diabetes insipidus [2]. Whereas other causes of central diabetes insipidus was shown to be from tumors or trauma to the brain [1,3].
The development of cerebral salt wasting combined with central diabetes insipidus was shown in one case report by Jim-Lin, but this occurred in individuals with trauma or tumors to the brain [1,3,5]. The development of cerebral salt wasting syndrome occurs when there is hyponatremia with elevated urine sodium and hypovolemia [3]. With the development of cerebral salt wasting syndrome in the setting of central diabetes insipidus there could be iatrogenic SIADH due to vasopressin or desmopressin administration [5]. However, an individual with cerebral salt wasting syndrome will show substantial polyuria and natriuresis [5,3]. The development of cerebral salt wasting combined with central diabetes insipidus in the setting of AML carry very poor prognostic factors [1,3].
In summary, we presented a pediatric patient who was diagnosed with AML with development of central diabetes insipidus and later concurrent cerebral salt wasting syndrome. There has been a reports of an adults with AML and later developed central diabetes insipidus [4]. It is important to recognize that central diabetes insipidus and also cerebral salt wasting syndrome can occur in the pediatric population who have AML [6]. The sooner central diabetes insipidus and cerebral salt wasting are identified as possible differential diagnoses, the sooner treatment can begin as both pathologies require different treatment plans.
Our case reported fluctuation between DI and CSW in a newly diagnosed AML in an infant, and required an aggressive monitoring of her serum Na and osmolality, urine output, Na and osmolality. Utilizing vasopressin was challenging due to the frequent changes in the mentioned values sometime within 24 hours. Notably in this case, her brain MRI findings were normal. Similar case was reported in adults, yet with abnormal findings on brain MRI.
Authors declare there has no conflict of interest.
None
Citation: Sky K, Hadid S (2023) Central Diabetes Insipidus Alternating with Cerebral Salt Wasting Syndrome in an Infant with an Acute Myeloid Leukemia. Endocrinol Metab Syndr. 12:372.
Received: 07-Mar-2023, Manuscript No. EMS-23-22140; Editor assigned: 09-Mar-2023, Pre QC No. EMS-23-22140; Reviewed: 23-Mar-2023, QC No. EMS-23-22140; Revised: 03-Apr-2023, Manuscript No. EMS-23-22140; Published: 10-Apr-2023 , DOI: 10.35248/2161-1017.23.12.372
Copyright: © 2023 Sky K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.