Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2022)Volume 11, Issue 10
Objective: The impact of COVID-19 pandemic on student mental health has been an increasing concern in higher education. Some studies suggest that university students’ mental health have worsened, whereas other report that mental health remain stable, or even improvement during lockdown. Because of a lack of prospective studies with pre-during-post lockdown assessments, the long-term consequences of lockdown on students’ mental health are unknown.
Methods: This prospective study investigated short and long-term changes in mental health during the Chinese lockdown monitored across fourteen months from October 2019 to December 2020 measuring depressive and psychiatric symptoms, psychological resilience, perceived stress, suicidal ideation, and self-harm behavior. Self-report data was collected from 282 undergraduates (161 females) at three-time points: autumn 2019 (baseline, pre-pandemic), the sixth week of lockdown, and 10 months post-lockdown. The linear mixed model was used to examine the overall change in depression over time.
Results: Compared with before lockdown, an overall decrease in depression was found during and post-lockdown. Psychological resilience significantly increased whereas perceived stress significantly decreased 10 months after lockdown. There were no significant changes in psychotic symptoms and self-harm over time. Individuals with high level of psychotic symptoms and those with self-harm had less decrease in depression than those with without these conditions. No difference was observed for other subgroups.
Conclusion: The COVID-19 lockdown could have brought benefits rather than negative influences on mental health in Chinese university students. Such changes have important implications on how we can foster positive youth development in times of crisis.
Stress-related growth; Resilience; Positive changes; Depression; Lockdown
Higher education student mental health has been a growing concern, with a 63% increase in major depressive episodes in the last decade [1]. This is especially concerning when considering that the COVID-19 pandemic introduced increased stress levels due to transition to remote learning, social isolation, and career uncertainty [2]. In China, over 37 million university students were impacted psychologically; whose depression rates have increased 5.3% during lockdown [3]. In Western countries, levels of depression and anxiety in undergraduate students were also found to heighten due to lockdown restrictions [4-6]. However, most of these prior studies were cross-sectionally designed and mainly explored the short-term effects of the pandemic. In order to identify pandemic-induced changes, studies covering the entire period of the pandemic from before to outbreak, to after lockdown would be particularly beneficial.
Contrary to concerns raised early in the pandemic, longitudinal studies on individual’s mental health, including ours [7], points to a more mixed picture, with no or little change in depression and anxiety compared to pre-pandemic levels [8-10], or an initial increase and subsequently decline [11,12], or even an improvement in mental health following lockdown [13,14]. A meta-analysis of 25 longitudinal studies in general population samples showed that the negative impact of the COVID-19 lockdown was small in average and positive emotions remained unaffected, suggesting that most people have been largely unaffected by the global public crisis [15]. Similarly, another meta-analysis based on 65 longitudinal cohort studies found surprising adaptation and resilience capacity, showing an initial increase in incidence of mental health symptoms and a quick decrease to pre-pandemic level [16]. More encouraging news stems from patients with pre-existing mental health conditions, showing the stability or a slight decrease in depression, anxiety, worry and loneliness over the COVID-19 pandemic [17-19]. Of note, some studies also unexpectedly reported the COVID-19 lockdown could have brought benefits on mental health and positive changes [13,14]. For example, Li et al.(2021) found that depression, insomnia symptom and sleep problems were the highest before pandemic, then decreased during home confinement and continued to decline after the lockdown. Qu et al.(2022) also reported that the incidence of anxiety and depression in adolescents were lower after two months of home confinement than that before confinement. Positive changes in some life outcomes have also proved during COVID-19, such as better sleep quality, less unhealthy behavior and increased family connections [20,21]. Hence, it is still debated how mental health symptoms evolve over the time of lockdown, whether it has worsened or improved during lockdown, in particular, whether any changes continue to present or quickly vanish after the lifting of lockdown.
According to resilience perspective, there comes a building effect which fosters personal growth and improves their mental health when individuals can use the crisis in a transformative way to develop new coping skills, broadened perspectives and new personal resources [22]. For example, Waters and colleagues found that positive interpretation predicted levels of stress-related growth during the global pandemic as this flexible cognition was an important coping process that built and expanded personal growth [23]. A narrative study postulated that successfully navigating the challenges of COVID-19 would strengthen individuals’ family cohesion, social connections, personal growth and mental health [24]. Stress-related growth theory proposed that acute stress and pandemics could stimulate an improvement in psychological and social functioning, such as family and social connectedness, trustworthiness and sharing behavior [25,26]. These frameworks together suggest that people show surprising resilience capacity when they are faced with uncertainty and crisis. However, the pattern of adaptive functioning, or resilience is likely to be shaped by distinct individual characteristics, and the socio-political context in different lockdown restrictions [27]. Unlike in many Western countries, there was not multiple national lockdowns with “Dynamic COVID-zero” strategy after experiencing the first strict lockdown in the spring of 2020. Local strict lockdowns balance the prevention and control of this disease with socioeconomic stability [28]. Individuals have been challenged to learn new ways of communicating with others, and find new methods to remain flexible and resilient during uncertain times. Cultural beliefs about adversity can also influence how people adjust to COVID-19 [29]. In Confucian thoughts, adversity is an opportunity for self-cultivation of virtues, and Chinese people may have strong forbearance and perseverance on severe limitations on capacity for in-person social interaction whereas people in an open culture might not be tolerant [30,31]. This highlights the need to consider country-specific factors when investigating and interpreting the mental health effects of the pandemic.
The present study was to investigate the immediate and long-term impact of the national lockdown on mental health in university students across fourteen months from October 2019 to December 2020 over three time points: pre-, during and post-lockdown. It was hypothesized there would be a short- and long-term negative impact of the pandemic on mental health symptoms in university students. There is an urgent need to identify mechanisms underlying possible changes in mental health in response to COVID-19. The secondary aim was to investigate the impact of different individual and psychosocial risk factors on changes in mental health. It was hypothesized these risk factors would show a stronger association with increased depressive symptoms.
Participants
The current study was based on data from the on-going project examining on mental health and behaviour in university students. The first wave of the project was conducted during October 2019 at time point 1 (baseline, pre-lockdown), where 282 firstyear undergraduate psychology/education students completed a battery of online questionnaires assessing their non-suicidal selfinjury, resilience and perceived stress. At the beginning of the COVID-19 outbreak, an invitation for the follow-up survey was sent after the Chinese lockdown began (time point 2; lockdown). The second survey (N=202) was completed online from 1 March to 30 April 2020 through online survey platform (www.wjx.com), 82 participants did not respond the invitation. The third survey (N=270) was conducted from 1 November to 30 December 2020, university resumption and 10 months after lockdown (time point 3; post-lockdown). The final sample (N=282) with multiple imputation of missing data comprised of 161 (57%) females, with a mean age of 19.81 (SD=2.08). Ethics approval was obtained from the Institutional Review Board of the Hunan Agricultural University (2020-026) and informed consent procedures were followed throughout.
Measure
Sociodemographic and health variables were provided: (1) gender, (2) age, (3) place of residency (city, country), (4) monthly household income (high, average, low), (5) single parent household (yes, no), (6) pre-existing diagnosed mental illness (yes, no), (7) family history on mental health illness (yes, no), (8) suicidal ideation (yes, no).
Depression was assessed by the Center for Epidemiologic Studies Depression Scale [32] and self-harm with the non-suicidal self-injury scale [33]. Psychotic symptoms were measured by the Prodromal Questionnaire [34]. Psychological resilience was measured by the Connor-Davidson Resilience Scale [35] and perceived stress was measured by the Perceived Stress Scale [36]. These assessments were administered each wave.
Lockdown-specific questions were asked to assess specific stress experienced due to lockdown restrictions at T2. The following 17 items were developed: 1) Restrictions on the free movement of citizens, 2) Mandatory testing of temperature and wearing masks in public, 3) Closed residential community, 4) Unable to meet friends and relatives, 5) Widespread news and information about the new virus, 6) Mandatory reported health situation every day, 7) Privacy exposure, 8) Lack of supplies of personal protective equipment (PPE) i.e. masks or protective clothes, 9) Healthcare staffs infection and risk of hospitals being overwhelmed, 10) School closures, 11) Learning online rather than face-to-face,12) Being unable to complaints in public, 13) Friends and family being diagnosed, 14) Confirmed cases in your area, 15) Family’s fears of COVID-19 disease, 16) Increasing daily incidence, 17) Increasing daily deaths toll. Each participant was required to assess the influence of these events from 1 (not at all) to 5 (very severe), with higher total scores indicating a greater number of stressful experiences.
Statistical analysis
Missing Completely At Random (MCAR) test was firstly used to test the nature of our missing data over time. Further, independent samples t-tests were used to examine whether university students who completed all waves differed from those with missing data. Multiple imputations were conducted to handle missing data. The number of imputations was increased until the fraction of missing information/imputations M=.01 reached a value which was <10% of the standard error of the estimate. 30 imputations were sufficient to meet this criterion in present study. All data (n=282) included in the following analysis. Firstly, to assess the potential impact of the pandemic on mental health, the linear mixed model was used to examine the overall change in depression, psychotic symptoms, selfharm, psychological resilience and perceived stress over time (pre- , during and post-lockdown). Bonferroni correction was used to correct multiple comparisons. Secondly, interactions between time and different predefined subgroups (e.g., single-parent household, family history of mental health illness, household income, and suicidal ideation) pre-lockdown were used to identify heterogeneity in the effects of COVID-19pandemic. Baseline psychotic symptoms, self-harm, perceived stress, resilience and COVID- 19related stressors during lockdown were transformed respectively into a categorical variable with “high” and “low” groups. Statistical analysis was performed using SPSS 27.0 (IBM Corp, released 2019).
Across the three timepoints (pre-, during and post-lockdown), the percentage of participants with a clinically significant level of depression (16.7%, 11.3%, and 12.3%) did not differ, 2 (2)=2.90, p=.234. Significant higher depression scores at baseline were observed for individuals who reported self-harm behaviour, suicidal ideation, psychotic symptoms, low psychological resilience, high perceived stress, and high the COVID-19 related stressors having a family history of mental health illness, compared with those who did not report these risk factors (all p-values<.001). No significant difference was observed for age, gender, place of residency, household income and single-parent household.
The mixed linear model found the main effect of time was significant when controlling for age, gender and place of residency (F (2,564)=3.44, p=.033), showing a significant decrease in the scores for depressive symptoms from before to during, to 10 months after lockdown. Bonferroni-corrected pairwise post-hoc comparisons showed that depression both during- and post-lockdown significantly lowered compared with before lockdown, but depression showed no difference between during and post-lockdown, see Table 1. Level of psychological resilience was the highest whereas perceived stress was the lowest after lockdown. However, psychological resilience and perceived stress during lockdown stayed the same level with pre-lockdown. There were no significant changes in psychotic symptoms and self-harm over time in Figure 1.
| Characteristics | Time point | Mean | SD | F | η2 | p | Bonferroni comparison |
|---|---|---|---|---|---|---|---|
| Depression | Before | 12.82 | 8.77 | 7.04 | 0.03 | 0.001 | T3>T1, T2>T1, T2=T3 |
| Outbreak | 10.96 | 7.58 | |||||
| After | 10.94 | 8.3 | |||||
| Resilience | Before | 29.35 | 8.61 | 10.43 | 0.03 | <.001 | T3>T1, T3>T2, T1=T2 |
| Outbreak | 29.28 | 8.87 | |||||
| After | 31.26 | 8.00 | |||||
| Perceived Stress | Before | 25.59 | 6.12 | 22.33 | 0.11 | <.001 | T3<T1, T3<T2, T1=T2 |
| Outbreak | 24.69 | 6.33 | |||||
| After | 23.07 | 6.73 | |||||
| Psychotic symptoms | Before | 3.28 | 3.00 | 2.61 | 0.01 | 0.078 | T1=T2=T3 |
| Outbreak | 2.86 | 2.98 | |||||
| After | 3.23 | 2.89 | |||||
| Self-harm | Before | 0.85 | 2.92 | 0.95 | 0.00 | 0.36 | T1=T2=T3 |
| Outbreak | 0.81 | 2.687 | |||||
| After | 1.03 | 3.25 |
Note: Depression: The Centre for Epidemiologic Studies Depression Scale.
Resilience: The Connor-Davidson Resilience Scale.
Perceived stress: The Perceived Stress scale.
Psychotic symptoms: The Prodromal Questionnaire.
Self-harm: The Non-Suicidal Self-injury scale.
Table 1: Repeated ANOVA analysis of all variables.
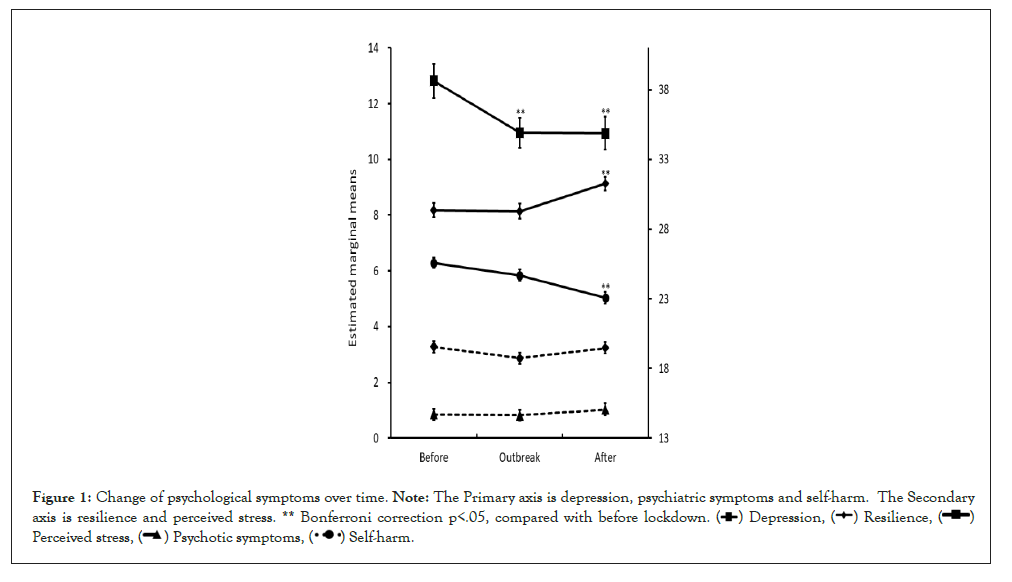
Figure 1: Change of psychological symptoms over time. Note: The Primary axis is depression, psychiatric symptoms and self-harm. The Secondary
axis is resilience and perceived stress. ** Bonferroni correction p<.05, compared with before lockdown. 

To further examine difference change in depression associated with the pandemic between different subgroups with a higher risk of mental health problems, the interaction of time with a set of predefined risk factors were entered the mixed linear model. As shown in Table 2, individuals with high level of psychotic symptom showed a less decrease in depressive symptoms than the low-level group. Similarly, individuals with self-harm behaviour showed a less decrease in depressive symptoms than those without self-harm. No meaningful difference was observed for other subgroups, including gender, place of residence, family history of mental health illness, household income, single-parent household, and suicidal ideation, perceived stress, psychological resilience and COVID-19 related stressors.
| Characteristic properties | Estimate | t | p | 95%CL |
|---|---|---|---|---|
| Interactions with time (difference in change from T1 to T3) | ||||
| Single-parent household (no) | -0.11 | -0.15 | 0.883 | -1.51, 1.30 |
| Family history of mental health illness (no) | 0.52 | 0.66 | 0.507 | -1.02, 2.05 |
| Household income (high) | [Reference] | - | - | - |
| Low | 0.10 | 0.18 | 0.857 | -0.98, 1.18 |
| Average | 0.56 | 1.46 | 0.146 | -0.20, 1.31 |
| Suicidal ideation (no) | -0.40 | -0.46 | 0.647 | -2.11, 1.32 |
| COVID-19 stressor (low) | -0.21 | -0.55 | 0.58 | -0.95, 0.53 |
| Resilience (low) | 0.31 | 1.01 | 0.315 | -0.30, 0.93 |
| Psychotic symptoms (low) | -1.30 | -3.65 | <.001 | -1.99, -0.60 |
| Self-harm (low) | -3.26 | -7.79 | <.001 | -4.08, -2.44 |
| Perceived stress (low) | 0.02 | 0.06 | 0.951 | -0.52, 0.55 |
Note: Depression: The Centre for epidemiologic studies depression Scale, with 20 score or more indicating a clinically significant level of depression.
Psychotic symptoms: The prodromal questionnaire, with 6 score or more indicating clinically significant level of psychotic symptoms.
Self-harm: The non-suicidal self-injury scale, with 1 score or more indicating self-injury risk.
Resilience: The Connor-Davidson resilience Scale; with 22 score or more indicating high psychological resilience.
Perceived stress: The perceived stress scale, with 26 score or more indicating high perceived stress.
Table 2: Mixed model predicting changes in depressive symptoms associated with the pandemic.
Contrary to our expectation, the present study found an overall decrease in depressive symptoms from the early stages of lockdown to 10 months after lockdown compared with in the previous year, whereas psychotic symptoms and self-harm not being much affected by the ongoing crisis. Interestingly, the improvement pattern in psychological resilience and perceived stress delayed after lockdown. This suggested that mental health of Chinese students saw improvements during lockdown, and the benefit became larger 10 months after lockdown, suggesting that the Chinese lockdown did not worse students’ mental health, but showed remarkable signs of positive psychological function in the long term.
Previous studies found most individuals were sufficiently able to cope with the pandemic and showed surprisingly resilient during pandemic [15,16]. In the Netherlands, for example, a longitudinal study reported no increase in anxiety and depressive symptoms from before to after the outbreak [37]. In a Chinese general population study, no negative longitudinal changes were found in anxiety and depression levels [9]. A study from Japan found that suicide rates among children and adolescent were not significantly different from the previous two years during the school closure time [38]. There is also convincing evidence showing surprising ability to bounce back and adapt following lockdown. In the UK, the highest levels of depression and anxiety occurred in the early stages of lockdown but subsequently declined as lockdown continued [11]. In Spain, after the lifting of lockdown, depressive symptoms rapidly decreased after an initial increase during the initial outbreak [39]. Similar to the present results, several longitudinal studies have proved that the COVID-19 lockdown could have brought benefits influences on individual’s mental health. In Chinese adolescents, depression, insomnia symptom and sleep problems were decreased during home confinement and continued to decline after the lifting of lockdown [13,14]. In our previous study, Chinese children and adolescents reported significant decrease in different types of child maltreatment during lockdown [7]. Similar observations emerged in Chinese adults, the lockdown did not bring damaging psychological effects, some benefits on the contrary were found including reduced aggressive behaviour, less drinking and smoking, and sleeping problems improvement [20]. In American, adults did not show significant changes in loneliness but rather increased perceived support from family and friends across the whole lockdown [40]. In Scotland, people experienced many positive changes such as improved family relationships, increase in exercise or physical activity, doing more enjoyable things, and being more appreciative of things usually taken for granted [21]. These convincing evidence highlight that increased resilience building has occurred in face of the unprecedented pandemic, and most individuals has been either largely unaffected or is even doing better during the pandemic [41].
It is possible that the improvements in mental health are associated with positive functioning growth after acute adversity. According to the theoretical model for psychosocial gains from adversity [42], people can experience marked psychological improvement following different forms of adversity including better relationships, increased psychological well-being, more personal strength, greater appreciation for life, renewed sense of life’s possibility, and deepened spiritual connection. Indeed, the majority of parents reported the COVID-19 lockdown improved relationship with their children [43], including taking more time with their children, showing more physical affection, warmth and love toward their children [44], and experiencing stronger relationship (e.g., sharing laughter, being loved and kind [21]. In China, parents have more intensive interaction with their children, especially in the case of one-child families [45]. When staying home, university students may develop strong family cohesion, which they tend to experience higher levels of psychological safety, more extensive collaboration, greater unit attachment, and higher unit-level resilience [46]. Such positive connections as social boosters may contribute to students’ capacities to endure, cope and potentially thrive during this global pandemic [47]. There were prior evidence that disasters and pandemics activated people efforts to connect with others and promoted meaningful social interactions. After 9/11, for example, Americans spent more time with friends and family and increased trust in neighbours [48]. During SARS epidemic, people in Hongkong exhibited social connectedness growth including taking greater care of family members and giving friends more support [49]. These beneficial effects of acute adversity on social relationships strengthen individual’s psychological resources and capacities to buffer against distress and bolster mental health. Mancini also proposed that the more meaningful social connections and cooperative social environment in the face of the difficult feelings, the more resilient would be in the long term. Prior studies found that positive functioning after acute adversity (or adversarial growth) was large in magnitude and could persist for a year or longer after the traumatic events [50-52]. Our findings are consistent with this viewpoint. As illustrated in Figure 1, the decreasing pattern in depression continued 10 months after the national lockdown, suggesting that the positive changes in emotion last for a long time.
For Chinese university students, this may partly be because the lockdown itself could have offered a reprieve from daily academic hassles and stress. School-related problems are a major stressor that contributes to students’ mental health problems across the globe [53]. Exams, housing, friendships, relationships, financial pressures, and career uncertainty - these are all reasons that result in stress. Compared with Western universities, students endure much more a sense of competition because academic performance will sort them to eventually decide their future career [54]. School closure and lockdown may benefit to escape these negative stressors, as vacations and weekends usually are stress reduction due to periods of relaxation [55]. In addition, students staying at home may have more time doing enjoyable things that typically students would not be able to, such as longer use times with playing games and watching funny videos, more flexible time to learning and rest, more independent space to expand autonomy [21], resulting in increased positive emotion and then better sense of well-being. Indeed, when universities reopened, they it had been 8 months for school close since the pandemic started. It is, therefore, very likely that the relaxed and prolonged home duration could lead to positive psychological change, as increased resilience, reduced depression and decreased perceived stress presented 10 months after lockdown in our study.
These changes in depressive symptoms were associated with preexisting mental health problems, which two groups displayed a less decrease in depression from pre- to post-lockdown, namely, individuals with high level of psychotic symptoms and those with self-harm. These results are consistent with previous studies showing pre-existing health inequalities were strongly linked with mental health difficulties during and after lockdown [56]. Indeed, these vulnerable groups were associated with less depression improvement in present study across time. It will be helpful in identifying priorities of mental health needs among various vulnerable populations for improving national mental health.
It is interesting that these improvement patterns during pandemic often explained a few sentences in the discussion or ignored entirely. This is because that a traditional perspective has focused on clinical symptomatology by addressing the ways in which people are wounded and weakened during crisis. However, most people manage to live lives of ‘dignity and purpose’ despite difficulties and challenges [57]. Meta-analysis research found that more than 50% of people who endured trauma come out stronger from the experience [58]. The present findings strongly suggested that the pandemic may stimulate improvement in our psychological adjustment and lead to mental growth from adversity, which encourage future research to focus more on benefit finding and personal growth in times of crisis.
It should be taken into consideration that the small sample size prevented adequately powered statistical analysis, such as those with pre-existing mental health disorders could be particularly vulnerable to the negative effects of this pandemic, but less participants who had history of diagnosed mental illness (N=2), or suicidal plan (N=2), suicidal attempt (N=1) in the present study stopped from further analysis. However, in our larger sample (in preparation), preliminary results found a short- and long-term improvement in depression and anxiety in Chinese adolescent sample (n=1577) who had completed a 4-year, six-wave longitudinal study. Similarly, the improvement pattern in depression, anxiety and pleasure capacity were also found in another longitudinal study (n=2000) that carried out in the same university with the present study. These results supported that the Chinese lockdown had a positive effect on students’ mental health. In addition, online data collection could lead to particular loss of participants with poor or declining mental health, resulting in biases towards better mental health. Further prospective studies are needed, including larger and diversity sample and a wider range of potential risk factors.
In conclusion, the present findings suggested that the impact of lockdown on mental wellbeing was beneficial in the short and long-term in Chinese university students. Individuals with high level of psychotic symptoms and those with self-harm had less improvement in depression than those with without these conditions.
XHY devised the study concept, interpreted the data and wrote up the first draft. SXL, LLC and CLW collected data. MQL administrated the investigation. All authors contributed to editing and commenting on the final version.
The authors declare that this study received funding from the MSc-PHD Talent project of Changning Health Commission (RCJD2022S08) and the East China Normal University and health joint fund (2022JKXYD09003) to XHY, the Clinical Project of Changning Health Commission (20194Y013) and Shanghai Health Commission (20204Y0499) to LLC. The funders were not involved in the study design, collection, analysis, and interpretation of data, the writing of this article or the decision to submit it for publication.
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the Hunan Agricultural University (2020-026).
Informed consent was obtained from all subjects involved in the study.
The data is available from the corresponding author upon request.
The authors declare no conflict of interest.
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Sholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Sholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [PubMed].
[Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed]..
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Sholar].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
[Crossref] [Google Sholar] [PubMed].
[Crossref] [Google Sholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
Citation: Yang X.H, Liu S.X, Chen L.L, Wang C.X, Long M.Q (2022) Changes in Depression Pre-, During and Post-Lockdown in a Chinese Student Sample. J Dep Anxiety.11:487
Received: 12-Sep-2022, Manuscript No. JDA-22-20096; Editor assigned: 15-Sep-2022, Pre QC No. JDA-22-20096 (PQ); Reviewed: 29-Sep-2022, QC No. JDA-22-20096; Revised: 06-Oct-2022, Manuscript No. JDA-22-20096 (R); Published: 13-Oct-2022 , DOI: 10.35248/2167-1044.22.11.487
Copyright: © 2022 Yang X.H, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.