Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 6
Objective: To evaluate and compare the changes of Higher Order Aberration (HOAs), visual acuity and refractive outcome after using wavefront guided Lasik and topography guided Lasik for correction of refractive errors.
Materials and methods: This is a prospective comparative study recruited 60 eyes of 30 patients, where 15 patients underwent topo-guided Lasik and 15 patients underwent wavefront guided Lasik. All participants underwent Uncorrected Visual Acuity (UCVA), Best Corrected Visual Acuity (BCVA), refractive outcome and wavefront to assess Root Mean Square (RMS) and Higher Order Aberration (HOAs) in each group and compare between Wavefront Guided Lasik (WFG) and Topography Guided Lasik (TG) pre-operative and at 3 months and 6 months post-operative.
Results: Mean patient age was 29.33 ± 5.62, 28.73 ± 6.72 in topoguided and wavefront group respectively. In TG group, statistically significant improvement were evident postoperatively in Spherical Equivalent (SE) (P=0.000), spherical aberration (P=0.00) and UCVA (P=0.000). Similarly in WFG group, statistically significant improvement were evident postoperatively in spherical equivalent (P=0.000), spherical aberration (P=0.04) and UCVA (P=0.000). On comparing HOAs, topoguided was significantly better at 3 months (P=0.02), but at the end of the study there was no statistically significance difference (P=0.052), spherical aberration (P=0.047) was significantly lower in WFG and coma (P=0.032) were significantly lower in TG group.
Conclusion: The study showed good efficacy, predictability, and stability of eyes undergoing TG Lasik and WFG Lasik with a follow-up of six months.
High order aberration; Visual acuity; Refraction; Wavefront guided lasik; Topoguided lasik
Higher Order Aberrations (HOAs), (spherical aberrations, coma, and trefoil) are small optical irregularities of the ocular refractive media. Those HOAs cannot be improved with spectacles or contact lenses, dissimilar to low order aberrations (myopia, hypermetropia, and simple astigmatism) [1]. After effective improvement of error of refraction by refractive surgery, patients start complaining of halos, glare and reduction in contrast sensitivity. Authors have determined that HOAs are responsible for these postoperative complains and symptoms [2].
Wavefront Guided (WFG) ablations have been known to be successful and expectable in improving astigmatism and HOAs in the eye. Evaluating its effects for treatment of HOAs is important [3]. The WF-guided approach provides a customized treatment plan relied on an eye’s special preoperative aberrometry intending to not only diminishing induced postoperative aberrations but also decreasing or eliminating preoperative HOAs [4].
Topography Guided (TG) excimer ablation relies on high-resolution corneal topographic height maps to render a customized ablation profile comprising HOAs and perfect measurement of the corneal astigmatism. Topography-guided custom ablation treatment has been accepted by the U.S. Food and Drug Administration (FDA) for primary Lasik in myopic and myopic astigmatism eyes, with good results, efficiency and safety [5].
Prospective comparative study comprised 60 eyes of 30 patients divided into group A including 15 patients underwent topo- guided Lasik and group B including 15 patients underwent wave- front guided Lasik. Patients were recruited between July 2017 to July 2020 at Fayoum University Hospital and Dar El Oyoun Hospital.
Inclusion and exclusion criteria
Inclusion criteria included patients with age group from 21 to 39, Error cylinder from +4 to -4 astigmatism and sphere from +5 to -8, topographic K reading from 40 to 46, while exclusive criteria included patients with a corneal thickness of less than 500 μm.
Preoperative examination included the following
Autorefraction with and without cycloplegia, visual acuity measurement (Uncorrected Visual Acuity (UCVA) and Best Corrected Visual Acuity (BCVA) using logMAR).
Investigation
Corneal tomography was performed by using Scheimpflug camera (Oculus Pentacam®; Oculus Optikgerate GmbH, Wetzlar, Germany).
Wavefront analysis: Using the iDesign wavefront (Abbott Medical Optics Inc. STAR S4 IR, IDesign), four readings were taken before surgery and after surgery at 3 and 6 months and the best achievement, simplified by purest centroid image, was used for analysis, to measure Root Mean Square (RMS). Group A (TG Lasik): the treatment plan were obtained using the Allegro Topolyzer topography vario (Alcon, Ft Worth, TX, and USA) system. Topography images were picked out for acceptable covering, uniformity among 2 to 8 images, and accurate mire recognition and then were transported to the laser study notebook computer. Manifest refraction data were entered into the study notebook computer along with an asphericity correction. Next, the laser treatment pattern was calculated by the study notebook software using refractive data for the correction of lower-order errors and corneal topographic data for the correction of higher- order errors. Group B (WFG Lasik): WFG lasik of IDESIGN (Abbott Medical Optics Inc.). Preoperative aberrometry was measured with the iDesign System, and the calculated was used to alter the sphere according to the magnitude of the aberrometer- derived cylinder to avoid overcorrection of sphere. After the flaps were elevated, the programmed treatment was applied once iris registration was achieved.
Surgical technique
Patients were scheduled for topography-guided and wavefront guided Lasik procedure. Group A, the Lasik platform used was The WaveLight EX500 excimer laser with T-CAT software (Alcon, Ft Worth, TX, USA) for excimer ablation. In order to remove the minimum possible tissue, the optical zone diameter was kept between 5.5 mm and 6.5 mm in all cases. Group B (Visx S4 iDesign) (Abbott Medical Optics Inc), the laser ablation was calculated according to the new- generation Hartmann-Shack aberrometer measurement that was applied using the Star S4IR excimer laser. Treatments were programmed in group A cases with a 6.0 mm optical zone and a total ablation zone between 8.0 mm and 9.0 mm.
Then, patients received topical steroid antibiotic drops tobramycin and dexamethasone (Tobradex®; Alcon Laboratories, Inc.) four times daily for 1 week and then tapered off for the next 3 weeks and (systane Alcon Laboratories, Inc) for dry eyes for 3 months.
Postoperative evaluation includes slit lamp examination, UCVA on 1 day, 1 week, 3 months and 6 months and wavefront to assess HOAs in each group and compare between wavefront guided Lasik and topography guided Lasik at 3 months and 6 months.
Statistical analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations and ranges when parametric and median, Inter-Quartile Range (IQR) when data found non-parametric. Also qualitative variables were presented as number and percentages.
The comparison between groups with qualitative data was done by using Chi-square test. The comparison between two groups with quantitative data and parametric distribution were done by using Independent t-test; while the comparison between two groups with quantitative data and non- parametric distribution was done by using Mann-Whitney test. Also, the comparison between more than two paired groups with quantitative data and non-parametric distribution were done by using Friedman test followed by post hoc analysis using Bonferoni test.
The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant as P>0.05 is non-significant and if P<0.05 is significant.
Demographic data
This study included 60 eyes of 30 patients where 15 patients underwent topoguided Lasik and 15 patients underwent wavefront guided Lasik, there was no statistically significances difference regarding age, sex, K reading and corneal thickness with P values: P=0.793, P=0.439, P=1.00 and P=0.0666 respectively (Table 1).
| Demographic data | Topoguided group | Wavefront group | P-value | |
|---|---|---|---|---|
| No=15 | No=15 | |||
| Age | Mean ± SD | 29.33 ± 5.62 | 28.73 ± 6.72 | 0.793 |
| Sex | Female | 9(60.0%) | 11(73.3%) | 0.439 |
| Male | 6(40.0%) | 4(26.7%) | ||
| k1 | Mean ± SD | 42.75 ± 1.32 | 42.75 ± 1.32 | 1.000 |
| k2 | Mean ± SD | 43.93 ± 1.44 | 43.93 ± 1.44 | 1.000 |
| Pachymetry | Mean ± SD | 536.50 ± 13.35 | 544.03 ± 17.48 | 0.066 |
Note: P-value >0.05: Non significant; P-value <0.05: Significant; SD: Standard Deviation
Table 1: Independent t-test. Demographic data of the patients underwent topoguided lasik and wavefront guided lasik.
Visual acuity
Regarding the visual acuity, there was significant improvement in UCVA from day one postoperatively, with mean at pre-operative was 0.52 ± 0.19 (TG), 0.57 ± 0.23 (WFG) and at 3 months was 0.03 ± 0.06, 0.05 ± 0.06 of topoguided group and wavefront group with P value (P=0.000) and (P=0.000) respectively, with no significant difference in mean changes from 3 months to 6 months (P=0.0317) and (P=0.157) respectively. For BCVA, there was no significant difference between pre-operative and post-operative (P=0.368) in topoguided group, but there was significant difference between pre-operative and post-operative (P=0.05) in wavefront group (Table 2).
| Visual acuity | Pre-operative | 3 months | 6 months | P-value | |
|---|---|---|---|---|---|
| No=15 | No=15 | No=15 | |||
| Topoguided group | |||||
| UCVA | Mean ± SD | 0.52 ± 0.19 | 0.03 ± 0.06 | 0.03 ± 0.06 | 0 |
| BCVA | Mean ± SD | 0.03 ± 0.07 | 0.03 ± 0.06 | 0.03 ± 0.06 | 0.368 |
| Parameters | P1 | P2 | |||
| UCVA | 0 | 0 | |||
| Wavefront group | |||||
| UCVA | Mean ± SD | 0.57 ± 0.23 | 0.05 ± 0.06 | 0.05 ± 0.06 | 0 |
| BCVA | Mean ± SD | 0.05 ± 0.07 | 0.05 ± 0.06 | 0.04 ± 0.06 | 0.05 |
| Parameters | P1 | P2 | |||
| UCVA | 0 | 0 | |||
| BCVA | 0.157 | 0.046 | |||
Note: P-value>0.05: Non significant; P-value<0.05: Significant; UCVA: Uncorrected Visual Acuity; BCVA: Best Corrected Visual Acuity; SD: Standard Deviation; P1: Comparison between pre-operative vs. 3 months; P2: Comparison between pre-operative vs. 6 months; P3: Comparison of 3 months vs. 6 months
Table 2: Friedman test followed by post hoc analysis using Wilcoxon rank test. UCVA and BCVA pre-operative and post-operative results in both groups.
On comparing two procedures, there was no statistically significant difference between topography and wavefront guided lasik post-operative. Both procedures were equally efficacious at the end of the 6-month follow-up. No eye lost lines of BCVA at 6 months after surgery and 2 eyes from topography guided group (6%) and 5 eyes from wavefront guided group (16.6%) gained lines, twenty two eyes (73.3%) of the wavefront guided lasik and twenty eyes (66.6%) of the topography guided lasik had a UCVA of 0.00 log MAR (P=0.332) at the end of 6 months.
Refractive outcome
Preoperative and postoperative refractive outcomes in TG group (spherical equivalent, sphere and cylindrical), there was significant reduction on day one post-operative. The mean spherical equivalent, sphere and cylindrical pre-operative were -2.50 ± 2.62, -1.88 ± 2.54 and -2.53 ± 1.31 and at 3 months were -0.38 ± 0.44, -0.19 ± 0.45 and 0.42 ± -0.30 with P value (P<0.001, P=0.015 and P=0.00) respectively. There was no significance difference during the rest of follow up except for SE, there was sadistically significant difference from 3 to 6 months (P=0.013) (Table 3).
| Topoguided group | Pre-operative | 3 months | 6 months | P-value | |||
|---|---|---|---|---|---|---|---|
| No=15 | No=15 | No=15 | |||||
| SE | Mean ± SD | -2.50 ± 2.62 | -0.38 ± 0.44 | -0.30 ± 0.37 | 0.000 | ||
| Sphere | Mean ± SD | -1.88 ± 2.54 | -0.19 ± 0.45 | -0.20 ± 0.41 | 0.000 | ||
| Cylinder | Mean ± SD | -2.53 ± 1.31 | -0.42 ± 0.30 | -0.35 ± 0.34 | 0.000 | ||
| Parameters | P1 | P2 | |||||
| SE | <0.001 | <0.001 | |||||
| Sphere | 0.015 | 0.024 | |||||
| Cylinder | 0.000 | 0.000 | |||||
Note: P-value>0.05: Non significant; P-value<0.05: Significant; SE: Spherical Equivalent; SD: Standard Deviation; P1: Comparison between pre-operative vs. 3 months; P2: Comparison between pre-operative vs. 6 months; P3: Comparison of 3 months vs. 6 months
Table 3: Friedman test followed by post hoc analysis using Wilcoxon Rank test. Preoperative and postoperative refractive outcome in topoguided group.
Regarding wavefront guided group, there was also significant reduction observed from day one post-operative with mean pre- operative spherical equivalent, sphere and cylindrical refractive outcome were -2.04 ± 3.22, -1.32 ± 3.33 and -1.67 ± 0.92 and at 3 months were -0.47 ± 0.38, -0.34 ± 0.46 and -0.45 ± 0.30 respectively, that was statistically significant with P value at 3 months (P=0.026, P=0.035 and P=0.000) respectively. No significant changes were observed in these parameters (spherical equivalent, sphere and cylindrical refractive outcome) during the rest of the follow-up with P value (P=0.152, P=0.208 and P=0.248) respectively at 6 months (Table 4).
| Wavefront group | Pre-operative | 3 months | 6 months | P-value | |
|---|---|---|---|---|---|
| No=15 | No=15 | No=15 | |||
| SE | Mean ± SD | -2.04 ± 3.22 | -0.47 ± 0.38 | -0.42 ± 0.30 | 0.001 |
| Sphere | Mean ± SD | -1.32 ± 3.33 | -0.34 ± 0.46 | -0.22 ± 0.33 | 0.001 |
| Cylinder | Mean ± SD | -1.67 ± 0.92 | -0.45 ± 0.18 | -0.42 ± 0.17 | 0.000 |
| Parameters | P1 | P2 | |||
| SE | 0.026 | 0.015 | |||
| Sphere | 0.035 | 0.050 | |||
| Cylinder | 0.000 | 0.000 | |||
Note: P-value>0.05: Non significant; P-value<0.05: Significant; SE: Spherical Equivalent; SD: Standard Deviation; P1: Comparison between pre-operative vs. 3 months; P2: Comparison between pre-operative vs. 6 months; P3: Comparison of 3 months vs. 6 months
Table 4: Friedman test followed by post hoc analysis using wilcoxon Rank test, Preoperative and postoperative refractive outcome in wavefront group.
On comparing two groups, there was statistically significant difference regarding pre-operative cylindrical refraction with P value (P=0.001), non-significant difference in SE and spherical refraction pre-operative with P value (P=0.419 and P=0.536, respectively) and also on post- operative SE, sphere and cylinder with the P value (P=0.313), (P=0.309) and (P=735) at 3 months and (P=0.57), (P=1.00) and (P=0.825) at 6 months, respectively.
Aberrometric data
The aberrometric data in topoguided group, the mean change of RMS pre-operative, 3 months and 6 months postoperative were 0.52 ± 0.44, 0.39 ± 0.16 and 0.37 ± 0.15, respectively. The results showed that there was significantly reduction of RMS at 3 months post-operative with P value (P=0.030) and with no significance difference from 3 months to 6 months with P value (P=0.235). Regarding coma and spherical aberration, no significant changes were observed in coma (P=0.074) and significant improvement was observed in spherical aberration (P=0.000) (Table 5).
| Topoguided group | Pre-operative | 3 months | 6 months | p-value | |
|---|---|---|---|---|---|
| N=15 | N=15 | N=15 | |||
| RMS | Mean ± SD | 0.52 ± 0.44 | 0.39 ± 0.16 | 0.37 ± 0.15 | 0.040 |
| Coma | Mean ± SD | 0.09 ± 0.09 | 0.07 ± 0.03 | 0.06 ± 0.03 | 0.074 |
| Spherical aberration | Mean ± SD | 0.06 ± 0.11 | 0.03 ± 0.06 | 0.02 ± 0.06 | 0.000 |
| Parameters | P1 | P2 | |||
| RMS | 0.030 | 0.013 | |||
| Spherical aberration | 0.001 | 0.000 | |||
Note: P-value>0.05: Non significant; P-value<0.05: Significant; RMS: Root Mean Square; SD: Standard Deviation; P1: Comparison between pre-operative vs. 3 months; P2: Comparison between pre-operative vs. 6 months; P3: Comparison of 3 months vs. 6 months
Table 5: Friedman test followed by post hoc analysis using Wilcoxon Rank test. Preoperative and postoperative aberrometric data in topoguided group.
In wavefront guided group, the mean changes of RMS pre- operative, 3 months and 6 moths post- operative were 0.53 ± 0.50, 0.63 ± 0.35 and 0.51 ± 0.29 respectively. The results showed that there was increase in RMS at 3 months in comparison to pre-operative, however, not statistically significant with P value (P=0.253). At 6 months, there was significant reduction in RMS in comparison to 3 months with P value (P=0.002). But at the end of the study there was no significance difference in RMS pre- operative to 6 months with P value (P=0.975). Regarding coma and spherical aberration there was no significance difference in coma (P=0.051) and significant improvement in spherical aberration (P=0.004) was observed (Table 6).
| Wavefront group | Pre-operative | 3 months | 6 months | p-value | |
|---|---|---|---|---|---|
| N=15 | N=15 | N=15 | |||
| RMS | Mean ± SD | 0.53 ± 0.50 | 0.63 ± 0.35 | 0.51 ± 0.29 | 0.006 |
| Coma | Mean ± SD | 0.07 ± 0.03 | 0.11 ± 0.10 | 0.11 ± 0.10 | 0.051 |
| Spherical aberration | Mean ± SD | 0.02 ± 0.02 | -0.01 ± 0.07 | -0.01 ± 0.06 | 0.004 |
| Post hoc analysis | |||||
| Parameters | P1 | P2 | P3 | ||
| RMS | 0.253 | 0.975 | 0.002 | ||
| Spherical aberration | 0.003 | 0.002 | 0.797 | ||
Note: P-value>0.05: Non significant; P-value<0.05: Significant; RMS: Root Mean Square; SD: Standard Deviation; P1: Comparison between pre-operative vs. 3 months; P2: Comparison between pre-operative vs. 6 months; P3: Comparison of 3 months vs. 6 months.
Table 6: Friedman test followed by post hoc analysis using Wilcoxon Rank test. Preoperative and postoperative aberrometric data in topoguided group.
On comparing topoguided Lasik and wavefront guided Lasik RMS, there was no significant difference between two procedures at the end of 6 months (P=0.055). But at 3 months the results revealed that the topography guided achieved statistically significantly (P=0.02) greater predictability, reduced HOAs, especially in patients with preoperative HOAs greater than 0.3 RMS. Regarding coma and spherical aberration, coma was significantly better at 6 months (P=0.032) in topoguided group and spherical aberration was significantly better in wave front group at 3 months (P=0.047) (Table 7 and Figures 1a-1c).
| Characteristics | Topoguided group | Wavefront group | P-value | |
|---|---|---|---|---|
| No=15 | No=15 | |||
| Root mean square | ||||
| Pre-operative | Mean ± SD | 0.52 ± 0.44 | 0.53 ± 0.50 | 0.584 |
| Post-operative 3 months | Mean ± SD | 0.39 ± 0.16 | 0.63 ± 0.35 | 0.002 |
| Post-operative 6 months | Mean ± SD | 0.37 ± 0.15 | 0.51 ± 0.29 | 0.055 |
| Coma | ||||
| Pre-operative | Mean ± SD | 0.09 ± 0.09 | 0.07 ± 0.03 | 0.202 |
| 3 months | Mean ± SD | 0.07 ± 0.03 | 0.11 ± 0.10 | 0.156 |
| 6 months | Mean ± SD | 0.06 ± 0.03 | 0.11 ± 0.10 | 0.032 |
| Spherical aberration | ||||
| Pre-operative | Mean ± SD | 0.06 ± 0.11 | 0.02 ± 0.02 | 0.072 |
| 3 months | Mean ± SD | 0.03 ± 0.06 | -0.01 ± 0.07 | 0.047 |
| 6 months | Mean ± SD | 0.02 ± 0.06 | -0.01 ± 0.06 | 0.278 |
Note: P-value>0.05: Non significant; P-value<0.05: Significant; SD: Standard Deviation; RMS: Root Mean Square
Table 7: Mann-Whiney test. Comparison between topoguided lasik and wavefront guided lasik regarding RMS, coma and spherical aberration.
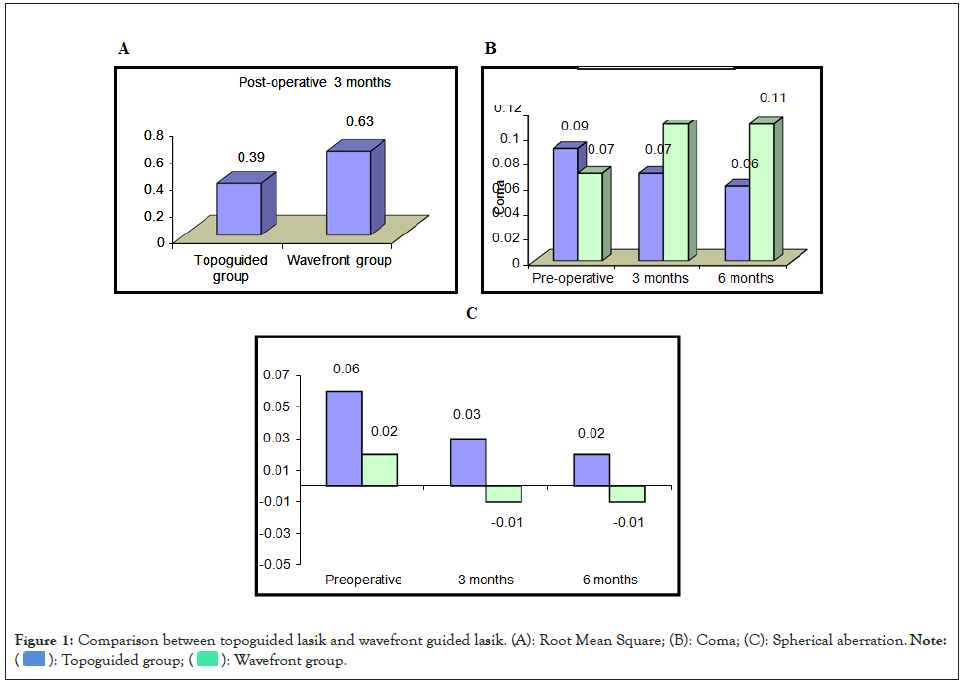
Figure 1: Comparison between topoguided lasik and wavefront guided lasik. (A): Root Mean Square; (B): Coma; (C): Spherical aberration.

Wavefront-guided treatments try improving refractive outcomes by taking in consideration HOAs of the optical system, like the aberrations from the cornea, the lens, and even the retina; topography-guided ablation intent to make the uneven front corneal surface regular to accomplish the wanted refractive outcome [6].
The pupil limits the wavefront measurements and therefore, measurements of the periphery are not concerned. Secondly, eyes go through pupil centroid shift producing visual quality deterioration. Topographic calculations are not relying on the size or the shape of the pupil and they deal with cornea centrally and periphery. This is an important advantage of TG Lasik as irregularities in the periphery of the corneas are accountable for the majority of HOAs. The use of TG Lasik in eyes with optical zones small or off-center has been exposed by previous studies [7].
Topographers do not give data about the sphero-cylindrical refraction of the eye, unalike wavefront analyzers. Therefore, topographic refractive treatment algorithms should be incorporated with measurements taken from manifest refraction more than based on information given by the topographer alone [8].
The aim of this study is to evaluate and compare the changes of HOA, UCVA and refraction after using wavefront guided Lasik and topography guided Lasik for correction of refractive errors. This study included 60 eyes of 30 patients treated with topoguided lasik and wavefront guided lasik (15 patients each group) July 2017 to October 2019 at Dar El Oyoun hospital.
Regarding topoguided group, this study evaluated the performance in terms of visual, refractive, and aberrometric outcomes. The efficacy of the surgery was good in the sample evaluated, with logMAR 0.00 UCVA achieved in almost all cases, and significant improvement in refractive outcome. Similarly to Hashmani et al. evaluating the outcomes of TG Lasik, BCVA preoperative was 20/20. On day one and 6 months post-operatively, 86% and 94% of eyes had a UCVA of 20/20 or better, respectively. The mean preoperative sphere, cylinder, and Spherical Equivalent (SE) values were -4.3 ± 1.6 (D), -1.0 ± 0.8 D, and -4.8 ± 1.8 D, and on 6 months positively they were -0.1 ± 0.6, -0.5 ± 0.3, and -0.4 ± 0.6 D, respectively [7].
Also similar to Kanellopoulos who found good predictability and safety on using TG Lasik. His study comprised 202 eyes with hyperopic astigmatism and hyperopia that had underwent TGL. His study revealed that 75.5% and 94.4% of eyes accomplished 0.5 D and 1D of target SE at 24 months, whereas there was gained in one line at least in 46.6% of eyes postoperatively [9].
Regarding aberrometric data, this study revealed that there was significant improvement in RMS HOAs and spherical aberration with no significance difference in coma post-operatively in TG Lasik group that was similar to a contralateral study conducted by Farooqui and Al-Muammar, in which they found the same safety and predictability of TG Lasik in improving HOA that comprises 46 eyes that experienced topography-guided corneal customized Lasik using the Customized Aspheric Treatment zone (CATz) ablation profile in one eye and conventional Lasik using in the other eye for myopia with or without astigmatism. Postoperative glare and RMS values for HOAs were assessed at 1 and 3 months and compared between the two eyes. 81% of patient’s specified glare was greater in conventionally treated eyes than in the CATz- treated eyes at 1 and 3 months postoperatively. The RMS values for total coma (0.2385 vs. 0.1522) and spherical aberration (0.2381 vs. 0.1058) in conventionally treated and CATz-treated eyes were significantly greater in conventionally treated eyes (P=0.029 and P=0.004, respectively) at 3-month follow-up [10].
This is contrary to a study done by Wallerstein et al. RMS was raised to the pre-operative value. But the patients had remarkable improvements in both subjective uncorrected quality of vision and disturbance of night vision after Lasik in comparison to spectacle- and contact lens-corrected vision and spectacle before Lasik. TG ablation using the Alcon WaveLight EX500 excimer laser and T-CAT/Contoura software resulted in outstanding precision, effectiveness, and safety, with better quality of vision and improved disturbance of night vision post-operative in eyes with astigmatic refraction 2.00 D or greater, plus eyes with topographic irregular astigmatism [11].
Regarding wavefront group, this study revealed that the efficiency of the surgery was good in the sample evaluated, with logMAR 0.00 UCVA achieved in almost all cases, and significant improvement in refractive outcome similar to a study done by Smadja et al. In which there was improvement in UCVA from 0.1 ± 0.1 preoperatively to 1.1 ± 0.15 postoperatively (P<0.01), 76.6%, 94.4%, and 96.6% of the eyes had monocular vision BCVA of 20/16, 20/20, and 20/25 respectively. No eye lost 2 or more lines of BCVA, and 29.2% of the eyes gained 1 or more lines of BCVA. Manifest SE postoperatively was within ± 0.5 diopter in all eyes [12].
Another retrospective study published by Schallhorn et al. who evaluated WFG Lasik, using wavefront data achieved with a new Hartmann-Shack aberrometer (iDesign Advanced WaveScan aberrometer; Abbott Medical Optics, Inc., there was significant improvements in both UCVA (P<0.01) and BCVA, (P<0.04) were detected postoperatively. No eyes lost two or more lines of BCVA. In 14.0% (34 eyes), there was improvement of one or more lines of BCVA of the overall sample. For refractive outcomes, the manifest SE was changed from -3.28 ± 1.79 diopters (D) before surgery to -0.03 ± 0.29 D one month after surgery. Their study revealed that 93.0% of the eye accomplished within 0.5 D and 99.6% within 1 D of target manifest SE. Preoperative manifest astigmatism was -0.72 ± 0.67 and reduced to -0.14 ± 0.20 at 1 month [13].
Regarding RMS of wavefront guided group HOAs increased at 3 months positively, but not statistically significant, then decreased significantly at 6 months. There were also no significance changes from pre-operative to 6 months with any significance changes in coma, significant reduction in spherical aberration.
Similarly to Duran et al. made a study on 33 eyes having WFG Lasik with the Star S4IR excimer laser combined with the iDesign system. No significant changes were noticed in coma and spherical aberration (P=0.778, P=0.677) at 30 days postoperatively. The RMS increased significantly at 30 days postoperatively (P=0.041), but decreased significantly at 90 days postoperatively (P=0.007), reaching the preoperative levels (P=0.233), which settled the capability of the WFG Lasik to afford good control of ocular HOAs [14].
Other studies have shown a significant aberrometric reduction, such as Moussa et al. who found a significant decreased in the level of primary spherical aberration, RMS after WFG Lasik using the same laser platform and aberrometer [15]. Other study by Wang and Koch, they found the RMS value corresponding to HOAs experienced a statistically significant increase but of very small amount (0.02 μm) and was not clinically significant considering the variability of this parameter in the normal healthy population. Dissimilarities between studies in the level of myopia and astigmatism treated as well as in the surgical procedure followed could account for the differences in this matter [16].
On comparing RMS value, the results of the present study revealed that there were no statistically significance difference between both group at 6 months with (P=0.055), and both platform were safe, effective and predicable regarding HOA. This was similar to a study made by Toda et al. Patients were randomly assigned to WG ablation or TG guided ablation. HOA were assessed between groups before, 1 and 3 months after Lasik. The results revealed that the HOAs evaluated by iDesign were not significantly different between the two groups at 1 and 3 months after Lasik. Both customized ablation systems used in Lasik accomplished outstanding results in quality of vision and visual function [17]. Another study made by Kanjani et al. showed similar results that WG and TG Lasik lead to increase visual performance by reducing HOAs [18].
On the other hand, our study revealed that at 3 month the topography guided achieved statistically significant difference (P=0.02) that was similar to Moshirfar et al. who found that when assessing RMS of HOA, the amount was quite small for Alcon Contoura since it assessed only the aberration of the cornea, whereas Visx iDesign assessed HOA of the whole optical system, and that Visx IDesign produced less HOAs than Nidek CATz. Though, this evaluation was unfair since Nidek CATz had nearly a greater preoperative HOA than Visx iDesign. Treating patients with a greater baseline HOA may have also exaggerated some of the other results, and thus control for this variable is required for future studies [19].
So this study demonstrated good efficacy, predictability, and stability of eyes undergoing TG Lasik and WFG with a follow-up of six months. Both procedures were equal in efficacy and safety at 3 and 6 months regarding vision and refraction, but for RMS and high order aberration, topoguided was better at 3 months but at the end of the study there was no difference. Future studies are needed to confirm whether the same levels of predictability, safety and postoperative visual quality outcome in larger number of patients with longer follow up period.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Amin MH, Kamal MA, Sherif AM, Hafez MAA, Abdallah KK (2022) Changes of Higher Order Aberrations after using Wave Front Guided Lasik and Topography Guided Lasik for Correction of Refractive Errors: A Comparative Study. J Clin Exp Ophthalmol. 13:931.
Received: 04-Nov-2022, Manuscript No. JCEO-22-18974; Editor assigned: 07-Nov-2022, Pre QC No. JCEO-22-18974 (PQ); Reviewed: 21-Nov-2022, QC No. JCEO-22-18974; Revised: 28-Nov-2022, Manuscript No. JCEO-22-18974 (R); Published: 05-Dec-2022 , DOI: 10.35248/2155-9570.22.13.931
Copyright: © 2022 Amin MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.