Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research - (2020)Volume 10, Issue 10
Background: Pregnancy is a dynamic physiological state evidenced by several transient changes which even affects the oral cavity. Present study was conducted with an aim to assess the changing patterns of gingivitis and periodontitis in different trimesters of pregnancy amongst pregnant and non-pregnant women attending the outpatient Department of Government Hospitals in Delhi, India.
Methodology: A total sample size of 800 pregnant and 800 non-pregnant women attending the O.P.D of 4 Government hospitals of Delhi was obtained through Stratified Cluster Sampling Technique. A structured pretested assessment form was used to assess the gingival, periodontal and oral hygiene status using Gingival Index (GI), Community Periodontal Index (CPI) and Loss of Attachment (LOA) and Oral Hygiene Index-Simplified (OHI-S). Statistical analysis was done using SPSS v16.0 software package.
Results: Mean GI scores was significantly high for pregnant women than non-pregnant women (1.57 ± 0.51, 1.48 ± 0.35 respectively, p<0.001) and was more in 2nd trimester (1.73 ± 0.42) and 3rd trimester (1.75 ± 0.45) as compared to 1st trimester of pregnancy (1.25 ± 0.48) (p=0.001). Maximum CPI code 3 was seen in 14.6% of pregnant subjects and 8.1% of non-pregnant subjects (p-0.001). Mean OHI-S score for pregnant and non-pregnant subjects was 2.89 ± 0 and 2.60 ± 1.07 respectively (p=0.002).
Oral Hygiene status also worsened with increase in trimester of pregnancy, (p=0.001).
Conclusion: Prevalence of the Gingival and Periodontal disease was significantly high among pregnant women and worsened with increasing gestation age Hence it is necessary to reinforce knowledge about significance of oral health in pregnant women by means of appropriate preventive and educational programs.
Trimester wise comparison; Pregnancy, Gingival health; Periodontal health; India
Oral health is an important component of general health. Many risk factors of oral disease are often the same as those implicated in the major general diseases. It affects people both physically and psychologically and there exists a relationship between oral diseases and systemic health. Oral health also constitutes an integral part of overall health and wellbeing for women across the lifespan [1,2].
Mother’s health influences the healthy future of society which depends on the health of the children of today and their mothers, who are guardians of that future. Pregnancy is a dynamic physiological state evidenced by several transient changes. These changes can develop into various physical signs and symptoms that can affect the patient’s health, perceptions, and interactions with others in her environment [3-5].
The oral cavity is also the seat of these physiologic changes that mainly occur due to hormonal fluctuations during pregnancy like increase in progesterone level and altered metabolism and immune response; all increasing the woman’s susceptibility to oral infections, and occurrence of oral diseases like gingivitis, periodontitis, dental caries, tooth erosions, pyogenic granuloma, temporomandibular joint disorders etc. Even debilitated oral health influences pregnancy in the form of preterm delivery and low birth weight. Hence, there is a need to address various oral health conditions while managing the pregnant woman [6-20].
Even, different trimesters of pregnancy experience varied levels of hormonal fluctuations which provide peculiar clinical picture during that trimester. Gingivitis and periodontitis tends to appear in second month of pregnancy along with the increase in the proportion of anaerobic gram negative bacteria coinciding with an increase in oestrogen and progesterone levels. Maximum intensity is observed in eighth month after which it tends to revert back to normal.
Nayak R et al. [12] in Chattisgarh, India and Albornoz C et al. [13] in Spain; conducted studies to assess the influence of the gestation period (trimester) on the gingival health and found that gingival inflammation was worsened during the second and third trimesters of pregnancy which was contributed to the presence of Porphyromonas gingivalis.
The estimated crude birth rate of India (2016) has been reported to be 21 per 1000 mid-year population. Many Government health care programmes like Janani Suraksha Yojana (scheme) and The Integrated Child Development Services (ICDS) are currently under enforcement, which provide improved health care facilities to pregnant women. However, oral health care of pregnant women in India still majorly remains an unserved sector. Thus, it is important to know the status of oral health of pregnant women in order to recommend effective preventive measures [12-16].
Though there are voluminous literatures regarding the prevalence and severity of gingivitis and periodontitis in pregnant women in developed countries, scanty literature is available assessing the changing pattern of gingivitis and periodontitis in different trimesters of pregnancy in developing countries like India.
Hence, the present study was conducted with an aim to assess the changing patterns of gingivitis and periodontitis in different trimesters among pregnant women and comparing the same with non-pregnant women attending the Government Hospitals in Delhi. The data available will also be helpful in planning of oral health education and promotion programs for the pregnant women.
The present study was a hospital based cross-sectional study conducted in four Government Hospitals of Delhi, India. A total of 800 pregnant and 800 Non pregnant females were included for the study. The study period extended to 4 months from March 2014 to June 2014.
Prior to the main study, a pilot study was carried out in one of the selected Government hospital of Delhi. The sample size for the present study was calculated based on the data obtained from the pilot study conducted on fifty primigravidae women in one of the selected Government Hospital of Delhi, India. The prevalence of periodontal disease and gingivitis among pregnant women with single gestation was found to be 76.5% and 91% respectively. For the present study, the sample size was determined at 95% confidence interval. Sample size was calculated using the formula: n=z2 × p × q/ m2which was calculated to be 768 in pregnant females and thus, a minimum of 800 subjects were included in each group (pregnant and non pregnant females).
Sampling procedure
For the study purpose Delhi was arbitrarily divided into four zones namely North, South, East and West zones. There are twenty three Government hospitals under Delhi Administration in these zones with O.P.D facility in the Department of Obstetrics and Gynaecology. 17 Out of these; four hospitals were randomly selected through Stratified Cluster Sampling method such that one hospital from each zone was included for the study. From the selected hospitals, a total sample size of 800 pregnant females attending the outpatient department of Department of Obstetrics and Gynaecology, aged 20-30 years was obtained. The sample of 800 non pregnant females were mainly the relatives of the pregnant patients attending the O.P.D of Obstetrics and Gynecology Department of the selected hospitals matched with the pregnant females for age. Thus, from each selected hospital 100 pregnant and 100 non pregnant females were included for the study. The study subjects were selected on the basis of following inclusion and exclusion criteria [21-27].
Inclusion criterion
• Pregnant and non-pregnant women between 20 to 30 years
• Subjects who gave written informed consent
• Pregnant women who were prima gravidae
Exclusion criterion
• Subjects not willing to participate in the study
History of medications; current use of systemic corticosteroids, congenital heart disease, existing hypertension and diabetes before the pregnancy, history of epilepsy, asthma and chronic renal disease.
The study protocol was approved by the Institutional Ethical Committee, D.J. College of Dental Sciences and Research, Modinagar. Permission from the respective hospital and attending Gynaecologists for examining the subjects was obtained prior to the start of the study. The Permission to examine the pregnant females was obtained from the Medical Superintendent of each participating hospital. Written informed consent was obtained from each study participant. Structured proforma in English was used to record information on General information including sociodemographic characteristics, Duration of gestation in case of pregnant females, Past Medical and Dental History and Oral Hygiene Habits. A single examiner trained in the Dept. of Public Health Dentistry carried out all the clinical examinations. The intra examiner reliability was good (Kappa value 0.87). Type III clinical examination was done to record Gingival Index by Loe and Sillness for assessing gingival health, Oral Hygiene Index-simplified by Greene and Vermillion to evaluate debris and calculus deposits on the teeth and Community Periodontal Index and Loss of Attachment to assess the periodontal status.
All the collected data was entered in the Microsoft Word Excel Sheet 2007 version and processed using the SPSS v21.0 software package (SPSS Inc. Chicago, IL, U.S.A) Cohen’s kappa statistics was used to assess the examiner reliability. Student t-test, and One-way analysis of variance (ANOVA) was used to analyze the difference between the means of the two groups. The Chi square test was used to analyze difference between the proportions of the two groups. Any p-value less than 0.05 was considered significant.
The study group comprised of 800 Pregnant and 800 Non pregnant women in the age group of 20-30 years with mean age of 23.48 ± 2.87 and 25.66 ± 3.48 for Pregnant and Non Pregnant women respectively. Among the pregnant women; 149 (18.6%) were illiterate, 66 (8.3%) had done primary education, 204 (25.5%) had completed education till middle school, 179 (22.4%) had completed till high school, 93 (11.6%) completed education till Senior Secondary, 99 (12.4%) were Graduate and only 10 (1.2%) were Postgraduate. The educational status of non-pregnant subjects revealed that 51 (6.4%) were illiterate, 77 (9.6%) had done primary education, 273 (34.1%) had completed their studies until middle school, 228 (28.5%) had finished their high school, 42 (5.3%) had completed senior secondary120 (15%) were graduate while 9 (1.1%) were post graduate.
Trimester wise distribution of pregnant females is shown in Figure 1. The mean Gingival index scores was high for pregnant women (1.57 ± 51) than non-pregnant women (1.48 ± 35) and the difference was statistically significant (p<0.001). The periodontal health assessed through Maximum CPI and LOA score revealed that among pregnant women; Maximum CPI score 3 and 4 was seen in 117 (14.6%) and 3 (0.4%) respectively among pregnant women. However, among non pregnant women; only 65 (8.1%) women had Maximum CPI score 3 while score 4 was found in 1 (0.1%) women (p-0.001).
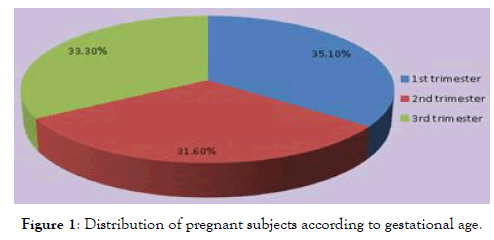
Figure 1: Distribution of pregnant subjects according to gestational age.
The mean OHI-S Score of pregnant women and non-pregnant women was 2.89 ± 0.95 and 2.60 ± 1.07. Respectively (p=0.002). The trimester wise comparison for the pregnant women revealed a statistically significant deteriorated gingival and periodontal health status with increasing gestational age. The same was observed for oral hygiene status as well.
Pregnancy is a unique yet a convoluted state in women’s life. The increase in hormonal secretion and growth of the fetus may pose various challenges in providing dental care for pregnant patients. Therefore, understanding physiologic changes of the body fetus on oral health of pregnant females is crucial. Only primigravidae subjects were included for the study so as to nullify the influence of previous pregnancy. The assessment of educational status among the pregnant and non-pregnant women elicited that 81.4% of the pregnant and 93.6% of non-pregnant women had completed a minimum of primary education. This is in accordance to the census report 2011 for Delhi NCT which reported a minimum literacy rate for females to be 80.93%. Past dental history unveiled that majority of the pregnant women had never visited a dentist before. Also, dental care services are available in very few states at the primary health care level thereby accounting for limited accessibility of dental treatment.
In our study, the prevalence of gingivitis was found to be 100% (subjects with mild, moderate and severe gingivitis among both pregnant women and non-pregnant women). This is similar to the findings of Loe and Silness in Norway [20]. However Nooch Poung Ret al. [6] in Thailand found the prevalence of gingivitis in pregnant women to be 86.4% and that in non-pregnant women to be 72.8% respectively. The increase in severity of gingivitis during pregnancy might be contributed to a rise in circulating levels of estrogen and progesterone which affect the gingival microvasculature Lundgren et al. [18] The elevated hormonal levels together with vascular changes give rise to a more florid response to the irritant effects of plaque and debris, resulting in gingivitis [6,10].
The mean Gingival Index scores gradually increased from first trimester to third trimester. Similar findings have been reported by Tilakaratne A et al. [19] in Sri Lanka and Nayak R et al. [12]. However non-significant increase in the Gingival index scores was seen in the findings of Bacima Get al. [20]. This coincides with an increase in estrogen and progesterone concentration. The maximum intensity is observed in the eight month, after which gingivitis decreases [10].
The prevalence of periodontal disease was high in the pregnant females as compared to non-pregnant females in the present study. The findings are in agreement with the findings of Jago JD et al. [21]. Also similar results have been reported by Tadkamadla A et al. [19] in Sri Lanka [8], Yaghobi S et al. in Iran [22] and Wandera M et al. [23] in Uganda. Only 2.9% of the pregnant subjects and 0.6% of non-pregnant subjects had periodontal loss of attachment measuring 4 mm-5 mm in the present study. Similar prevalence (8.1%) was reported in a study among normal pregnancy group. However, Vasiliauskiene I et al. [15] reported contrary findings of prevalence of 18.97% of pockets of 4 mm-5 mm. The periodontal status might be due to the effects of hormonal level on the gingival status of pregnant women which may be accompanied by increased levels of Bacteroides, Provtevella [8]. Also, worsening of the periodontal condition with the progression of pregnancy was observed. The findings are in agreement with studies conducted by Japan where the percentage of subjects with CPI score 3 and 4 increased from 7% in 2nd month of pregnancy to 31% in 8th month of pregnancy. Contradictory findings were reported by Tilakratne A et al. [19] in Srilanka where an increase in the gingival index score during the first to third trimester was observed but the values for the periodontal pockets did not any show significant difference during any stage of pregnancy. Our study also depicted deterioration in both periodontal status and periodontal loss of attachment with higher oral hygiene scores (p<0.05), suggesting that as a result of dental plaque accumulation, gingival changes develop superimposed on pregnancy associated physiologic alterations.
In our study, good oral hygiene was found in only 4.1% among pregnant women and 11.8% of non-pregnant women. Similar results have been reported by Amin R et al. [24] who reported mean OHI-S score of 1.031 ± 0.998 in pregnant and 0.592 ± 0.464 in non-pregnant women in Mangalore [27]. Higher scores in pregnant women might be due to elevated hormonal levels and changes in psychological behavior like stress and anxiety during pregnancy which might lead to neglect of oral hygiene resulting in poor oral hygiene [27]. However contradictory findings were seen by Arafat AHet al. [26].
Oral hygiene Index-simplified (OHI-S) scores were found to increase progressively with the increase in trimester of pregnancy. This finding is supported by the observations of the studies on pregnant women by Samant A et al. [27]. However studies done on pregnant women by Tadkamadla KS et al. [8] in Rajasthan showed no association between deposits of plaque and duration of pregnancy. This could probably be due to the less importance that is given to oral health with progression of pregnancy.
Although the present study was intended to be a longitudinal study design, but due to non availability of the study subjects for repeated examination, cross-sectional design was used which proved to be the major limitation of the study. Also proper matching of the controls to confirm the study findings in future longitudinal studies is recommended.
It was concluded that the prevalence of the Gingival and Periodontal disease was significantly high among pregnant women in comparison to non-pregnant women. Neglect of oral hygiene during pregnancy further deteriorates the condition. The study also highlighted that the pregnant women have large portion of unmet dental needs and possess poor oral health knowledge. These needs have to be met largely through prevention oriented treatment plan by laying more emphasis on self-care measures, and dental care should be provided depending on the trimester of pregnancy. Specific preventive oral health care programme should be made an integral part of antenatal care by including a dentist or dental hygienist in the antenatal team along with gynecologist and pediatrician.
Citation: Jain S, Patthi B, Jain K, Singla A, Kundu H, Singh K (2020) Changing Pattern of Gingivitis and Periodontitis in Different Trimesters among Pregnant Women Comparing the Same with Non Pregnant Women Attending the Government Hospitals in Delhi. Gynecol Obstet (Sunnyvale) 10:541. doi: 10.35248/2161-10932.2020.10.541
Received: 25-May-2020 Accepted: 02-Sep-2020 Published: 10-Oct-2020 , DOI: 10.35248/2161-10932.2020.10.541
Copyright: © 2020 Jain S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.