Research Article - (2023)Volume 9, Issue 4
Characterization of Selected Multidrug-Resistant Bacteria from Clinical and Hospital Environmental Sources Using Vitek 2 Compact System
Emmanuel D. Alabi1*, Binta L. Bindawa2, Ignatius Mzungu1 and Ayodele T. Adesoji1Abstract
Background: Antibiotics Resistant Bacteria (ARB) are a global problem. Patients and hospital environments can be sources for dissemination of ARB that are Multi-drug Resistant (MDR).
Methods: Therefore, we characterized MDR bacteria from clinical and hospital environmental samples from selected hospitals within Katsina state, Nigeria. A total of 203 bacteria were isolated from 420 samples (clinical=220 and hospital environment=200). Bacteria preliminary identification and antibiogram were determined by biochemical tests and Kirby Bauer disk diffusion method, respectively. MDR bacteria were selected based on resistance to ≥ 3 different classes of antibiotics.
Results: Staphylococcus aureus was the most frequently isolated bacteria from clinical samples; i.e., infected surgical incisions (23.58%) and infected trauma wounds (20.75%) and hospital environmental samples; i.e., door handles (32.98%) and desks (14.43%). Highest resistance (92.79%) to both ampicillin and gentamycin was observed among hospital environmental isolates. Clinical isolates showed highest (80.19%) resistance to cefoxitin. MDR bacteria exhibited 12 antibiotics resistance patterns and the most common (20/50) resistance phenotypes among MDR clinical isolates was to amoxiclav, cefoxitin and ciprofloxacin while resistance to ampicillin, chloramphenicol, colistin sulphate, kanamycin and nalidixic acid was commonly (10/50) observed among hospital environmental isolates. Vitek-2-system further detected and characterized Proteus mirabilis, Enterobacter cloacae spp. dissolvens, Enterobacter cloacae and Pseudomonas aeruginosa as MDR isolates with the highest resistance phenotypes.
Conclusions: High occurrence of MDR bacteria in the studied locations portend a great public health consequence and may be disseminated to immunocompromised patients, healthcare workers and the environment. Hence, there is need for concerted AMR surveillance in the study locations.
Keywords
Antimicrobial resistance; Antibiotic resistant bacteria; Antibiotic susceptibility test; Antimicrobial susceptibility testing; Minimum inhibitory concentration; Multidrug resistant bacteria; Healthcare associated infection; Vitek-2 compact system
Introduction
Healthcare Associated Infections (HCAIs) previously referred to as Nosocomial Infections (NIs), are one of the most relevant public health challenges globally. HCAIs are infections acquired by patients on admission in healthcare facilities. Its onset is usually 48-72 hours after the patient's admission (hospitalization), or within 10 days after discharge [1,2]. Several literatures suggested that environmental contamination by pathogenic bacteria plays an important role in the nosocomial transmission and dissemination of multidrug resistant pathogens [3-6].
The burden of HCAIs is further worsened by the global spread of Antimicrobial Resistance (AMR) by multidrug resistant pathogens [7]. These pathogens also constitute agents of occupational infections amongst Healthcare Workers (HCWs) [8]. Invasive medical devices such as indwelling catheters and ventilators used in modern healthcare facilities are also associated with these infections, 7% of every hospitalized patient in developed and 10% in developing countries can acquire these recalcitrant infections [9].
The role of the hospital environment as a reservoir of pathogens responsible for HCAIs is still debated. Pathogens promoting HCAIs are common in several hospital environments, where they are able to persist from hours to months and their transmission to patients is favoured by Healthcare Workers (HCWs). Hospital surfaces at close contact with patients such as bed bars and header, bedside table, taps, and door handles in wards (“high-touched surfaces”), are considered easily contaminable and at risk to transmit pathogens to patients. HCWs’ hands also play a fundamental role in patient to patient transmission by touching contaminated surfaces or patients during care giving activities [10].
Hospitalized patients in Intensive Care Units (ICUs), burn units, and patients undergoing surgeries are those at higher risk of HCAIs. Report from the Extended Prevalence of infection in Intensive Care (EPIC II) study, showed that the figure of infected patients within the ICUs are usually as high as 51% [11]. It is imperative to recognize the basis and modes of spread of infection and implement guidelines on hindrance practices [12]. Obtaining accurate and timely microbiological report shortens the time required to enable the clinicians prescribe and optimize antibiotics treatment sooner and, thus, decrease the deleterious effects of an inappropriate treatment [13].
Vitek 2 compact system is a fast and efficient tool used for identification and susceptibility testing of bacteria in clinical and environmental settings and has been used in monitoring and surveillance to prevent outbreaks of MDR bacteria [14]. It is a broth micro dilution based AST system which uses 64 well plastic cards containing 17 to 20 antimicrobial agents, combinations of susceptibility cards can be done with extension of susceptibility cards resulting in the testing of 18 to 19 additional antimicrobial agents on the same isolate. The Vitek 2 compact system measures changes in turbidity over time (growth curve), comparing a growth control well with wells containing various antibiotics concentrations. Results are obtained in 8-18 hours as Minimum Inhibitory Concentration (MIC) [15].
Due to poor surveillance mechanisms and poor implementation of standard control measures, there is paucity of data on pathogens associated with HCAIs in North-West, Nigeria. Thus, this study seeks to isolate and characterize clinical and environmental Multi-Drug Bacteria (MDR) using Vitek 2 compact system from selected healthcare facilities within Dutsin-Ma and Katsina metropolis in Katsina state-Nigeria.
Materials and Methods
Study areas and sampling locations
Katsina is a state in North-West Nigeria, it lies between the geographic coordinates of 12°59’7.9116” N and 7°37’1.7184” E. The latitude of 12.985531 and the longitude of 7.617144 (Figure 1). It has an area of 23,938 Km2 and a population of 318,132 inhabitants as at the 2006 census [16].
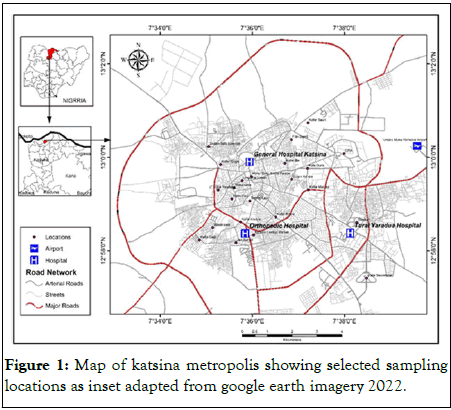
Figure 1: Map of katsina metropolis showing selected sampling locations as inset adapted from google earth imagery 2022.
Dutsin-Ma town is the local government headquarters of Dutsin-Ma local government area in Katsina state-Nigeria. It lies between the geographic coordinates of 12°27’17’’N, 7°29’29’’E. 19 and located on latitude of 12°27'16.13"N and a longitude of 7°29'51.55"E respectively (Figure 2). The local government has an area of 527 km2 and a population of 169,829 inhabitants as at the 2006 census [16].
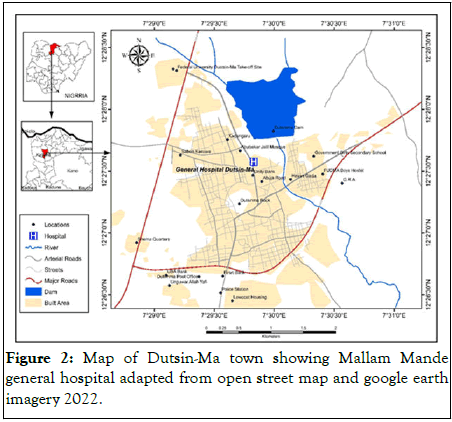
Figure 2: Map of Dutsin-Ma town showing Mallam Mande general hospital adapted from open street map and google earth imagery 2022.
Samples and samples collection
Four hospitals were selected for the study, namely; Mallam Mande General Hospital Dutsin-Ma, General Hospital, Katsina, Turai Yar’adua Maternity and Children’s Hospital, Katsina and General Amadi Rimi Orthopaedic Hospital, Katsina. In this study, a total of 420 samples were collected. Samples include 220 clinical samples obtained from infected surgical incisions, urine samples from patients with prolonged indwelling catheters, skin burns, suppurating wound pus and infected trauma wounds from patients hospitalized in Mallam Mande general hospital Dutsin-Ma and general hospital, Katsina and 200 hospital environmental samples comprising floors, door handles, walls, beds and bedposts, wound dressing tools, bedside desks, tabletops and wards air samples collected from Mallam Mande General Hospital Dutsin-Ma, General Hospital, Katsina, Turai Yar’adua Maternity and Children’s Hospital, Katsina and General Amadi Rimi Orthopaedic Hospital, Katsina respectively. Both clinical and environmental samples were collected aseptically using sterile swab sticks moistened with sterile peptone water between January and October, 2022.
Bacteria isolation and preliminary identification
Samples collected were streaked on mannitol salt agar, cetrimide agar, MacConkey agar without salt and nutrient a agar plates respectively for the isolation of clinical and hospital environmental isolates. Inoculated agar plates were incubated at 37°C in an incubator. Nutrient agar plates were examined after 24 hours for distinct colonies, MacConkey agar plates were observed for lactose and non-lactose fermentation after 24 hours. Mannitol salt agar plates were observed after 48 hours of incubation for visible growth and mannitol fermentation [17], while cetrimide agar plates were examined for the production of pyocyanin and pyoverdine after 48 hours [18]. In order to obtain pure cultures, bacteria isolated on MacConkey agar and nutrient agar were sub-cultured by re-streaking distinct colonies on fresh MacConkey and nutrient agar plates respectively. Distinct colonies (pure cultures) were isolated and stored on double strength nutrient agar slants at 4°C in refrigerator. Each isolate was subjected to preliminary biochemical tests that include; gram staining, catalase test, slide coagulase test, oxidase, indole, methyl red, voges proskauer, citrate utilization, mannitol fermentation, blood haemolysis and triple sugar iron tests.
Antimicrobial susceptibility testing and selection of MDR bacteria isolates
Antimicrobial Susceptibility Testing (AST) of pure isolates was performed on Mueller Hinton agar using Kirby Bauer disk diffusion method. The following antibiotics disks (Oxoid, UK) were used: tetracycline (30 μg), gentamicin (10 μg), cefuroxime (30 μg), ciprofloxacin (5 μg), oxacillin (1 μg), erythromycin (15 μg), sulphamethaxazole/triprimetoprim (25 μg), amoxiclav (30 μg), ampicillin (25 μg), chloramphenicol (50 μg), kanamycin (30 μg), nalidixic acid (30 μg), nitrofurantoin (50 μg), streptomycin (25 μg) and colistin sulphate (100 μg) for screening the isolates. Zones of inhibition were measured in millimeter with a meter rule after incubation at 37°C for 24 hours. Diameters of inhibition w ere i nterpreted u sing clinical and laboratory laboratory standards institute breakpoints protocols. Isolates resistant to three or more different classes of antibiotics were classified and selected as MDR bacteria.
Identification and characterization of selected MDR bacteria using Vitek-2-compact system
Thirty-one (31) randomly selected MDR bacterial isolates were selected for characterization using Vitek 2 compact system. Each bacterial isolate was suspended in 3 milliliters of 0.45% physiological saline solution to the density of 0.5 to 0.60 McFarland measurement using DensiCHEK Plus instrument (Biomerieux, USA). The suspensions were used for both bacterial identification and AST using the Vitek 2 compact system (Biomerieux, USA) according to the manufacturer’s instructions (Biomerieux, USA). All AST inoculum dilutions, card sealing and incubator loading functions were performed by the instrument. Gram Negative (GN) and Gram Positive (GP) cards were used for gram negative and gram positive bacterial identification respectively. The filled and sealed cards were inserted into the Vitek 2 reader incubation chamber and incubation was performed at temperature 35.5°C.
Gram positive and Gram negative AST cards were used for Gram positive and Gram negative AST respectively using Vitek-2-compact system. MDR isolates were tested against different classes of antibiotics representing aminoglycosides, penicillins, Carbapenems, cephalosporins, quinolones, tetracyclines and sulphonamides. Optical reading of cards was performed every 15 minutes by the Vitek 2 compact system, with a multi channeled fluorometer and photometer to record fluorescence, turbidity, and colorimetric signals. Susceptibility results were obtained in 8-18 hours, depending on the organism and susceptibility parameters. At the completion of the incubation cycle, bacterial isolates were identified, and MIC values were determined for each antibiotic contained on the card. The detection of antimicrobial resistance was facilitated by the Advanced Expert System (AES). This software system validates MIC results by a set of in vitro testing rules based on 20,000 MIC distributions with over 2000 phenotypes and provides result interpretations and corrections; it may further add footnotes (CLSI or laboratory defined). Results were interpreted according to the clinical and laboratory standards institute breakpoints.
Results
A total of 420 samples were collected from both clinical (n=220) and hospital environmental (n=200) sources (Table 1), out of which 203 bacterial isolates (clinical isolates=106, hospital environment isolates=96) were obtained. Staphylococcus aureus was the most frequently isolated presumptive bacteria from both clinical and hospital environmental samples showing 23.58%, 20.75%, 32.98% and 14.43% occurrence from infected surgical incision, infected trauma wounds, door handles and desks, respectively. Pseudomonas aeruginosa and Streptococcus spp. were the least presumptive isolates from the hospital environment showing 2.06%percentage occurrence each from hospital walls and on wound dressing instruments respectively (Table 2). Among hospital environmental isolates screened, 92.79% showed resistance to both Ampicillin (AMP) and Gentamycin (GEN) respectively, while the lowest 44.33% resistance was to Kanamycin (KAN). Conversely, clinical isolates exhibited the highest (80.19%) resistance to cefoxitin (FOX) and the lowest (20.75%) resistance to Colistin sulphate (CO) (Table 3). A total of 82 (40.39%) MDR bacteria were obtained after AST on all isolates (Table 4). Higher occurrence (50/82; 60.97%) of MDR bacteria were found in the clinical samples compared to hospital environmental samples (32/82; 39.03%).
| Clinical samples (n=220) | Hospital environmental samples (n=200) | ||||
|---|---|---|---|---|---|
| Sources | Number of samples collected | Percentage of total clinical samples (%) | Sources | Number of samples collected | Percentage of total hospital environmental (%) |
| Infected surgical incisions | 70 | 31.81 | Floors | 30 | 15 |
| Urine (prolonged indwelling catheter) | 40 | 18.19 | Walls | 30 | 15 |
| Skin Burns | 35 | 15.9 | Door handle | 40 | 20 |
| Infected trauma wounds | 50 | 22.73 | Desks | 30 | 15 |
| Suppurating wound Pus | 25 | 11.37 | Beds | 30 | 15 |
| Wound dressing instruments | 20 | 10 | |||
| Wards air samples | 20 | 10 | |||
| Total | 220 | 100 | 200 | 100 | |
Table 1: Number of samples collected from clinical and hospital environmental sources within Katsina and Dutsin-Ma Metropolis.
| Clinical isolates (n=106) | Hospital environmental isolates (n=97) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sources | Number of samples collected (n) | Suspected Bacteria | Number of suspected bacteria isolated | Percentage occurrence (%) | Sources | Number of samples collected (n) | Suspected Bacteria | Number of suspected bacteria isolated | Percentage occurrence (%) |
| Infected surgical incision | 70 | S. aureus Streptococcus sp. | 25 8 |
23.58 7.56 | Floor | 30 | P. aeruginosa Bacillus sp. | 5 6 |
5.15 6.19 |
| Urine (prolonged indwelling catheters) | 40 | E. coli Proteus sp. P. aeruginosa | 11 3 1 |
10.38 2.83 0.94 | Wall | 30 | Bacillus sp. P. aeruginosa | 7 2 |
7.22 2.06 |
| Skin Burns | 35 | P. aeruginosa | 9 | 8.49 | Door handles | 40 | S. aureus | 32 | 32.98 |
| Infected trauma wounds | 50 | S. aureus Streptococcus sp. | 22 7 |
20.75 6.6 | Desk | 30 | S. aureus | 14 | 14.43 |
| Suppurating wound Pus | 25 | S. aureus Streptococcus sp. | 16 4 |
15.1 3.77 | Bed | 30 | Bacillus sp. Staphylococcus sp. | 7 10 |
7.22 10.31 |
| Wound dressing instruments | 20 | S. aureus Streptococcus sp. | 6 2 |
6.19 2.06 | |||||
| Wards air samples | 20 | Bacillus sp. | 6 | 6.19 | |||||
| Total | 220 | 106 | 100 | 200 | 97 | 100 | |||
Table 2: Occurrence of bacterial isolates from clinical and hospital environmental samples within Katsina and Dutsin-Ma metropolis.
| Clinical isolates (n=106) Hospital environmental isolates (n=97) | ||||
|---|---|---|---|---|
| Antibiotics | Number of resistant isolates (%) | Number of resistant isolates (%) | Number of susceptible isolates (%) | Number of susceptible isolates (%) |
| CIP | 57 (53.77) | 49 (46.23) | 79 (81.44) | 18 (18.56) |
| FOX | 85 (80.19) | 21 (19.81) | 52 (53.61) | 45 (46.39) |
| AMC | 80 (75.47) | 26 (24.53) | 85 (87.63) | 12 (12.37) |
| TET | 53 (50.00) | 53 (50.00) | 71 (73.20) | 26 (26.80) |
| AMP | 80 (75.47) | 26 (24.53) | 90 (92.79) | 7 (7.21) |
| ERY | 40 (37.34) | 66 (62.26) | 52 (53.61) | 45 (46.39) |
| CO | 22 (20.75) | 84 (79.25) | 45 (46.39) | 52 (53.61) |
| KAN | 43 (46.23) | 63 (59.43) | 43 (44.33) | 54 (55.67) |
| NI | 80 (75.47) | 26 (24.53) | 60 (61.86) | 37 (38.14) |
| NA | 53 (50.00) | 53 (50.00) | 60 (61.86) | 37 (38.14) |
| GEN | 46 (43.40) | 60 (56.60) | 90 (92.79) | 7 (7.21) |
| CXM | 81 (76.42) | 25 (23.58) | 85 (87.63) | 12 (12.37) |
| S | 79 (74.53) | 27 (25.47) | 52 (53.61) | 45 (46.39) |
| CPC | 66 (62.26) | 40 (37.74) | 70 (72.16) | 27 (27.84) |
| OX | 40 (37.34) | 66 (62.26) | 52 (53.61) | 45 (46.39) |
| Note: CIP: Ciprofloxacin; FOX: Cefoxitin; AMC: Amoxiclav; CXM: Cefuroxime; GEN: Gentamicin; TET: Tetracycline; ERY: Erythromycin; AMP: Ampicillin; CPC: Chloramphenicol; CO: Colistin Sulphate; K: Kanamycin; NA: Nalidixic Acid; NI: Nitrofurantoin; S: Streptomycin; OX: Oxacillin | ||||
Table 3: Antibiotics resistance profile of bacterial isolates from clinical and environmental sources.
| Sources | Number of Antibiotics | Resistance phenotypes | Number of isolates (%) |
|---|---|---|---|
| Clinical | 3 | CIPFOXAMC | 20 |
| 4 | CIPFOXAMCCXM | 9 | |
| 5 | CIPFOXAMCCXMTET | 7 | |
| 6 | CIPFOXAMCCXMTETERY | 4 | |
| 7 | CIPFOXAMCCXMTETERYOX | 3 | |
| 8 | CIPFOXAMCCXMTETERYFOXGEN | 7 | |
| 50 (60.97) | |||
| Environments | 3 | AMPCPCCO | 5 |
| 4 | AMPCPCCOK | 6 | |
| 5 | AMPCPCCOKNA | 10 | |
| 6 | AMPPCPCCOKNANI | 2 | |
| 7 | AMPCPCCOKNANIS | 5 | |
| 8 | AMPCPCCOKNANISTET | 4 | |
| Total phenotypes 12 | 32 (39.02) | ||
| Note: CIP: Ciprofloxacin; FOX: Cefoxitin; AMC: Amoxiclav; CXM: Cefuroxime; GEN: Gentamicin; TET: Tetracycline; ERY: Erythromycin; AMP: Ampicillin; CPC: Chloramphenicol; CO: Colistin Sulphate; K: Kanamycin; NA: Nalidixic Acid; NI: Nitrofurantoin; S: Streptomycin; OX: Oxacillin | |||
Table 4: Multiple antibiotics resistance phenotypes among MDR bacteria from clinical and hospital environmental sources within Katsina and Dutsin-Ma metropolis.
Twelve (12) different antibiotics resistance phenotypes were identified from this study (Table 4), the multiple antibiotics resistance pattern to Ciprofloxacin (CIP), Cefoxitin (FOX) and amoxiclav (AMC) was the most (20/50) frequently observed pattern in clinical isolates while the least (3/50) observed antibiotics resistance pattern among these isolates was to Ciprofloxacin (CIP), Cefoxitin (FOX), Amoxiclav (AMC), Cefuroxime (CXM), Tetracycline (TET), Erythromycin (ERY) and oxacillin (OX). Most (10/32) isolated bacteria from hospital environmental sources showed multiple antibiotics resistance patterns to Ampicillin (AMP), Chloramphenicol (CPC), Colistin sulphate (CO), Kanamycin (K) and Nalidixic Acid (NA) and the least (2/32) observed antibiotics resistance patterns was to Ampicillin (AMP), Chloramphenicol (CPC), Colistin sulphate (CO), Kanamycin (K), Nalidixic Acid (NA) and Nitrofurantoin (NI) respectively.
Vitek 2 compact system revealed the identities and antibiogram profiles of the 31 randomly selected MDR isolates with multiple antibiotics resistance to various classes of antibiotics (Table 5). The isolates with the highest frequencies of occurrence are Pseudomonas aeruginosa (9/31; 29.03%), kocuria kristinae (5/31; 16.13%), Ochrobactrum anthropi (3/31; 9.68%), Enterobacter cloacea and Enterobacter cloacea spp dissolvens (3/31; 9.68%) respectively. However, clinical isolates that showed the highest resistance phenotypes are; Proteus mirabilia, Pseudomonas aeruginosa, Enterococcus gallinarum and Staphylococcus aureus while the least resistance phenotypes recorded were from Kocuria kristinae respectively. Isolates with the highest frequencies from hospital environments are Pseudomonas aeruginosa, Kocuria kristinae, Ochrobactrum anthropi, Enterobacter cloacea and Enterobacter cloacea spp dissolvens, and the highest resistance phenotypes recorded were from Pseudomonas aeruginosa, Enterobacter cloacea spp dissolvens, Enterobacter cloacea, Enterococcus faecalis, Enterococcus gallinarum, Proteus mirabilis, Staphylococcus haemolyticus, Staphylococcus aureus, Kocuria kristinae and Ochrobactrum anthropi, and the least resistance phenotypes recorded were from Staphylococcus vitulinus, Chromobacterium violaceum and Providencia stuartii respectively.
| Bacterial genera | Percentage Identities | Presumptive Bacteria | Sources | Resistance phenotypes |
|---|---|---|---|---|
| Clinical Isolates | ||||
| Proteus mirabilis | 99% | Proteus sp. | Urine | AMPCEFOPIPCEFAZLEVOCIPRONITROCEFTRIACEFEPCEFTAAMP/SULBA |
| Staphylococcus aureus | 95% | S. aureus | wound swab | CIPOXATETVANCLIND |
| Kocuria kristinae | 89% | S. aureus | wound swab | AMPCPCCOLKAN |
| Pseudomonas aeruginosa | 98% | streptococcus sp. | wound swab | AMPCEFOCEFAZNITROCETRIAAMP/SULBATRIM/SULF |
| Enterococcus gallinarum | 90% | streptococcus sp. | wound swab | LEVO*CIPROERYT*TETVANCOCLINDMOXISHL-RGHL-R |
| Hospital environmental isolates | ||||
| Ochrobactrum anthropi | 93% | P. aeruginosa | Ward wall | AMPCPCCOL |
| Kocuria kristinae | 94% | S. aureus | Ward Door handle | NAAMPCPCCOL |
| Ochrobactrum anthropi | 93% | Staphylococcus sp. | Bed | AMPCPCCOL |
| Streptococcus thoraltensis | 93% | Bacillus sp. | Female ward Floor | AMPCPCCOLKAN |
| Chromobacterium violaceum | 90% | Bacillus sp. | Female ward Floor | AMPCPCCOL |
| Sphingomonas paucimobilis | 85% | P. aeruginosa | ICU Floor | AMPPIPLEVOCIPRO |
| Enterobacter cloacea spp dissolvens | 95% | P. aeruginosa | ICU Floor | CEFCEFAZGENTLEVONITROCEFTRIACEFEPCEFTAMEROPTRIM/SULTOBRA |
| Kocuria kristinae | 94% | Bacillus sp. | Male ward Floor | NAAMPCPCCOL |
| Kocuria kristinae | 99% | S. aureus | Ward Door handle | AMPCPCCOLKANNANIS |
| Ochrobactrum anthropi | 91% | Streptococcus sp. | Wound dressing scissors | AMPCPCCOL |
| Staphylococcus haemolyticus | 98% | Bacillus sp. | Ward Floor | CEFOLEVOCIPROTRIM/SULFOXAERYTETRIFDOXYCLIND |
| Pantoea sp. | 90% | P. aeruginosa | Ward Floor | AMPCPCCOLKANNA |
| Enterobacter cloacea | 93% | S. aureus | A/E Desk | CEFOPIPCEFAZGENTLEVO*CIPRONITRO*CETRIACEFEPCEFTATRIM/SULF |
| Pseudomonas aeruginosa | 97% | Bacillus sp. | Bed | CETRIAAMP/SULBATRIM/SULFAMPCEFOCEFAZNITRO |
| Pseudomonas aeruginosa | 97% | S. aureus | Desk | AMPCEFOCEFAZNITROCETRIAAMP/SULBATRIM/SULF |
| Pseudomonas aeruginosa | 97% | P. aeruginosa | Maternity Floor | AMPCEFOCETRIAAMP/SULBATRIM/SULFCEFAZNITRO |
| Pseudomonas aeruginosa | 91% | P. aeruginosa | Ward Wall | AMPCEFOCEFAZNITROCETRIAAMP/SULBATRIM/SULF |
| Staphylococcus vitulinus | 90% | S. aureus | Ward Door handle | CIPFOXAMC |
| Pseudomonas aeruginosa | 98% | P. aeruginosa | Maternity Floor | NITROCETRIAAMP/SULBATRIM/SULFAMPCEFOCEFAZ |
| Pseudomonas aeruginosa | 95% | P. aeruginosa | Ward Wall | CETRIAAMP/SULBATRIM/SULFAMPCEFOCEFAZNITRO |
| Pseudomonas aeruginosa | 98% | P. aeruginosa | A/E Wall | AMPCEFOCEFAZNITROCETRIAAMP/SULBATRIM/SULF |
| Kocuria kristinae | 89% | Bacillus sp. | A/E Floor | AMPCPCCOL |
| Enterobacter cloacea | 96% | S. aureus | Ward Door handle | CEFOPIPCEFAZGENTNITRO*CEFTRIATRIM/SULFTOBRA* |
| Pseudomonas aeruginosa | 98% | P. aeruginosa | A/E Floor | AMPCEFOCEFAZNITROCETRIAAMP/SULBATRIM/SULF |
| Enterococcus faecalis | 99% | S. aureus | A/E Door handle | AMPERYTTETDOXYVANCCLINDMOXI*SHL-R |
| Providencia stuartii | 92% | P. aeruginosa | A/E Wall | AMPCPCCOL |
| Note: AMP: Ampicillin; CEFO: Cefoxitin; CIPRO: Ciprofloxacin; NITRO: Nitofurantoin; TRIM/SULF: Trimethoprim/ Sulfamethoxazole; CEFEP: Cefepime; CEFTA: Ceftazidime; CEFAZ: Cefazolin; PIP: Piperacillin; ERTA: Ertapenem; MEROP: Meropenem; AMIK; Amikacin; TOBRA; Tobramycin; LINE: Linezolid; DAPTO: Daptomycin; DOXY: Doxycycline; TIGE: Tigecycline; RIFAM: Rifampicin; MOXI: Moxifloxacin; CEFTRIA: Ceftriaxone; AMP/SULBA: Ampicillin/Sulbactam; GENT: Gentamycin; OXAC: Oxacillin; LEVO: Levofloxacin; CLIND: Clindamycin; SHL-R: Streptomycin High Level (synergy); GHL-R: Gentamycin High Level (synergy); TET: Tetracycline; VANC: Vancomycin; ERY: Erythromycin; CPC: Chloramphenicol; COL: Colistin Sulphate; KAN: Kanamycin; S: Streptomycin; *=Intermediate; Wound swab: Infected Trauma Wound; A/E: Accident and Emergency; GP: Gram Positive; GN: Gram Negative | ||||
Table 5: Phenotypes and antibiotics resistant profiles of selected multi-drug resistant isolates identified using Vitek 2 compact system from clinical and hospital environmental isolates.
Discussion
Several scientific reports have revealed the role of contaminated hospital environment in harboring and dissemination of MDR pathogens and the resultant risk of HCAI amid the global incidence of antimicrobial resistance that has increased the rate of morbidity and mortality globally [19,20]. In this study, we isolated various bacterial strains associated with HCAIs from both clinical and hospital environmental sources (Table 1). Staphylococcus aureus had the highest frequency of occurrence (32.98% and 23.58%) from both environmental and clinical sources respectively. This is higher than the report of Gastmeier, et al., that analyzed 1022 nosocomial outbreaks and observed 14.8% of the outbreaks was attributed to S. aureus. On the other hand, outbreaks of Methicillin-Resistant S. aureus (MRSA) due to environmental contamination have also been previously reported [21,22]. The high occurrence of S. aureus from infected surgical incisions (23.58%) and door handles (32.98%) in this study may be attributed to the fact that Staphylococcus is a normal flora of the body and can readily be shed to colonize surgical incisions during or after surgical operations and can be disseminated via the skin to "highly touched surfaces" like door handles, this is evident as S. aureus was isolated from wound dressing instruments (6.19%) and door handles (32.98%) respectively in this study.
The occurrence of Pseudomonas aeruginosa from clinical (8.49%) and environmental (5.15%) sources respectively (Table 2), agrees with similar studies conducted in Nigeria and Uganda, which showed higher prevalence rates in hospital environments and residential sewage run-offs as high as 86.4%, 66.7%, and 33%, respectively, while infection among burn patients was reported to be 59.6%, 53.97%, and 37.5%, respectively [23-26]. Although P. aeruginosa is a widespread soil bacterium [27], it has been identified as one of the leading pathogens causing HCAIs worldwide [7,28]. In this study, Pseudomonas aeruginosa was frequently isolated from clinical samples compared to environmental samples. Regrettably, vulnerable and immunocompromised patients may be at risk of infections due to the dissemination of MDR Pseudomonas aeruginosa from patient-to-patient during care-giving activities by HCWs hands. Furthermore, hospital environmental isolates demonstrated highest resistance to ampicillin (92.79%) and amoxiclav (87.63%) and least resistance to kanamycin (44.33%), whereas clinical isolates demonstrated highest resistance to cefoxitin (80.19%) and amoxiclav (75.47%) and least resistance to colistin sulfate (20.75%), respectively, a similarly high rate (76.4%) was found among clinical isolates; S. aureus, Pseudomonas aeruginosa and Klebsiella pneumoniae in Cameroon [29]. Several S. aureus isolated in this study were resistant to cefoxitin. Felten, et al., reported that cefoxitin disk diffusion tests have been used to detect 100% of all MRSA classes [30]. Moreover, high resistance to cephalosporins class of antibiotic (cefoxitin) and beta-lactam antibiotics (amoxiclav and ampicillin) by clinical and hospital environmental isolates in this study, may be attributed to doctors' frequent use of empirical prescriptions before patients’ microbiological test results are available, and the release of wastewater containing high quantities of antibiotics that are incompletely metabolized, disinfectants, by-products of hospital procedures and patient treatment which is often discharged to septic tanks or allowed to flow through canals without any pre-treatment [31], this practice poses serious public health concerns amidst the global surge in AMR.
Furthermore, the resistance to cephalosporins and beta-lactam antibiotics tested may also be attributed to the production of beta-lactamase, an enzyme that inactivates β-lactam rings in β-lactam antibiotics and closely related antibiotics. Isolates that showed similarity in their antibiotics resistance patterns may have a possible genetic link due to horizontal gene transfer resulting from mobile elements harbouring antibiotics resistance genes [32]. On the contrary, colistin sulphate and kanamycin resistance was the least observed in both clinical and environmental isolates respectively. This agrees with other studies who studied aminoglycosides resistance in clinical and environmental isolates [33,34].
Vitek 2 compact system as an efficient diagnostic tool gave the explicit identities of isolates and confirmed the antibiogram profiles of previously screened MDR isolates and revealed other resistance phenotypes, several other pathogens that could not be tentatively identified with conventional biochemical tests were also detected. The system detected kocuria kristinae which are often misidentified or misinterpreted as contaminants of clinical and environmental specimens but have been reported to cause bacteraemia and recurrent sepsis, endocarditis and pneumonia particularly in immunocompromised patients and in patients with indwelling medical devices [35-39]. Vitek 2 compact system also detected MDR Enterobacter cloacea and extensively drug resistant (XDR) Enterobacter cloacea spp dissolvens respectively, this is similar to the findings of Wilson, et al., where they reported Enterobacter spp. as the second most common nosocomial pathogens capable of producing a wide range of infections such as; pneumonia, urinary tract infections, septicemia and have emerged as healthcare acquired pathogens from intensive care patients, especially from those on mechanical ventilation in the United States, which has increasingly contributed to the dissemination of carbapenem-resistant infections [40-43]. Enterococcus gallinarum and Enterococcus faecalis organisms found in the normal bowel microbiota of humans and many animals were also detected by Vitek 2 compact system, they have been reported to colonize soft tissue wounds, ulcers, and the gastrointestinal tract of hospitalized patients and cause bloodstream infections, and have also been reported to cause meningitis in Doha, Qatar and Shenyang, China respectively [44,45]. Thus, the Vitek 2 compact system is a very important tool for surveillance, rapid characterization and antimicrobial susceptibility testing in clinical and environmental settings in low and middle-income countries where diagnosis and treatment of multi-drug resistant pathogens can be difficult and expensive, results are usually available within 8-18 hours and can help reduce routine empirical prescription by clinicians and ultimately improve the patients’ diagnosis and treatment outcome.
Conclusion
This study has given an insight that multi-drug-resistant pathogens abound in the studied hospital environments and may be a source of healthcare-associated infections. Therefore, surveillance mechanisms, Infection Prevention and Control (IPC), and improved sanitary measures should be deployed to monitor healthcare facilities for the detection of agents of HCAI at the earliest possible stage. Most importantly, public education and awareness on the risks associated with the indiscriminate use and abuse of antibiotics should be improved amongst the populace.
Ethical Approval and Consent to Participate
Ethical approval to carry out this study was obtained from the ethical review committee of Katsina state ministry of health with approval number: MOH/ADM/SUB/1152/1/556.
Informed Consent
The manuscript does not contain any individual persons’ data in any form.
Consent for Publication
We certify that the submission is original work and is not under review elsewhere.
Data Availability Statement
The authors assert that the data supporting the findings of this study are available.
Competing Interests
The authors declare that they have no competing interests.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
IM, ATA and EDA designed the study; EDA and BLB carried out the laboratory work; EDA wrote the first draft and the final manuscript of the article; BLB, IM and ATA went through the final manuscript; all the authors have read and approved the final version of the manuscript.
Acknowledgements
The authors would like to thank the management and staff members of the hospitals where samples were collected and Mr. Tayo Abdulkadir, department of geography and regional studies, Federal university Dutsin-Ma, Katsina state-Nigeria, who designed the maps of the sampling locations using GIS.
References
- Pittet D, Allengranzi B, Storr J, Donaldson L. ‘Clean care is safer care’: The global patient safety challenge 2005-2006. Int J Infect Dis. 2006;10(6):419-424.
[Crossref] [Google Scholar] [PubMed]
- Haque M, Sartelli M, McKimm J, Bakar MA. Health care-associated infections; An overview. Infect Drug Resist. 2018;(11):2321-2333.
[Crossref] [Google Scholar] [PubMed]
- Dancer SJ. Controlling hospital-acquired infection: Focus on the role of the environment and new technologies for decontamination. Clin Microbiol Rev. 2014;27(4):665-690.
[Crossref] [Google Scholar] [PubMed]
- Sood G, Perl TM. Outbreaks in health care settings. Infect Dis Clin North Am. 2016;30(3):661-687.
[Crossref] [Google Scholar] [PubMed]
- Huslage K, Rutala WA, Sickbert-Bennett E, Weber DJ. A quantitative approach to defining “high-touch” surfaces in hospitals. Infect Control Hosp Epidemiol. 2010; 31(8):850-853.
[Crossref] [Google Scholar] [PubMed]
- Otter JA, Yezli S, Salkeld JA, French GL. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control. 2013;41(5):S6-S11.
[Crossref] [Google Scholar] [PubMed]
- Wu N, Zhu T. Potential of therapeutic bacteriophages in nosocomial infection management. Front Microbiol. 2021;12:638094.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization (2016) Prevention of hospital acquired infections. A practical guide. Department of Communicable Disease, Surveillance and Response.
- Khan HA, Baig FK, Mehboob R. Nosocomial infections: Epidemiology, prevention, control and surveillance. Asian Pac J Trop Biomed. 2017;7(5):478-482.
- Facciola A, Pellicano GF, Visalli G, Paolucci IA, Venanzi Rullo E, Ceccarelli M. et al. The role of the hospital environment in the healthcare associated infections: A general review of the literature. Eur Rev Med Pharmacol Sci. 2019;23(3):1266-1278.
[Crossref] [Google Scholar] [PubMed]
- Wang W, Zhu S, He Q, Zhang R, Kang Y, Wang M. et al. Developing a registry of healthcare-associated infections at intensive care units in West China: Study rationale and patient characteristics. Clin Epidemiol. 2019;11:1035-1045.
[Crossref] [Google Scholar] [PubMed]
- Chandra PN, Milind K. Lapses in measures recommended for preventing hospital acquired infection. J Hosp Infect. 2001;47(3):218-222.
[Crossref] [Google Scholar] [PubMed]
- Galar A, Yuste JR, Espinosa M., Guillen-Grima, Hernaez-Crespo S, Leiva J. Clinical and economic impact of rapid reporting of bacterial identification and antimicrobial susceptibility results of the most frequently processed specimen types. Eur J Clin Microbiol Infect Dis. 2012;31(9):2445-2452.
[Crossref] [Google Scholar] [PubMed]
- Tshabuse F, Buthelezi N, Folami AM, Donnelly L, Swalaha FM. Rapid detection of drug-resistant Escherichia coli by Vitek 2 compact system. Water SA. 2022;48(4):450-456.
- Alan TE, James AK. Manual of commercial methods in clinical microbiology. Second Edition. John Wiley and Sons. 2016;416-418.
- Cheesbrough M. District laboratory practice in tropical countries, part 2. Cambridge university press. 2005;132-142.
- Alonso B, Fernandez-Barat L, di Domenico, EG, Marin M. Characterization of the virulence of Pseudomonas aeruginosa strains causing ventilator associated pneumonia. BMC Infect Dis. 2020;20(1):909.
[Crossref] [Google Scholar] [PubMed]
- Chemaly RF, Simmons S, Dale C Jr, Ghantoji SS, Rodriguez M, Gubb J, et al. The role of the healthcare environment in the spread of multidrug-resistant organisms: Update on current best practices for containment. Ther Adv Infect Dis. 2014;2(4):79-90.
[Crossref] [Google Scholar] [PubMed]
- Rampling A, Wiseman S, Davis L, Hyett AP, Walbridge AN, Payne GC, et al. Evidence that hospital hygiene is important in the control of methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2001;49(2):109-116.
[Crossref] [Google Scholar] [PubMed]
- Gastmeier P, Stamm-Balderjahn S, Hansen S, Nitzschke-Tiemann F, Zuschneid I, Groneberg K. et al. How outbreaks can contribute to prevention of nosocomial infection: Analysis of 1,022 outbreaks. Infect Control Hosp Epidemiol. 2005;26(4):357-361.
[Crossref] [Google Scholar] [PubMed]
Author Info
Emmanuel D. Alabi1*, Binta L. Bindawa2, Ignatius Mzungu1 and Ayodele T. Adesoji12Department of Medical Laboratory Science, Kankia Iro School of Health Technology Kankia, College of Health Sciences and Technology, Katsina, Nigeria
Citation: Alabi ED, Bindawa BL, Mzungu I, Adesoji AT (2023) Characterization of Selected Multidrug-Resistant Bacteria from Clinical and Hospital Environmental Sources Using Vitek 2 Compact System. Appli Microbiol Open Access. 9:258.
Received: 20-Apr-2023, Manuscript No. AMOA-23-23660; Editor assigned: 24-Apr-2023, Pre QC No. AMOA-23-23660 (PQ); Reviewed: 08-May-2023, QC No. AMOA-23-23660; Revised: 22-Jun-2023, Manuscript No. AMOA-23-23660 (R); Published: 29-Jun-2023 , DOI: 10.35248/2471-9315.23.9.258
Copyright: © 2023 Alabi ED, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.