Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2024)Volume 9, Issue 3
Aim: To analyse the presentations of paediatric Diabetic Ketoacidosis (DKA) to black town and mount druitt hospitals over a 10-year period to assess the associated travel burden incurred to receive care from the closest tertiary referral centre for their families to receive care from the closest tertiary referral center, we gain insights into the accessibility and utilization of healthcare services, particularly for conditions as critical as DKA in pediatric patients.
The analysis involves delving into various aspects, including the frequency and severity of DKA presentations, demographic characteristics of the affected population and the geographical distribution of patients seeking care at these hospitals. By examining trends over a decade, patterns may emerge that shed light on potential factors influencing DKA incidence and management in these communities.
Furthermore, evaluating the travel burden faced by families adds another layer of understanding to the healthcare landscape. Factors such as distance to the tertiary referral center, transportation options available, socioeconomic status of families and potential barriers to accessing care may all play a role in determining the extent of this burden. This analysis could uncover disparities in healthcare access and inform strategies to mitigate them, ensuring equitable access to quality care for all pediatric patients, irrespective of their geographical location or socioeconomic background.
Moreover, exploring the impact of travel burden on health outcomes, such as delays in seeking treatment, exacerbation of DKA symptoms and complications arising from suboptimal management, provides valuable insights for healthcare policymakers and providers. By identifying areas for improvement in the healthcare system, such as enhancing transportation infrastructure, expanding telehealth services or implementing community outreach programs, we can work towards reducing the burden on families and improving the overall management of pediatric DKA.
Methods: Retrospective review of data on all patients ≤ 16 years who presented with DKA to black town and mount druitt hospitals between 2008 and 2017.
Results: Of the 79 DKA presentations including 53 first presentations, the mean age was 12 years. Fifty-two percent of patients presented with moderate or severe DKA and 63.3% (50 patients) were acutely transferred for further expert management. The mean difference travel distance for patients from their usual residence to the Children’s Hospital at Westmead (CHW) compared to or Black Town Hospital (BH) and Mount Druitt Hospital (MDH) was eight and 16 kilometres respectively, translating to an additional 15 and 36 minutes respectively by public transport.
Conclusions: Establishing local paediatric diabetes services to improve access to care may overcome the challenge of distance. This can facilitate follow up in the long-term and potentially reduce the number of hospital presentations with DKA. Moreover, the availability of local services may empower primary care providers to manage diabetes more effectively, thus reducing the reliance on tertiary care centers for acute management and potentially decreasing the number of hospital presentations with DKA. In addition to improving access to care, local pediatric diabetes services can foster a sense of community and support among families facing similar challenges. This can be particularly beneficial for parents/caregivers in navigating the complexities of managing a chronic condition like diabetes in their children. Overall, investing in local pediatric diabetes services has the potential to enhance the quality of care, reduce healthcare disparities and ultimately improve outcomes for children with diabetes in underserved areas.
Diabetes mellitus; Diabetic ketoacidosis; Children; Hyperglycaemia
Diabetic Ketoacidosis (DKA) occurs when there is a combination of hyperglycaemia, insulin deficiency, metabolic acidosis and ketonaemia or ketonuria [1]. Based on registration data with the National Diabetes Services Scheme (NDSS), we estimate that in our catchment area there are at least 40 children under 10 years of age with type 1 Diabetes Mellitus (DM). Specialized paediatric diabetes services do not currently exist in either local non-specialist hospital (Blacktown or Mount Druitt Hospital), despite the local population having a large burden of diabetes and an increased odds ratio of developing DM [2,3].
Acute care provided by the general paediatric services in these hospitals is limited to mild DKA. Children with more severe DKA are transferred to the closest tertiary paediatric endocrinological service, at the Children’s Hospital at Westmead (CHW), situated further east. For chronic care, children are managed either at CHW or the next closest paediatric endocrine service, to the west of our local health district.
In this study we review the hospital presentations and estimate the impact of distance on the families of children with DKA over a 10-year period. Specifically, we will examine the severity of DKA at presentation, healthcare utilization patterns and clinical outcomes in relation to the distance between patients' residences and the nearest pediatric endocrine service.
By elucidating the relationship between distance and DKA outcomes, we hope to identify potential barriers to care and inform strategies to improve access to pediatric diabetes services. Addressing these barriers is essential for optimizing the management of pediatric diabetes, reducing the burden of DKA and improving the overall health and well-being of affected children and their families.
This retrospective study reviewed all paediatric DKA presentations at Blacktown and Mount Druitt Hospitals in western Sydney, Australia. The research was performed in accordance with the Declaration of Helsinki and was approved by the Western Sydney Local Health District Human Research Ethics Committee (WSLHD HREC) (1906-06 QA).
Inclusion criteria for this study were: (1) Individuals ≤ 16 years of age and (2) An admission with a final diagnosis of DKA between January 2008 and December 2017.
Clinical and demographic data were extracted from electronic medical records. The mean travel distance from usual place of residence to the different local hospitals was calculated i.e. home to Blacktown Hospital (BH) or Mt Druitt Hospital (MDH) vs home to the tertiary referral centre. Figure 1 illustrates the locations of the hospitals relative to each other. Statistical analysis was undertaken using Excel Version 16.66.1 (2022).
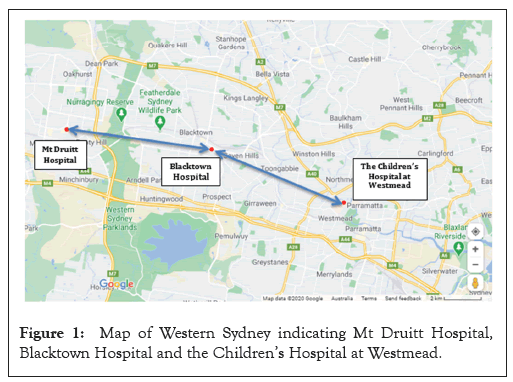
Figure 1: Map of Western Sydney indicating Mt Druitt Hospital, Blacktown Hospital and the Children’s Hospital at Westmead.
There were 79 presentations in total, 53 presenting with the first episode of DKA. Mean age was 12 years and fifty patients (63.3%) required transfer to another hospital for tertiary care. Mean travel distance and time were longer to BH compared to MDH. The extra distance families would have had to travel on average to the CHW compared to BH or MDH were 8 and 16 km respectively. This corresponded to an extra 8 or 16 minutes by car or an extra 15 or 36 minutes by public transport respectively (Table 1). Furthermore, exploring potential strategies to mitigate the challenges posed by extended travel distances, such as telemedicine consultations or community-based outreach programs, could enhance the overall efficiency and effectiveness of healthcare delivery for pediatric patients requiring specialized care. By addressing these logistical barriers, healthcare systems can strive towards ensuring timely access to appropriate medical interventions, ultimately optimizing patient outcomes and reducing the burden on families navigating complex healthcare pathways.
| Blacktown Hospital (BH) |
Mt Druitt Hospital (MDH) |
The Children’s Hospital at Westmead (CHW) |
Extra travel to CHW |
|||
|---|---|---|---|---|---|---|
| Time (minutes) | Personal vehicle (car) | 17 | 9 | 25 | BH | MDH |
| 8 | 16 | |||||
| Public transport | 65 | 44 | 80 | 15 | 36 | |
| Distance (km) | 15 | 7 | 23 | 8 | 16 | |
Note: BH: Blacktown Hospital; MDH: Mt Druitt Hospital; CHW: Children’s Hospital at Westmead.
Table 1: Average travel distances and times from home to hospitals.
Severe DKA requires management in a tertiary paediatric centre. Access for immediate and ongoing care at the closest centre compared to their local hospitals incurs a cost (distance and time) to these families.
The care of children with DM has financial impacts on families, including lost wages due to time off work [4,5]. Informal burdens include choice of employment, socialisation activities and school absenteeism. Carers view longer travel times as barriers to care and have been associated with poorer metabolic control and lower levels of caregiver satisfaction. These negative effects might be mitigated if local specialized services were available [5-7].
A diabetes outreach model can achieve similar metabolic control to care in a tertiary centre [8]. Investing in an outreach service with emphasis on local capacity building and staff education may result in long-term benefit. Outreach services can also be provided by telehealth and has been proposed even before COVID-19, but has logistic barriers and is not always the preferred option by children or parents. A shared care model between paediatric endocrinologists and general paediatricians is another approach [9-13]. We are much closer to tertiary services than rural and remote units. Thus paradoxically there may be less incentive for capable families or health planners to explore these options.
Our study is limited by the small sample size despite a 10-year window. The retrospective nature of this study cannot account for missing data nor coding deficiencies. We did not include children with hyperglycaemia who did not meet criteria for DKA but who would face the same travel-related challenges as seen in (Figure 2).
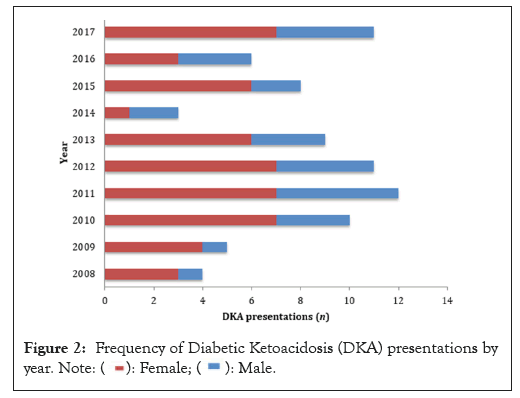
Figure 2: Frequency of Diabetic Ketoacidosis (DKA) presentations by
year. Note: 
Further work to capture service utilization, perceptions of service delivery and the financial implications resulting from challenges accessing care would shed more light on the topic. Incorporating these additional dimensions of research into the analysis of pediatric DKA presentations would enrich our understanding of the complex factors influencing healthcare access and utilization in underserved communities. By addressing not only the clinical aspects of DKA management but also the broader social, economic and perceptual factors shaping the healthcare experience, we can develop more holistic approaches to improving outcomes for pediatric patients with DKA and their families.
External specialist care remains necessary to support acute emergencies but establishing locally accessible specialist paediatric diabetes services may lessen the additional burden of distance and travel in improve long-term outcomes. Our study sheds light on the challenges faced by families of children with Diabetic Ketoacidosis (DKA) in our catchment area, particularly concerning access to specialized pediatric diabetes services. Despite an estimated population of at least 40 children under 10 years of age with type 1 Diabetes Mellitus (DM) in our area, the absence of specialized pediatric diabetes services in local non-specialist hospitals like Blacktown or Mount Druitt Hospital poses significant obstacles to timely and comprehensive care.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Lee YH, Teo SSS, Hng TM (2024) Children with Diabetic Ketoacidosis in Western Sydney: Too Close or Too Far? Clin Pediatr. 09:266.
Received: 29-Apr-2024, Manuscript No. CPOA-24-31285; Editor assigned: 01-May-2024, Pre QC No. CPOA-24-31285 (PQ); Reviewed: 15-May-2024, QC No. CPOA-24-31285; Revised: 22-May-2024, Manuscript No. CPOA-24-31285 (R); Published: 29-May-2024 , DOI: 10.35248/2572-0775.24.09.266
Copyright: © 2024 Lee YH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.