
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2024)Volume 14, Issue 2
Objective: This study aimed to investigate the diagnosis, treatment, and selection of second-stage urethral reconstruction methods for necrotizing fasciitis and urethral defects in the scrotal region.
Methods: A retrospective analysis was conducted of a case of necrotizing fasciitis and urethral defects in the scrotal region treated by the author. The clinical and pathological characteristics, treatment process, surgical methods, outcomes of second-stage urethral reconstruction, and relevant literature were summarized.
Results: A patient with necrotizing fasciitis and urethral defects in the scrotal region underwent bladder diversion, surgical debridement, vacuum-sealing drainage, and wound closure. Four weeks after the wound healed, the patient was discharged for recuperation. Six months later, scrotal urethral reconstruction was performed using a circular penile skin flap graft to repair the 12 cm urethral defect. The urethral catheter was removed after three weeks, resulting in unobstructed urination and satisfactory recovery.
Conclusion: Clinical cases of necrotizing fasciitis and complete urethral defects in the scrotal region are rare. In the first stage, diverting urine flow and completely removing necrotic tissue while controlling the infection are crucial. After wound healing, the selection of an appropriate method for second-stage urethral reconstruction can achieve favorable outcomes.
Necrotizing fasciitis; Urethral defects; Urethral reconstruction
Necrotizing Fasciitis (NF) is a complex acute infectious disease characterized by invasion of the superficial and deep fasciae, as well as the skin and subcutaneous tissue. It was first reported in 1883 by Fournier as severe genital necrosis known as idiopathic scrotal necrosis [1], which commonly occurs in young individuals. In 1952, Wilson coined the term "necrotising fasciitis" to describe similar diseases occurring in other parts of the body. This condition can be triggered by immunodeficiency, long-term use of glucocorticoids, poorly controlled diabetes leading to wound and perineal infections [2]. Patients typically present with signs of sepsis such as chills, high fever, or hypotension. It is more frequently observed in adults, particularly in the abdominal and perineal regions, and can lead to serious complications and sequelae, resulting in death in severe cases. The simultaneous occurrence of scrotal NF and complete destruction of the scrotal urethra is rare, but is mostly seen in severe cases of scrotal NF. The treatment of scrotal NF is challenging, and urethral reconstruction in the scrotal region presents an even more daunting and difficult challenge. This article describes the diagnostic and therapeutic processes of a clinical case of scrotal NF combined with complete destruction of the scrotal urethra. Successful urethral reconstruction was achieved using a well-designed approach to restore normal voiding function in the patient. Several feasible treatment options for urethral reconstruction following urethral damage caused by scrotal NF have been summarized based on literature review and personal experience.
A 58-year-old male patient presented with a chief complaint of difficulty urinating for one week and scrotal swelling for two days. The patient had been experiencing difficulty urinating, decreased urine output, and lower abdominal distension for the past seven days, but did not seek medical attention. Over the past two days, the patient developed scrotal and perineal swelling along with urinary difficulties, prompting him to seek medical care at a local hospital. After receiving symptomatic treatment, the patient's family was informed of the critical condition involving the possibility of multiple systemic infections, and the patient was transferred to our emergency surgery department (Figure 1). The patient had a history of poorly controlled diabetes mellitus but was otherwise in good health with no history of trauma or surgery. Physical examination revealed significant scrotal swelling with a foul odor, and areas of the scrotal skin had ruptured with purulent discharge (Figures 1A and 1B). The preliminary diagnosis indicated necrotizing fasciitis of the scrotum, septicemia, and acute urinary retention. Emergency bladder fistulization was performed after initial indwelling catheterization failed. Postoperative multidisciplinary consultation recommended further abscess drainage and urgent surgical intervention. During surgery, the lesion was found to involve the scrotal skin and fascial layer, extending to the tunica vaginalis of the testis, reaching the prepubic space near the pelvic margin, and descending to the anterior rectum. Adequate incision and drainage were performed, with extensive removal of necrotic tissue up to the tunica vaginalis of the testis. The urethra showed complete infection and necrosis, requiring excision and thorough debridement from the base of the penis to the scrotal region. The proximal bulbous urethra was closed and ligated (Figures 1C and 1D). The wound was irrigated and disinfected, and fresh tissue was observed (Figure 1E). The scrotum and wound gap were dressed and fixed with a Vacuum Sealing Drainage (VSD) dressing, ensuring no air leakage. A negative pressure drainage tube was inserted. The plan included a second-stage urethral reconstruction surgery after wound healing (Figure 1F).
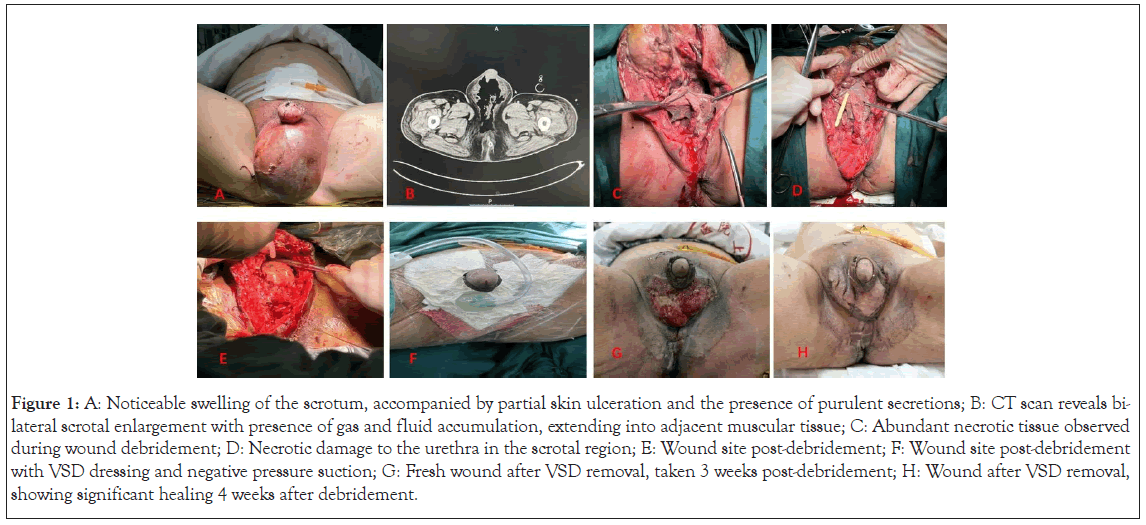
Figure 1: A: Noticeable swelling of the scrotum, accompanied by partial skin ulceration and the presence of purulent secretions; B: CT scan reveals bilateral scrotal enlargement with presence of gas and fluid accumulation, extending into adjacent muscular tissue; C: Abundant necrotic tissue observed during wound debridement; D: Necrotic damage to the urethra in the scrotal region; E: Wound site post-debridement; F: Wound site post-debridement with VSD dressing and negative pressure suction; G: Fresh wound after VSD removal, taken 3 weeks post-debridement; H: Wound after VSD removal, showing significant healing 4 weeks after debridement.
After thorough debridement and drainage, the patient was transferred to the ICU for further treatment. Antibiotics were administered postoperatively to combat infection. The patient received daily VSD negative pressure oxygen therapy for approximately 15 minutes, three times a day, along with weekly VSD replacement. After 10 days, the endotracheal tube was removed, and after 2 weeks, the patient was transferred from the ICU to a general ward. Three weeks after the operation, the VSD was removed, revealing the growth of fresh granulation tissue at the wound site (Figure 1G). Skin sutures were applied concurrently, and by the fourth week after debridement and suturing, the wound had healed (Figure 1H). The patient was discharged with a bladder fistula tube and scheduled for elective urethral reconstruction surgery.
Six months after the surgery, the patient returned for further evaluation (Figure 2). The skin in the scrotal area showed good recovery (Figure 2A). Urethral imaging indicated a defect in the scrotal segment (Figure 3A). Considering the excess foreskin tissue, pedicled preputial flap tubularization was considered for urethral reconstruction.
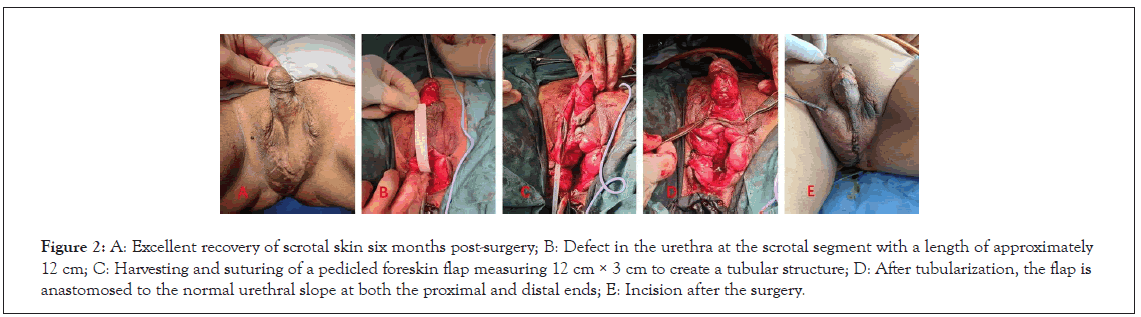
Figure 2: A: Excellent recovery of scrotal skin six months post-surgery; B: Defect in the urethra at the scrotal segment with a length of approximately 12 cm; C: Harvesting and suturing of a pedicled foreskin flap measuring 12 cm × 3 cm to create a tubular structure; D: After tubularization, the flap is anastomosed to the normal urethral slope at both the proximal and distal ends; E: Incision after the surgery.
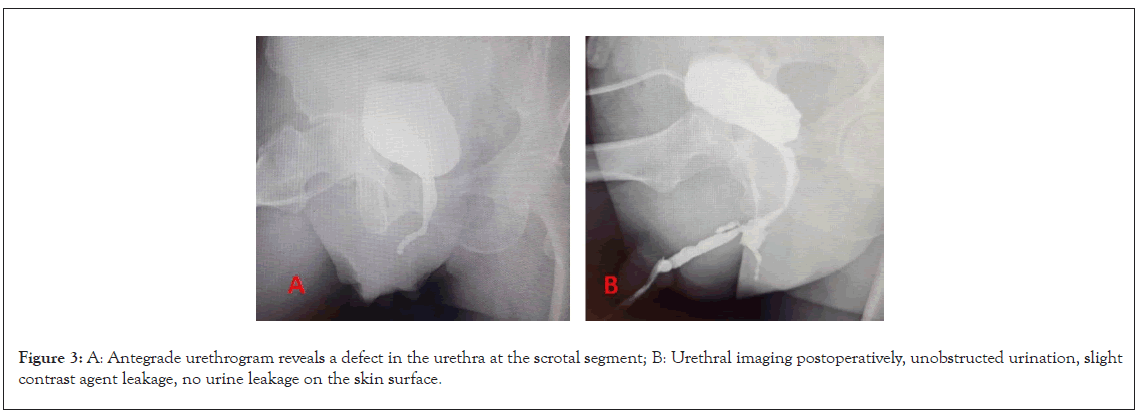
Figure 3: A: Antegrade urethrogram reveals a defect in the urethra at the scrotal segment; B: Urethral imaging postoperatively, unobstructed urination, slight contrast agent leakage, no urine leakage on the skin surface.
After thorough preoperative preparation, a perineal incision was made to expose the proximal residual urethra in the penile segment and the distal urethra in the bulbous segment. The urethral defect was approximately 12 cm in length (Figure 2B). A pedicled circular flap of the foreskin measuring approximately 12 cm in length and 3 cm in width was harvested and transferred to the site of the urethral defect in the scrotum. The catheter was wrapped around a size 18 silicone catheter and sutured to create a tubular structure. The distal end was anastomosed to the proximal residual urethra at an oblique angle, while the proximal end was anastomosed to the distal urethra in the bulbous segment. The procedure successfully reconstructed the urethra, and a size 18 silicone catheter was left in the urethral lumen. The surgery was performed without complications (Figures 2C-2E).
Three weeks postoperatively, the urinary catheter was removed, and the patient had unobstructed urination with no visible urine leakage on the skin surface. The maximum urine flow rate was 18 ml/s, and the urine volume was 136 ml. A urethral contrast study revealed minor extravasation of contrast agent at the suspected proximal anastomotic site (Figure 3B). Follow-up conducted for over six months showed no obstruction in urination and no occurrence of urinary fistula.
Necrotizing Fasciitis (NF) is a serious and rapidly spreading soft- tissue infection. Studies conducted by Kaiser et al. revealed that the mortality rate for patients with NF who undergo prompt surgical debridement is 8.3%, whereas the mortality rate increases to 75% for those who do not receive timely debridement [3]. The prognosis of elderly patients and those with concurrent medical conditions may be even poorer. The severity of the patient's condition, location of infection, and timeliness of treatment are crucial factors influencing the mortality rate.
The present case pertains to a patient with acute necrotizing fasciitis in the scrotal region accompanied by a history of diabetes and suboptimal glycemic control. The primary clinical manifestations encompass explosive and necrotizing fasciitis affecting the genital and perineal regions. The existing literature reports an overall mortality rate ranging from 7.5% to 40.0% [4,5]. This acute infection is predominantly polymicrobial in nature, with a combination of various bacteria (including streptococci, staphylococci, and anaerobic bacteria) orchestrating the disease process. The bacteria flourish and incite infection within the superficial fascia of the scrotum, rapidly disseminating in an outward fashion, thereby fostering the development of occlusive endarteritis and tissue necrosis within the subcutaneous milieu. Pathological alterations are typically limited to the scrotum, penile skin, and subcutaneous tissue, although in severe instances, involvement of the perianal and lower abdominal regions may occur. The depth of infection can extend through all layers of the scrotum; however, muscle involvement is uncommon.
For the management of this particular patient, achieving glycemic stability and expeditiously excising necrotic tissue through comprehensive debridement represent pivotal determinants for attaining success during the acute phase of treatment. This crucial intervention impedes the insidious propagation of the infection. Following meticulous debridement, it is imperative to safeguard and expose the testicles while concomitantly employing Vacuum-Sealed Drainage (VSD) to fill the scrotal cavity. This multifaceted approach fosters a propitious milieu for subsequent oxygen therapy and thwarts the growth and proliferation of anaerobic bacteria, thereby fostering the principles of wound healing and granulation. The salient peculiarity of this case resides in the far-reaching infection that encompasses not only the scrotal domain, but also the urethra at the scrotal segment, culminating in substantial destruction of a protracted segment of the scrotal urethra, thus engendering an arduous challenge for secondary urethral reconstruction.
In patients with urethral destruction resulting from necrotizing fasciitis, the selection of urethral reconstruction technique should be individualized, taking into account the patient's skin and wound conditions [6-10]. The author posits that the following approaches to urethral reconstruction are typically considered.
Permanent perineal urethrostomy
In 2022, Pedro et al. documented a case involving management of urethral destruction in the scrotal segment [11]. In this particular case, failed attempts at catheterization during the surgical intervention prompted the performance of a percutaneous suprapubic cystostomy, along with extensive penile and scrotal debridement that entailed complete penile detachment, subsequent embedding of the detached penis in the subcutaneous tissue of the upper bladder, and anterior urethrectomy, culminating in the ultimate execution of perineal urethrostomy.
For patients afflicted with severe local infection and substantial urethral necrosis, an initial recourse to suprapubic cystostomy above the pubic symphysis diverts urinary flow, thereby ushering in a favorable milieu for infection control. In contrast, perineal urethrostomy confers the distinct advantage of enabling patients to regain autonomy in urination post-recovery. However, it is significant to emphasize that this modality requires assuming a squatting position during urination, which can exert a certain degree of influence on the patient's overall quality of life.
Two-stage procedure: Percutaneous suprapubic cystostomy followed by scrotal skin flap tubed urethral reconstruction
In cases where urethral destruction is severe in the scrotal segment and the penile skin is limited, yet the scrotal skin boasts a more favorable condition, a two-stage approach is adopted. The initial stage involves performing percutaneous suprapubic cystostomy for urinary diversion. Following infection control and subsequent restoration of the scrotal skin, the second stage, known as scrotal skin flap tubed urethral reconstruction, is scheduled to take place approximately six months to one year post-initial intervention. The salient advantage of this technique lies in its astute exploitation of the local skin as the building block for urethral reconstruction, effectively obviating the need to procure additional free mucosal tissue from the oral cavity or tongue. However, it is imperative to acknowledge that this approach has certain drawbacks, the chief of which is the inherent possibility of hair follicle tissue existing within scrotal skin. Despite preoperative efforts to obliterate hair follicles, the specter of postoperative hair growth within the reconstructed urethral lumen, coupled with the advent of secondary complications, such as the formation of stones and large looms.
Three-stage procedure: Percutaneous suprapubic cystostomy, free mucosal prefabricated urethral graft, and urethral reconstruction
The first stage involves percutaneous suprapubic cystostomy, which is performed quickly to prepare for subsequent procedures. In the second stage, the surgeon faces the challenge of limited availability of proximal skin flaps. To overcome this, the surgeon skillfully utilizes oral buccal or tongue mucosa to create a prefabricated graft, which serves as a crucial component in repairing the urethral defect. The third stage begins approximately six months later and marks the culmination of the restoration process. It is important to note that this complex surgical endeavor carries its own set of risks. Obtaining sufficiently long segments of free mucosal tissue, such as bilateral buccal mucosa or tongue mucosa, presents its own challenges, requiring the surgeon to navigate the intricate oral cavity to meet the length requirements for the reparative journey. Alternatively, a combination of ipsilateral buccal mucosa and tongue mucosa can be employed, but this approach also entails potential risks. Patients with a predisposition to scarring or those who experience graft failure may encounter significant challenges during the third-stage urethral reconstruction, where the question of re-harvesting tissues becomes a vexing concern.
Two-stage procedure: Percutaneous suprapubic cystostomy followed by McAninch skin flap tubed urethral reconstruction
For patients afflicted by severe local infection, boasting a commendable penile skin condition, yet burdened by extensive scrotal skin destruction, a medical arsenal replete with options comes to the fore. Act one witnesses the major performance of percutaneous suprapubic cystostomy, an intervention that seeks to divert urinary symphony. Act two, a masterpiece conceived and perfected by the visionary urologist McAninch et al. in 1980, takes center stage, heralding the arrival of McAninch skin flap tubed urethral reconstruction [12,13]. This transformative procedure harnesses the power of a pedicled skin flap harvested from the foreskin to widen or reconstruct a constricted urethra, thereby restoring the harmonious rhythm of normal urinary function.
The patient described in this article had a favorable condition for penile foreskin reconstruction, while the scrotal segment of the urethra was completely destroyed. A meticulous plan was devised to use a pedicled skin flap with a remarkable inner preputial plate measuring approximately 3 cm in width. The penile skin was carefully retracted to expose the inner preputial region, from which a pedicled circular skin flap measuring 3 cm in width was harvested. Once unfurled, this flap stretched to an impressive length of 12 cm, meeting the demanding length requirements for urethral defect repair. The flap migrated to the scrotal region and formed a tube-like structure by wrapping itself around an absorbable suture. The proximal and distal ends of this conduit were then sutured to the normal urethra, successfully reconstructing the urethra.
The average circumference of the foreskin in healthy adults is typically 10 cm-12 cm. For individuals with a larger penile girth, the foreskin circumference may exceed these limits, making it suitable for reconstructing urethral defects in the anterior urethra. Preserving the blood supply of the skin flap is significant, requiring the expertise of a skilled urologist experienced in urethral reconstruction. The foreskin skin has superior stretchability compared to normal urethral tissue, so caution must be exercised when harvesting the flap to ensure its dimensions remain reasonable. This minimizes the risk of postoperative dilation and diverticula formation in the reconstructed urethral segment. Urethral healing typically occurs within 2-3 weeks after reconstruction. In this case, minor contrast agent extravasation was observed at the proximal anastomotic site during urethral imaging performed 3 weeks postoperatively, but no urinary leakage was detected. To prevent postoperative urinary fistula formation, the patient was instructed to engage in independent urination once daily after catheter removal, while using a bladder fistula tube to empty urine for the rest of the day. Five weeks after surgery, the bladder fistula tube was successfully removed, and the patient has since maintained normal urinary flow without fistula formation.
Necrotizing fasciitis of the scrotum is a grave, albeit relatively uncommon, infection with the potential to be life threatening. When this condition concurrently affects and devastates the urethra, treatment becomes even more intricate. It is imperative to aggressively manage the infection and preserve the patient's life while concurrently embarking on a well-thought-out design and plan to reconstruct the damaged urethra. In doing so, the aim is to optimize the restoration of normal urination function, thereby enhancing the patient's quality of life.
Author contribution
Duan Liujian: Writing-Drafting of the manuscript revising the manuscript critically for important intellectual content; Cao Jianwei: Writing-Drafting of the manuscript revising the manuscript critically for important intellectual content; Cui Xingang: Conception and design of study; Li Chao: Conception and design of study.
Acknowledgements
The study was approved by the ethics committee of Xinhua Hospital Affiliated to Shanghai Jiao Tong University, School of Medicine. The patients volunteered to sign an informed consent form. This study conformed to the provisions of the Declaration of Helsinki.
Disclosure of conflict of interest
None
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Liujian D, Jianwei C, Wei L, Lin Z, Xingang C, Chao L (2024) Choice of Urethral Reconstruction Methods Following Necrotizing Fasciitis and Urethral Defects in the Scrotal Region. J Clin Trials. 14:553.
Received: 12-Jan-2024, Manuscript No. JCTR-24-29157; Editor assigned: 15-Jan-2024, Pre QC No. JCTR-24-29157(PQ); Reviewed: 29-Jan-2024, QC No. JCTR-24-29157; Revised: 05-Feb-2024, Manuscript No. JCTR-24-29157(R); Published: 15-Feb-2024 , DOI: 10.35248/2167-0870.24.14.553
Copyright: © 2024 Liujian D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.