Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 6
Objective: To determine the Choroidal Thickness (CT) profile in healthy eyes of adult Omani population.
Methods: A cross-sectional study involving three hundred eyes of 150 volunteers (75 males, 75 females) ≥ 18 years of age. Volunteer’s age, gender, visual acuity, refractive error, and Axial Length (AL) were recorded. CT was measured at sub-foveal area and 500 microns and 1000 microns temporal, nasal, superior, and inferior from the fovea using Enhanced Depth Imaging-Optical Coherence Tomography (EDI-OCT) device.
Results: The mean age was 33.3 years (range: 21-55 years, SD ± 9.2 years), and the mean AL was 23.76 mm (SD ± 0.94 mm). CT was found thickest at the sub-foveal area (330.88 µm (SD ± 69.52 µm; 95% CI)). The second highest CT was found superiorly 500 µm away from the fovea (324.48 µm (SD ± 70.24 µm; 95% CI)). The lowest CT was 1000 µm away from the fovea nasally (301.16 µm (SD ± 70 µm; 95% CI)). A strong negative correlation was found between CT and age (p-value<0.05). There was no significant statistical difference in sub-foveal CT between males (337.61 µm, SD ± 75.64) and females (324.24 µm, SD ± 62.7) (P=0.242). No significant relationship was found between CT and AL or refractive errors.
Conclusion: Our study provides normative database of CT in healthy eyes of adult Omani population. CT depends on its location, sub-foveal being the thickest and nasally the thinnest. Establishing normative data of CT serves as a reference in the clinical settings and future researches.
Choroid; Choroidal thickness; Pachychoroid; Optical coherence tomography; Enhanced depth imaging
The highly vascular choroid lies between retina and sclera and provides nutrition to the outer one-third of retina, photoreceptor layer and retinal pigment epithelium and plays an important role in thermoregulation [1,2]. Structurally, it consists of three-caliber vessels; the inner most is the choriocapillaris which is hyper-reflective, small-sized, and affixed to retina through Bruch’s membrane. Sattler which is hypo-reflective medium-sized and located in the middle and the Haller which is hypo-reflective large-sized outer vessels and continued as lamina fusca to sclera.
The significance of quantitative measurement of Choroidal Thickness (CT) has been clearly elucidated in various chorioretinal disorders and reproducibility has efficiently been improved due to the use of advanced Optical Coherence Tomography (OCT) technology [3]. There are number of factors such as age, gender, refractive error, axial length [4,5], diurnal variation [6,7] and numerous ocular pathologies affecting the CT.
CT increases in pachychoroid [in Greek, Pachy means thick]. Chorioretinal disorders are often associated with thick choroid. Clinical spectrum of pachychoroid disorders includes pachychoroid pigment epitheliopathy, central serous chorioretinopathy, pachychoroid neovasculopathy, polypoidal choroidal vasculopathy/aneurysmal type 1 choroidal neovascularization, focal choroidal excavation, peripapillary pachychoroid syndrome in addition to Vogt-Koyanagi Harada disease [8,9]. Active choroidal tumors e.g. choroidal melanoma [10] and high hyperopia [11] also present with thick choroid. Whereas, CT decreases in high myopia associated with long axial length [12], proliferative diabetic retinopathy [13] and increasing age [14]. An estimated age-related choroidal thickness reduction is approximately 10 µ-15.6 µ for each decade of life [14,15].
The invention of non-invasive, non-contact imaging modality-the Optical Coherence Tomography (OCT) is used to acquire cross-sectional scans of the retina and measures real time CT in vivo; among all the enhanced depth imaging technique of Spectral Domain OCT (SD-OCT) and Swept Source OCT (SS OCT) have been proven to quantify the choroid accurately. These have a longer wave length and sufficient capability to visualize the choroid with good resolution [16,17].
There are several studies that have reported the normative database of CT worldwide [18-22]. However, there is no existing such database in Omani population. In addition, we have studied the CT profile at different points both vertically and horizontally from the fovea, that’s distinct from the published studies.
The purpose of conducting cross-sectional, descriptive, clinical study was to establish normative database of the Choroidal Thickness (CT) in healthy eyes of adult Omani population and to determine the correlation between sub-foveal CT and the age, gender, Axial Length (AL) and refractive status of the eyes.
Study was conducted in accordance with the tenets of the Declaration of Helsinki and an ethical approval was obtained from the institutional medical research ethical committee (MREC #1969), an informed consent was obtained from each volunteer. Those with no present or past history of ocular disorders were recruited. Exclusion criteria include high myopia (>-6D), or hyperopia (>+4D), any retinal or Retinal Pigment Epithelium (RPE) abnormalities detected on Optical Coherence Tomography (OCT) scan, poor image quality or any history of any intraocular surgery. All participants underwent AL measurement which was performed using ocular biometry (IOL Master; Carl Zeiss Meditec, Jena, Germany).
300 eyes of 150 healthy adult Omani volunteers (75 males, 75 females) ≥ 18 years of age were recruited and studied in the ophthalmology department at Sultan Qaboos University Hospital (SQUH). The study patients' age, gender, visual acuity, refractive error, and AL were recorded. CT was scanned and measured at sub-foveal area and 500 microns and 1000 microns temporal, nasal, superior, and inferior from the foveal center using Enhanced Depth Imaging-Optical Coherence Tomography (EDI-OCT) device (Heidelberg Engineering, Heidelberg, Germany). In current device the automated segmentation of the choroidal boundary’s detector is not available on the in-built software. Therefore, three trained independent readers measured the CT manually for all subjects using the OCT linear measurement tool, perpendicularly from the outer portion of the hyper-reflective line corresponding to the RPE to the inner surface of the sclera at sub-foveal area and 500 microns and 1000 microns temporal, nasal, superior, and inferior from the fovea (Figure 1). Inter-observer reproducibility and intra-observer repeatability was measured.
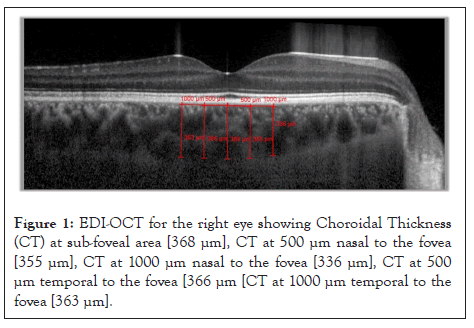
Figure 1: EDI-OCT for the right eye showing Choroidal Thickness (CT) at sub-foveal area [368 μm], CT at 500 μm nasal to the fovea [355 μm], CT at 1000 μm nasal to the fovea [336 μm], CT at 500 μm temporal to the fovea [366 μm [CT at 1000 μm temporal to the fovea [363 μm].
All data was entered in Epi-data then shifted to Statistical Package for the Social Sciences (SPSS) and analysis carried out in the IBM SPSS statistics version 26.0. For descriptive purposes, categorized variables were presented as frequency and percentage. Continuous variables were presented as mean with standard deviation and 95% confidence interval. Independent samples t- test and r-Pearson’s correlation coefficient test were used (P<0.05 considered statistically significant). Intraclass Correlation Coefficient (ICC) was obtained for the agreement among three readers.
CT was obtained for 300 eyes of 150 participants (75 males, 75 females) using EDI- OCT. The mean age of the participants was 33.3 years (range: 21-55 years, SD ± 9.2 years), and the mean axial length was 23.76 mm (SD ± 0.94 mm). CT was found to be the thickest at the sub-foveal area with a thickness of 330.88 µm (SD ± 69.52 µm; 95% CI). The second highest thickness of the choroid was found superiorly 500 µm away from the fovea (324.48 µm, SD ± 70.24 µm; 95% CI). The lowest CT was located nasally 1000 µm away from the fovea with a mean of 301.160 (SD ± 70 µm; 95% CI) (Table 1 and Figure 2). A strong negative correlation was found between CT and age at most of the measured sites (p-value<0.05) (Table 2). There was no significant statistical difference in the sub-foveal CT between males (337.61, SD ± 75.64) and females (324.24 µm, SD ± 62.7) in this study (p-value=0.242) (Table 3). No significant relationship was found between CT and the axial length or refractive errors. However, CT tends to be thicker in emmetropic and hyperopic eyes compared to myopic eyes. Finally, ICC showed very strong agreement between the three readers (ICC>0.90 for all the measurements) (Table 4).
| Measured points of choroidal thickness | Mean | Standard deviation |
|---|---|---|
| Sub-foveal area | 330.8 | 65.5 |
| 500 µm superior to the fovea | 324.4 | 70.2 |
| 500 µm inferior to the fovea | 323.1 | 70 |
| 1000 µm superior to the fovea | 321 | 69.5 |
| 1000 µm inferior to the fovea | 319.6 | 68.5 |
| 500 µm nasal to the fovea | 313.9 | 70 |
| 500 µm temporal to the fovea | 316.5 | 68.2 |
| 1000 µm nasal to the fovea | 303 | 70.1 |
| 1000 µm temporal to the fovea | 307.6 | 65.8 |
Table 1: Mean and Standard Deviation (SD) of choroidal thickness (µm) at different sites for 300 eyes.
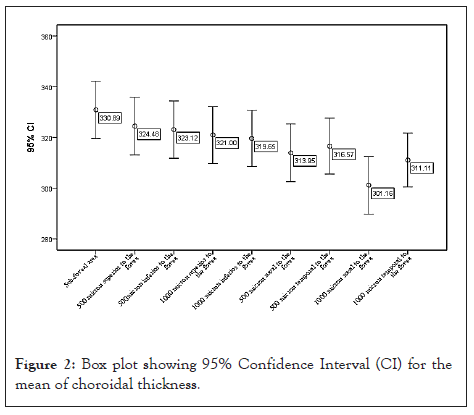
Figure 2: Box plot showing 95% Confidence Interval (CI) for the mean of choroidal thickness.
| Variable | Age | Sub-foveal area | 500 micron superior to the fovea | 500 micron inferior to the fovea | 1000 micron superior to the fovea | 1000 micron inferior to the fovea | 500 micron nasal to the fovea | 500 micron temporal to the fovea | 1000 micron nasal to the fovea | 1000 micron temporal to the fovea | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | r | 1 | -0.233** | -0.197* | -0.213** | -0.181* | -0.207* | -0.211** | -0.244** | -0.211** | -0.190* |
| P-value | 0.006 | 0.016 | 0.009 | 0.028 | 0.011 | 0.010 | 0.003 | 0.010 | 0.020 | ||
| N | 150 | 149 | 149 | 149 | 149 | 149 | 149 | 149 | 149 | 149 | |
Note: r: Pearson's correlation coefficient; **: Correlation is significant at the 0.01 level (2-tailed); *Correlation is significant at the 0.05 level (2-tailed)
Table 2: R-Pearson's correlation coefficient showing strong negative correlation between CT and age (P<0.05).
| Characteristics | Gender | Mean | Std. Deviation | P-value |
|---|---|---|---|---|
| Sub-foveal area | Male | 337.6194 | 75.64929 | 0.242 |
| Female | 324.2422 | 62.70053 | ||
| 500 µm superior to the fovea | Male | 330.8311 | 77.51099 | 0.275 |
| Female | 318.2156 | 62.1347 | ||
| 500 µm inferior to the fovea | Male | 330.1441 | 62.1347 | 0.226 |
| Female | 316.1933 | 62.1347 | ||
| 1000 µm superior to the fovea | Male | 328.0068 | 77.34039 | 0.224 |
| Female | 314.0911 | 60.64194 | ||
| 1000 µm inferior to the fovea | Male | 326.9279 | 74.8418 | 0.199 |
| Female | 312.4622 | 61.28302 | ||
| 500 µm nasal to the fovea | Male | 321.9212 | 76.14561 | 0.168 |
| Female | 306.0844 | 62.92586 | ||
| 500 µm temporal to the fovea | Male | 324.1126 | 72.05926 | 0.181 |
| Female | 309.1356 | 63.86027 | ||
| 1000 µm nasal to the fovea | Male | 308.9707 | 75.53245 | 0.178 |
| Female | 293.4578 | 63.99372 | ||
| 1000 µm temporal to the fovea | Male | 319.6757 | 70.45977 | 0.115 |
| Female | 302.6578 | 60.21323 |
Table 3: Relationship between mean choroidal thickness and gender showing no statistically significant difference in the mean CT between males and females at all measured points (Independent samples t-test) P>0.05.
| Measured points of choroidal thickness | Intraclass Correlation Coefficient (ICC) [right eye] | Intraclass Correlation Coefficient (ICC) [left eye] |
|---|---|---|
| Sub-foveal area | 0.968 | 0.970 |
| 500 µm superior to the fovea | 0.950 | 0.962 |
| 500 µm inferior to the fovea | 0.959 | 0.964 |
| 1000 µm superior to the fovea | 0.952 | 0.947 |
| 1000 µm inferior to the fovea | 0.961 | 0.960 |
| 500 µm nasal to the fovea | 0.964 | 0.963 |
| 500 µm temporal to the fovea | 0.966 | 0.966 |
| 1000 µm nasal to the fovea | 0.963 | 0.963 |
| 1000 µm temporal to the fovea | 0.925 | 0.952 |
Table 4: Intraclass Correlation Coefficient (ICC) showing a very strong agreement between the readers (ICC>0.90 for all the measurements).
There are different consensus regarding to normal Choroidal Thickness (CT) and no single absolute normal value of CT is documented. However, it is well explored that the choroid is thickest at sub-foveal area, sequentially thinner extrafoveal temporally and thinnest nasally [14]. The high oxygen demand at the fovea is proposed for choroid to be thickest at sub-foveal zone [19].
Some clinical trials report sub-foveal CT varies between 220 to 350 µ and ≥ 390 µ considered as thick choroid [23]. Cheung et al. mention that many researchers consider sub-foveal CT >300 µm as pathological [24]. Chhablani et al. described normal sub-foveal CT ranges from 191 ± 74.2 micron to 354 ± 111 micron [25].
In our study, we determined the choroid thickest at the sub-foveal area with a thickness of 330.88 µm (SD ± 69.52 µm; 95% CI). The second highest thickness of the choroid was found superiorly 500 µm away from the fovea (324.48 µm, SD ± 70.24 µm) and lowest CT was located nasally 1000 µm away from fovea with mean of 301.160 (SD ± 70 µm) and this sequence of thickness order from greater to lesser, sub foveal, superior and nasal respectively correlates as with published literature.
In the Iranian population, Heirani et al. utilized the same EDI-OCT and detected the mean sub-foveal CT was 329.83 ± 70.33 µm without significant difference in gender and interestingly, their results are closer to our study. In our study, there was no statistically significant difference in sub-foveal CT between males (337.61, SD ± 75.64) and females (324.24 µm, SD ± 62.7). Similarly, some other researchers did not reveal statistically significant difference in the choroidal thickness between genders, whereas studies from other regions showed significant difference in males and females. Zeng et al. detected higher mean SFCT in males (298.02 ± 101.47) µm than in females (256.28 ± 90.87) µm (P<0.05) [26]. Wang et al. mentioned the choroid is thicker in males with mean difference of 19.5 µm for foveal CT and 14.7 µm for average CT [27].
Rahman et al. reported the mean sub-foveal CT in healthy subjects was 332 µm that is also very similar to our study [28]. Bhayana et al. showed the mean sub-foveal CT was 299.10 ± 131.2 µ in Indians’ population that is lower CT than our study results [20].
Some Asian studies detected normal choroidal thickness much lower and not consistent with our results, such as in China; Wei et al. reported mean sub-foveal CT was 253.8 ± 107.4 µm [29], while Ding et al. observed an average sub-foveal CT was 261.93 ± 88.42 µm. In one Korean study, Kim et al. showed the mean sub-foveal CT was 279.5 ± 99.5 µm in normal eyes [30]. Whereas Ikuno et al. found mean sub-foveal CT was 354 ± 111 µm (range, 80 µm-641 µm) in Japanese population [31] that is comparatively higher CT than our findings. Abdellatif compared the CT among different age groups and he showed mean central CT (337.23 ± 37.51 µm) in young to middle aged Egyptian population. Their results are fairly near to results of our recruited participants of mean young to middle aged 33.3 SD ± 9.2 years.
Our study showed mean sub-foveal CT values higher than many of studies reported previously in the literature [25-28], while there are other studies showing an even higher CT than our obtained results. Lehmann et al. suggested considering sub-foveal CT of 395 µm as upper normal limit.
Many studies exhibit inverse correlation of choroidal thickness with Axial Length (AL) and refractive errors [32], but we did not find significant relationship of CT with AL and refractive errors. This was most probably due to our strict inclusion criteria focused at healthy eyes and excluding high refractive error as well as long eyes from our study because our primary aim was to determine the normative data in healthy eyes of adult Omani population.
Nagasawa et al. found significantly thicker choroid in children and younger compared to adults and old aged, Fujiwara et al. also explored that sub foveal choroidal thickness in younger than 10 years was significantly thicker than in other age groups [7,33]. Majority of our study volunteers were younger to middle aged of mean 33.3 SD ± 9.2 years with good CT, supports the trend of strong correlation of CT and age; younger the age higher the CT.
The comprehensive review of literature evidences the wide variation of normal CT among different regions and population is attributed to distinct ethnicity, case selection of different age group and variable refractive status. Moreover, Rahman et al. commented the inter-observer variability also affects the CT. The utilization of this particular model of OCT and manual measurement technique may limit the measurement of choroidal thickness due to an unclear posterior boundary at choroid-scleral junction. Matsuo et al. reported that the choroid measured with Swept Source (SS) OCT was thicker than that measured with SD-OCT instruments thus, the choroidal thickness should not be compared between the SD-OCT and SS-OCT instruments [34].
While, Yamashita et al. in Japanese population, measured the sub foveal choroidal thickness by using three different SD-OCTs: Heidelberg Spectralis-OCT, Cirrus HD-OCT and Topcon 3D OCT-1000 Mark II and reported that measurements with three different OCTs are highly correlated and could be used interchangeably [35].
However, available literature does not provide adequate evidence to compare the obtained results of choroidal thickness confidently between various OCT manufacturers. Our study provides normative database of CT in healthy adult Omani population. CT depends on its location, sub-foveal being the thickest and nasal being the thinnest. Establishing normative database of CT serves as a reference in the clinical settings and for future researches evaluating choroidal changes in different chorioretinal conditions. Finally, including a broader range of participants, particularly the pediatric age group, may add more meaningful results.
We would like to thank the following colleagues: Mr. Harith Al-Hasani, Optometrist, department of ophthalmology, Sultan Qaboos University Hospital for assisting in the recruitment of the volunteers; Ms. Sadika Al-Ajmi, Ophthalmic technician, department of ophthalmology, Sultan Qaboos University Hospital for assisting in performing the diagnostic tests; Mr. Sachin Jose Statistics Specialist, Research Section, Oman Specialty Board for assisting in data analysis.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Al-Abri M, Al-Aliyani A, Mal W, Holla A, Al-Rawahi A, Al-Marhoon M, et al. (2022) Choroidal Thickness Profile in Healthy Eyes of Adult Omani Population: A Cross-Sectional, Descriptive Clinical Study. J Clin Exp Ophthalmol. 13:935.
Received: 04-Nov-2022, Manuscript No. JCEO-22-19894; Editor assigned: 07-Nov-2022, Pre QC No. JCEO-22-19894 (PQ); Reviewed: 21-Nov-2022, QC No. JCEO-22-19894; Revised: 28-Nov-2022, Manuscript No. JCEO-22-19894 (R); Published: 05-Dec-2022 , DOI: 10.35248/2155-9570.22.13.935
Copyright: © 2022 Al-Abri M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.