
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Case Report - (2023)Volume 13, Issue 2
Pityriasis lichenoides is a benign inflammatory disease of unknown etiology. There are two types of this condition: An acute form and a chronic one both are more common in children and young adults. Here, we describe a case of Pityriasis Lichenoides Chronica (PLC).
Dermatologists have been leaders in the field of cosmetic surgery. Some dermatologists complete fellowships in surgical dermatology. Many are trained in their residency on the use of botulinum toxin, fillers, and laser surgery. Some dermatologists perform cosmetic procedures including liposuction, blepharoplasty, and face lifts. Most dermatologists limit their cosmetic practice to minimally invasive procedures. Despite an absence of formal guidelines from the American board of dermatology, many cosmetic fellowships are offered in both surgery and laser medicine.
Pityriasis lichenoides; Cyclins; Dermotology; Cosmetics
Pityriasis lichenoid is a rare dermatosis of unknown cause in young people. There are 2 clinical forms: Acute varioliform lichenoid pityriasis characterized by a papular rash evolving to necrosis and chronic lichenoid pityriasis resulting in a papulosquamous rash that may persist for months or years [1]. Different treatments have been proposed.
We report a new observation of PLC in an adolescent.
A 21 years old patient consulted for a disseminated rash evolving by successive outbreaks for 2 years. It consisted of erythematous papules, polymorphous, covered with greyish scales for some, ulcero-necrotic for others. There were leukomelanodermal scarring lesions. Palms and soles were respected. Scalp and facial involvement was noted. The rash was asymptomatic. The patient was apyretic and in good general condition.
The cutaneous histological examination was in favour of a PL in its chronic form by showing a parakeratotic hyperkeratosis, an acanthosis with lymphocytic exocytosis (Figure 1).
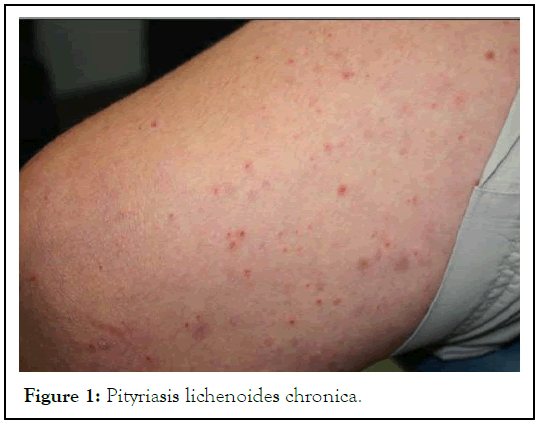
Figure 1: Pityriasis lichenoides chronica.
A treatment with dermocorticoids was started without improvement in the patient. One month later cyclines were introduced at 200 mg/kg per day. The clinical improvement was notable with an almost complete disappearance of the specific lesions in three months.
Pityriasis lichenoid is a spectrum of inflammatory dermatoses that includes a chronic and an acute form with several intermediate forms. Clinically, chronic lichenoid pityriasis manifests itself as an eruption of papulo-squamous elements evolving by flare-ups and remissions during several months. Necrotic lesions evolving to varioliform scarring are seen in the acute form. The pathophysiology is unknown. The diagnosis is based on the clinical picture as well as on the histological image and immune histochemical study. The main differential diagnosis is lymphomatoid papulosis due to clinical and sometimes histological similarities [2]. Several therapeutic modalities are available but large randomized studies are still lacking. First-line treatment is based on a course of antibiotics, mainly cyclins, in combination with dermocorticoids or topical tacrolimus. PUVA therapy or ultraviolet B phototherapy are proposed as second-line treatment [3,4]. Oral corticosteroid therapy and methotrexate are reserved for severe and recurrent forms.
PLC tends to have little, round, dim pink, flaky injuries. The scaling spots level out north of a little while, leaving earthy coloured staining, what blurs gradually more than a while, like PLEVA, PLC might keep going for a long time.
PLEVA sores are bothersome, crusted (scabbed) red knocks or rankles, which recuperate to leave little scars. It looks basically the same as chicken pox. PLEVA may likewise cause mouth ulcers. Most frequently, the injuries happen on the storage compartment, thighs and upper arms, yet may show up anyplace on the body. It might keep going for a really long time or even quite a while, with yields of new injuries seeming like clockwork. The conclusion might should be affirmed by a skin biopsy.
Pityriasis lichenoides" is a term used to allude to a gathering of uncommon, obtained, fiery skin problems that incorporates Pityriasis Lichenoides Chronica (PLC), Pityriasis Lichenoides Et Varioliformis Acuta (PLEVA), and the Febrile Ulceronecrotic Mucha-Habermann Disease (FUMHD) variation of PLEVA. The utilization of the expression "pityriasis lichenoides" to allude to each of the three problems is illustrative of the hypothesis that PLC, PLEVA, and FUMHD might address a clinical range of a solitary sickness.
A skin condition, otherwise called cutaneous condition, is any ailment that influences the integumentary framework the organ framework that encases the body and incorporates skin, nails, and related muscle and glands. The significant capability of this framework is as a hindrance against the outside environment [5].
States of the human integumentary framework comprise an expansive range of sicknesses, otherwise called dermatoses, as well as numerous nonpathologic states like, in specific conditions, melanonychia and racquet nails). While just few skin illnesses represent most visits to the doctor, a huge number of skin conditions have been described. Order of these circumstances frequently presents numerous nosological challenges, since fundamental causes and pathogenetics are frequently not known. Hence, latest reading material present a characterization in light of area (for instance, states of the mucous layer), morphology (constant rankling conditions), cause (skin conditions coming about because of actual variables, etc.
PLC is clinically described by the improvement of various layered, erythematous to brown papules on the storage compartment and furthest points (picture 1A-1C). The condition as a rule has a backsliding and dispatching course that endures for months or years.
The clinical indications, conclusion, and the board of PLC will be evaluated here. PLEVA and FUMHD are examined independently. (See "Pityriasis Lichenoides Et Varioliformis Acuta" (PLEVA)).
Authoritative ends on the study of disease transmission of Pityriasis Lichenoides Chronica (PLC) are obstructed by the regular absence of qualification between the subtypes of pityriasis lichenoides in the distributed writing and restricted information. As a general rule, PLC is viewed as an uncommon problem that is probably going to happen in youthful grown-ups and kids. Notwithstanding, PLC might create at whatever stage in life [6].
The presence of sex, ethnic, or racial preferences in PLC is dubious. In view of information from a couple of review investigations of kids with pityriasis lichenoides, there might be a slight male preference for pityriasis lichenoides in the pediatric populace. In one of the biggest series of kids with PLC (n=46), 59 percent of the youngsters were male.
LPC is a rare inflammatory dermatosis. An anatomic-clinical confrontation is essential to make the diagnosis. The diagnosis should be suspected in any papulo-squamous dermatosis. PL poses essentially a problem of diagnosis and therapeutic management. First-line treatment is based on a course of antibiotics, mainly cyclins.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ammar N, Daakir H, Senouci K (2023) Chronic Lichenoid Pityriasis: A Case Report. J Clin Trials. 13:526.
Received: 09-Nov-2022, Manuscript No. JCTR-22-20013; Editor assigned: 11-Nov-2022, Pre QC No. JCTR-22-20013 (PQ); Reviewed: 25-Nov-2022, QC No. JCTR-22-20013; Revised: 13-Feb-2023, Manuscript No. JCTR-22-20013 (R); Published: 20-Feb-2023 , DOI: 10.35248/2167-0870.23.13.526
Copyright: © 2023 Ammar N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.