Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2020)Volume 10, Issue 7
Introduction: Falling oestrogen levels in the perimenopause alter the function of dopamine, melatonin and neuropeptides, and therefore affect thermoregulation, vasomotor stability, mood regulation, quality of sleep and psychological wellbeing. When Hormone Replacement Therapy (HRT) is not appropriate, taking food supplements can be useful. A new food supplement for the menopause (ESP), which contains soy isoflavones, Magnolia and Agnus castus extracts, acts on the vasomotor and psycho affective symptoms and has shown interesting preliminary clinical results. This study, with a controlled design, confirms the clinical activity of ESP in symptomatic postmenopausal women.
Method: Menopausal women with more than five moderate hot flushes a day and with changes in mood or sleep were enrolled in a randomised, controlled, parallel-group, multicentre study. Women on active treatment for climacteric symptoms were excluded. Eligible women were assigned to three months ’ oral treatment with one tablet/day of ESP (Estromineral Serena Plus, Meda Pharma, Mylan Group), containing soy isoflavones (SI), Lactobacillus sporogenes (Ls), extracts of Vitex agnus-castus and Magnolia officinalis, vitamin D3 and calcium, or with E (Estromineral, Meda Pharma, Mylan Group), containing SI, Ls, vitamin D3 and calcium. At baseline and after one, two and three months, we evaluated the Kupper man Index (KI) score and symptoms present, and any adverse reactions were recorded. At the end of the study, the physicians expressed their clinical judgement and the women self-evaluated their treatment.
Results: Across 68 centres, 588 women were treated, 354 with ESP and 234 with E. They had a mean age of 53.0 years and had been menopausal for 2.8 years, and 32% had used HRT in the past. KI score, hot flushes, night sweats, palpitations, loss of libido, vaginal dryness, dyspareunia, insomnia, irritability, anxiety and sexual activity improved to asignificantly greater extent with ESP than with E (p<0.01). During the study, five cases (one withdrawal) in the E group and three cases (one withdrawal) in the ESP group experienced adverse events possibly related to the treatment.
Conclusion: The results confirm the synergistic effect of the nutraceutical combination Agnus castus, soy isoflavones and magnolia extract on vasomotor and psycho behavioural symptoms in postmenopausal women, with excellent compliance and safety.
Menopause; Menopausal symptoms; Hot flushes; Thermoregulation; Isoflavones; Chaste tree berry; Magnolia; Plant extracts
The menopause has characteristic vasomotor symptoms, often accompanied by psychological symptoms, which cause the worsening quality of life as a direct consequence of oestrogen deficiency. The endocrinological aspects of the menopause have yet to be fully clarified. It is known that oestrogen hormones usually modify the synthesis, release and metabolism of many neurotransmitters such as dopamine, melatonin and neuropeptides, including β-endorphins, which modulate the hypothalamic and limbic systems and particularly dopaminergic activity. The gradual fall in oestrogen levels that starts in the perimenopause, therefore, changes the function of these systems andconsequently affects thermoregulation, vasomotor stability, mood regulation and psychological wellbeing, explaining the most common symptoms of the menopause [1-25].
In postmenopausal women, dopamine activity is significantly reduced, and stimulating D2 receptors is effective at relieving hot flushes and reducing the psychological symptoms that go alongside them. In addition, it has been observed that sleep quality is associated with the quantity of melatonin secreted, which significantly decreases as age increases. Hormone Replacement Therapy (HRT), which should only be prescribed for moderate or severe symptoms according to international guidelines, has a limited scope because of genuine contraindications or plain refusal by women, even when they do have symptoms that would justify its use.
A new food supplement has been developed for the menopause, based on natural active ingredients. The effects of Soy Isoflavones (SI) on vasomotor symptoms and of magnolia on psycho affective symptoms-particularly anxiety, irritability and insomnia-have been potentiated by the addition of Agnus castus (chaste tree berry), which acts both on hot flushes and on psychological symptoms. This formulation Estromineral Serena Plus (ESP) also contains Lactobacillus sporogenes (Ls) to ensure that the soy isoflavones are absorbed, and vitamin D3, calcium and magnesium to strengthen bone mineralisation, especially where decalcification and/or osteoporosis are also present. ESP has shown promising clinical activity and optimal safety in postmenopausal women in a preliminary open-label, an uncontrolled study [2]. The aim of this research was to evaluate the efficacy of ESP in a controlled study versus another SI-and Ls-based food supplement for symptomatic postmenopausal women [3].
The experimental design chosen was a randomised, controlled, prospective, parallel-group, multicentre study coordinated by Professor Vincenzo De Leo of the Molecular Medicine and Development Department, Obstetrics and Gynecology Division at the University of Siena in Italy. The study was approved by the Local Ethics Committee for Clinical Research on Medicines at Siena University Hospital, Italy, and was conducted in accordance with the recommendations of the 1964 Declaration of Helsinki and its revisions up to 2013. Subjects gave their written informed consent and could leave the study at any time, without having to provide a reason. Each subject was given a letter addressed to her general practitioner, to inform the GP of the content of the study and to ensure greater compliance with the study procedures.
The inclusion criteria were menopausal women (clinically diagnosed based on the absence of menstrual periods for at least 12 months) with moderate typical symptoms of the menopause, namely more than five hot flushes a day with concomitant changes in mood or sleep that were not severe enough to require specific psychopharmacological treatment. The exclusion criteria were concomitant use of HRT or other pharmacological or nonpharmacological treatments that could interfere with the symptoms being studied. Each doctor taking part in the research had to treat at least ten women deemed eligible for the study, who were randomly and evenly assigned to one of the two treatments using a centre-specific randomisation list. The oral treatments to be compared were: ESP (Estromineral Serena Plus, Meda Pharma, Mylan Group), containing extract of Vitex agnuscastus 40 mg, SI 60 mg, Ls 109 spores, extract of Magnolia officinalis 50 mg, vitamin D3 5 μg and calcium 141 mg and E (Estromineral, Meda Pharma, Mylan Group), containing SI 60 mg, Ls 109 spores, vitamin D3 5 μg and calcium phosphate dihydrate 137 mg. Both were taken at the dose of one tablet/day for three months. The treatment could be continued beyond the planned duration of the study on a spontaneous basis, recording the clinical evaluations.
At baseline and after one, two and three months, we evaluated the presence and severity of hot flushes, night sweats, insomnia, irritability, depressed mood (melancholia), dizziness, fatigue, joint and muscle pain, headaches, palpitations and paraesthesia using the Kupperman Index (KI), as well as vaginal dryness, pain on sexual intercourse, anxiety, problems concentrating and loss of libido. Doctors could extend the treatment period to six months, recording the results in the appropriate Case Report Form (CRF). At the end of the study, the doctors provided their overall clinical judgement of the treatment, while the women self-evaluated the acceptability and perceived benefit of therapy (scale: 0=none, 1=modest, 2=fair, 3=good, 4=excellent) and the quality of their sexual activity (improved, unchanged or worse).
The sample size was calculated using the SISA method (Simple Interactive Statistical Analysis) [4].
Reduction in the Kupper man Index was the primary endpoint. Based on data from the literature, we hypothesized a reduction in KI score of 70% with ESP and 50% with the alternative treatment, giving an α of 0.05 (double-sided) and a power of 1 β=0.8 with a sample size of 105 subjects per treatment group (approximate number of cases necessary because both percentages are significant with a 5% probability level). Effect size and statistical power were calculated on the absolute differences in KI score from 0 to 3 months between the two treatments. Any adverse effects could be recorded in the CRF, specifying the severity, duration, time of resolution, relationship to treatment and measures taken as a result of the event.
Baseline homogeneity between the two groups was checked using Student ’ s t-test and the x2 test with Yates ’ correction applied where appropriate.
Statistical analysis of clinical efficacy was performed by comparing changes from baseline in the two treatment groups at various predetermined times, using all the data available at each time point, with a factor analysis of variance and, where appropriate, the x2 test.
All the data available at each time point were included in the analysis so that the sample size was maximised each time and no information was lost. The significance level was considered to be α=0.05 (type I error) and the power to be β=0.90 (type II error).
Across 68 centers, 588 women were treated, 354 with ESP and 234 with E.
They had a mean age (± standard deviation) of 53.0 ± 3.6 years, BMI of 25.7 ± 4.2 kg/m2, and had been menopausal for 2.8 years; 32% of them had used HRT in the past (Figure 1 and Table 1).
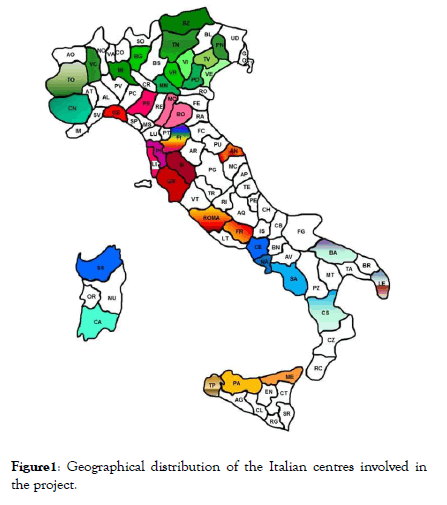
Figure 1: Geographical distribution of the Italian centres involved in the project.
| ESP | E | p | |
|---|---|---|---|
| Number | 354 | 234 | 588 |
| Age (years) | 52.4 ± 4.3 | 52.4 ± 4.5 | NS |
| Weight (kg) | 66.8 ± 2.6 | 67.0 ± 1.7 | NS |
| BMI (kg/m2) | 25.5 ± 1.8 | 24.9 ± 1.3 | NS |
| Menopause-spontaneous | 89.70% | 91.70% | NS |
| In menopause since (years) | 3.1 ± 3.4 | 2.8 ± 2.9 | NS |
| Previous use of HRT (%) | 16.8 | 13.1 | NS (x2 2 × 2 correzione di Yates) |
| Familiarity (%) | 28.4 | 25.5 | NS (x2 2 × 2 correzione di Yates) |
| Physical activity (%) | 38.4 | 33.8 | NS |
| Alcohol consumption (%) | 33.5 | 33.8 | NS |
| Smoking (%) | 16.5 | 22.9 | NS (x2 2 × 3) |
| Ex-smoker (%) | 17.6 | 14.3 | NS |
Table 1: Comparison of group characteristics at baseline (total no=588).
Based on the data reported in individual CRFs, the mean effective time (± SD) of monitoring visits was calculated as 32.4 ± 7.4 days (T1), 63.6 ± 10.5 days (T2), 97.8 ± 15.4 days (T3) and 213.3 ± 65.7 days (T6).
Checking for baseline homogeneity of clinical parameters between the two groups showed a higher KI score and more severe night sweats, insomnia, loss of libido and vaginal dryness in the ESP group vs E one Table 2.
| ESP | n | E | n | p | |
|---|---|---|---|---|---|
| IK | 26.54 ± 0.45 | 354 | 23.80 ± 0.55 | 234 | p<0.01 |
| Flushing | 2.35 ± 0.04 | 341 | 2.22 ± 0.05 | 224 | NS |
| Sweating | 2.16 ± 0.04 | 333 | 1.97 ± 0.05 | 215 | p<0.01 |
| Insomnia | 2.16 ± 0.04 | 316 | 1.92 ± 0.05 | 207 | p<0.01 |
| Irritability | 1.99 ± 0.05 | 306 | 1.88 ± 0.05 | 188 | NS |
| Anxiety | 1.89 ± 0.05 | 261 | 1.78 ± 0.06 | 171 | NS |
| Libido loss | 2.07± 0.04 | 294 | 1.91 ± 0.05 | 200 | p<0.01 |
| Vaginal dryness | 2.08 ± 0.05 | 289 | 1.88 ± 0.05 | 192 | p<0.01 |
| Dyspareunia | 1.97 ± 0.05 | 265 | 1.85 ± 0.06 | 177 | NS |
Table 2: Homogeneity check of clinical conditions between-group sat baseline (mean ± and SE).
The KI score, and particularly the severity of hot flushes, night sweats, palpitations, loss of libido, vaginal dryness, pain on sexual intercourse, insomnia, irritability and anxiety, decreased significantly (p<0.01) during treatment with either ESP or E versus baseline and the previous time point.
A significantly greater reduction (p<0.01) was observed with ESP than with E (Figures 2-4). At T2, the KI score was already below the threshold of 15.
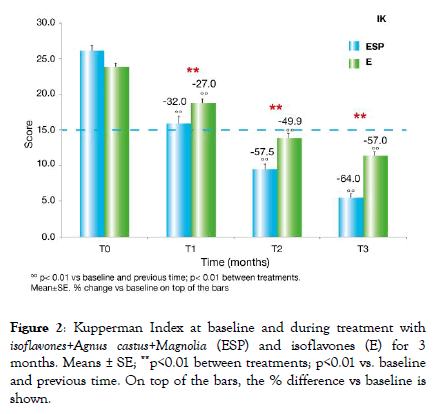
Figure 2: Index at baseline and during treatment with isoflavones+Agnus castus+Magnolia (ESP) and isoflavones (E) for 3 months. Means ± SE; **p<0.01 between treatments; p<0.01 vs. baseline and previous time. On top of the bars, the % difference vs baseline is shown.
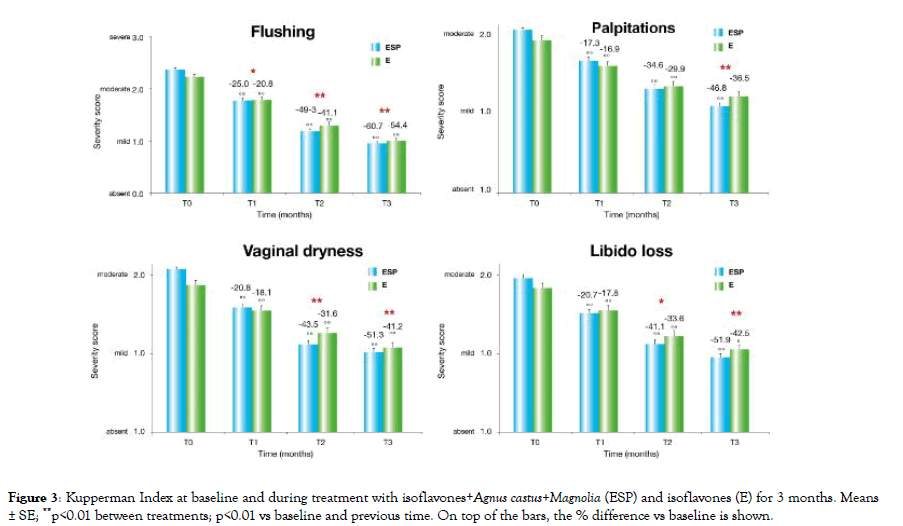
Figure 3: Kupperman Index at baseline and during treatment with isoflavones+Agnus castus+Magnolia (ESP) and isoflavones (E) for 3 months. Means ± SE; **p<0.01 between treatments; p<0.01 vs baseline and previous time. On top of the bars, the % difference vs baseline is shown.
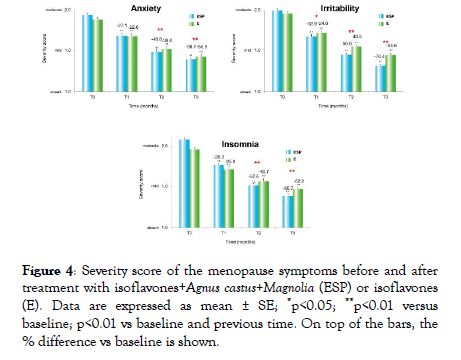
Figure 4: Severity score of the menopause symptoms before and after treatment with isoflavones+Agnus castus+Magnolia (ESP) or isoflavones (E). Data are expressed as mean ± SE; *p<0.05; **p<0.01 versus baseline; p<0.01 vs baseline and previous time. On top of the bars, the % difference vs baseline is shown.
ESP demonstrated a>60% reduction in KI score and the severity of hot flushes, insomnia and irritability.
More structural parameters such as vaginal dryness, dyspareunia and loss of libido saw a reduction of about 50%. In a minority of cases, the treatment continued until T6, and the following changes favouring ESP over E were confirmed: -72.0% vs -59.5% (p<0.01) for KI score, -71.4% vs-62.4% (p<0.05) for hot flushes, -41.9% vs-59.8% (p<0.05) for anxiety, -87.8% vs-60.3% (p<0.01) for irritability, and -76.7% vs-62.1% (p<0.01) for insomnia.
At the end of treatment, sexual activity was improved in 66.5% of subjects treated with ESP versus 51.4% of those treated with E (p<0.01 between treatments on the X2 2 × 3 test); perceived wellbeing was good or excellent in 64.1% versus 41.9% of cases (p<0.01 between treatments on the X2 2 × 2); the physician’s judgment of treatment was good or excellent in 71.5% versus 47.1% of cases (p<0.01); and acceptability to the patient was good or excellent in 72.9% versus 51.8% of cases (p<0.01).
The effect size for the primary endpoint (KI score) is 0.52, considered to be a medium effect size, with a statistical power of 90% for double-sided two-sample analysis.
During the study, five cases (one withdrawal) in the E group and three cases (one withdrawal) in the ESP group experienced adverse events judged by the investigator as having a possible relationship with the treatment.
The details reported (severity, onset time and duration) were as follows: flatulence (1 moderate, 7 days, 2 hours), constipation (1 severe, withdrawal), and blood loss (mild, 35 days, 2 days) on ESP; abdominal cramps (1 mild, 7 days, 2 hours), abdominal bloating (2 mild, 7 days, 20 days), itching (1 mild, 45 days, 3 days), and breast tenderness (1 severe, 1 month, withdrawal) on E.
Herbal medicines play a very important role in alleviating the symptoms that affect postmenopausal women. This controlled study confirms the preliminary efficacy and safety data-obtained under open-label, uncontrolled conditions–for the combination of soy isoflavones, agnus castus and magnolia. Although this research had a population with a higher KI score, its data are consistent with those from a randomised study comparing Vitex agnus-castus and placebo in menopausal women with an average of six hot flushes a day, which found a significant reduction in the daily frequency of hot flushes (p=0.015) and KI score versus placebo after two weeks of treatment (p=0.0001) [5]. Agnus castus acted in synergy with soy isoflavones and extract of magnolia on the KI score and vasomotor and psycho behavioural symptoms, with no negative interference on efficacy and safety, for an appropriate duration of treatment.
The superiority of ESP at controlling insomnia symptoms is explained by the anxiolytic activities of magnolia extract and Agnus castus, which increase the secretion of melatonin. The results can be extrapolated to the national population of Italy because they were collected from patients homogeneously distributed across the country. The effect size, which measures the difference between the means in comparison to the dispersion, was medium, indicating that the calculated sample size is adequate.
The limitations of the study are the lack of confirmation of the menopause with hormone values; the baseline non-homogeneity which disadvantaged ESP; the non-double-blind experimental design; and the low number of cases for evaluation at six months. However, the menopause was identified as per usual clinical practice; the baseline difference disadvantaging ESP makes its superiority over the control treatment even more significant, and the absence of double-blinding is partially minimized by the high number of final cases [6,7].
The menopause is undoubtedly a very vulnerable time in terms of symptoms because the low hormone levels cause neuroendocrine changes, forming the pathophysiological basis for autonomic dysfunction. As is now well known, conventional HRT is used by only a very small percentage of women, after a distorting media campaign that followed the publication of some data on the risk of breast cancer with HRT [8].
Among the alternative and complementary therapies aimed at postmenopausal women, soy isoflavones have a growing body of research and clinical documentation that support their activity in reducing vasomotor symptoms [9]. The positive effects of soy isoflavones on preventing osteoporosis are controversial and it is useful to combine them with calcium and vitamin D to strengthen this purpose [10].
The efficacy of ESP on moderate menopausal symptoms is explained by the presence in the formulation of magnolia and agnus castus extracts, which have their own beneficial properties and are indicated in postmenopausal women. Extract of Vitex agnus-castus, titrated as agnuside, its active ingredient, helps to alleviate symptoms of the menopause, particularly hot flushes and is also prescribed to treat Premenstrual Syndrome (PMS) in women of childbearing age [11-13]. There is, in fact, a similarity between this syndrome and menopausal symptoms: women who experienced PMS when they were younger get more severe autonomic dysfunction in the menopause [14,15]. The dopamine activation of Agnus castus, which probably occurs by acting on endorphins, plays an important role in alleviating hot flushes and improving the emotional symptoms of the menopause because reduced dopamine system activity is associated with psychological symptoms [16]. In addition, the binding affinity of Agnus castus for and oestrogen receptors and the increased dopaminergic tone in the hypothalamus balance the secretion of sex hormones and inhibit the secretion of prolactin [17]. Dopamine is the main neurotransmitter that controls secretion of prolactin by inhibiting it. There are clear data demonstrating that menopausal symptoms improve through an increase in dopaminergic tone with a reduction in prolactin levels, and this supports the rationale for combining phytoestrogens and Agnus castus to convincingly resolve vasomotor symptoms in postmenopausal women.
The hot flushes experienced by many menopausal women originate in the brain, and there are two regions involved: the brainstem, which plays a role in temperature regulation, and the insula, which is important in the perception of one ’ s own sensations. A Functional Magnetic Resonance Imaging (FMRI) study in postmenopausal women, who reported at least six hot flushes a day, showed that activity in the brainstem begins to increase before the start of the flush itself, whereas activity in the insula only increases after the flush has occurred [18]. The action of agnus castus on the hypothalamic thermoregulatory centre is therefore important.
Through its active ingredients, magnolol and honokiol, an extract of magnolia increase the body’s resistance and capacity to adapt to stress; its modulating activity on GABA-A receptors in the brain ’ s limbic system is responsible for its anxiolytic, antidepressant and mood regulation properties, which are very useful in postmenopausal women [19,20]. In the postmenopausal period, the extract of magnolia in combination with soy isoflavones has been shown to be effective on psychoaffective symptoms such as irritability, anxiety, and sleep disturbance, also helping to relieve concomitant vasomotor symptoms, versus a functional placebo and an active control [21,22].
Weight gain is also a clinical condition that affects many postmenopausal women, and it seems to be related to the higher prevalence of cases of anxiety, which manifests as a greater sense of hunger with a predilection for simple sugars and carbohydrates. This link between anxiety and increased appetite leads to weight gain with predominantly abdominal adipose tissue, partly in relation to oestrogen deficiency. Therefore, it is very useful to manage anxiety with natural remedies that have no risk of addiction.
Finally, no significant side effects have been reported for any of these ingredients, and there is optimal compliance from women, who feel that taking natural products will not negatively affect their body or increase their risk of breast cancer [23]. The Select Committee on GRAS (Generally Recognized As Safe) Food Substances reports that there is no evidence in the available information on soy isoflavones that demonstrates, or suggests reasonable grounds to suspect, a hazard to the public when they are used at levels that are now current or might reasonably be expected in the future. A systematic review of the side effects of Vitex agnus-castus describes it as a safe herbal medicine with no drug interactions and mainly gastrointestinal adverse effects. In addition, no changes have been observed in levels of oestradiol, follicle-stimulating hormone, liver enzymes or thyroidstimulating hormone. The therapeutic safety of ESP on breast density, endometrial thickness and liver function has been widely documented in specific studies, as has the absence of pharmacokinetic interaction with thyroid hormone replacement therapy [24,25].
Based on these activity and safety considerations, ESP, nutraceutical product combining phytoestrogens with extracts of agnus castus and magnolia could be especially useful, not only for resolving vasomotor symptoms but also to counter the neuroendocrine changes that are the main cause of anxiety, hot flushes and insomnia.
ESTRONET STUDY GROUP
Abbondanza M, Turin; Babich B, Bolzano; Cagnacci A, Modena; Cardinali l, Perugia; Cazzaniga M, Milan; Chionna R, Milan; Corsaro F, Vercelli; Costanzo M, Aprilia (RM); Di Mario M, Lodi; Faraci C, Modena; Gangemi D, Pavia; Gostinicchi P, Rome; Interlandi Raffaele, Pavia; Lupo A, Siracusa; Mainini G, Naples; Missionario O, Bologna; Monti M, Rome; Moroncini Clarice, Ancona; Nuovo R, Barletta Andria-Trani (BT); Panetta M, Matera; Pasquali A, Rome; Pietrobattista P, Rome; Rossi S, Rome; Sanfelici C, Turin; Santilli C, Pescara; Sperti L, Lecce; Viggiano F, Aversa (CE); Volpini G, Rome; Votano S, Rome; Waldis F, Milan.
Citation: Leo VD, Benvenuti C (2020) Clinical Activity of a Combination of Isoflavones, Agnus Castus and Magnolia in the Menopause: A Controlled Study on Estromineral Serena Plus. Gynecol Obstet (Sunnyvale)10:528. doi: 10.35248/2161-10932.2020.10.528
Received: 11-Jul-2020 Accepted: 18-Jul-2020 Published: 27-Jul-2020 , DOI: 10.35248/2161-10932.20.10.528
Copyright: © 2020 Leo VD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.