Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2024)Volume 9, Issue 4
Objective: To explore the etiology, age, diagnosis, treatment and prognosis of facioplegia.
Methods: A retrospective etiology and epidemiological survey of 757 patients with facioplegia admitted to the People's hospital of Shaanxi Province from January 2015 to October 2017 was conducted to analyze their clinical features.
Results: The primary incidence was the highest, accounting for 40% of the total incidence rate, the highest incidence of 19-60 years old, accounting for 48% of the total morbidity, the highest incidence of retirees, accounting for 43% of the total incidence rate, 11% of patients cured at discharge, 83% improved.
Conclusion: The etiology of facial paralysis is complicated; the incidence rate of adults is higher than that of children. The incidence rate of 41-60 years old is the highest and the hospitalization days are mostly 8-14 days. For patients with facioplegia, early diagnosis, timely and reasonable treatment, most of the prognosis is good.
Facioplegia; Treatment; Etiology; Diagnosis; Total incidence rate
Facioplegia, also known as facial paralysis, is mainly characterized by facial expression muscle group dyskinesia, clinical manifestations include oblique mouth and eye, mouth angle drooping of the affected side after shutting up, closing eyes, raising eyebrows, bulging gills, baring teeth cannot be completed, is a common clinical disease can occur all year round and in any age group. It is most common in adults and more male than female. Its etiology is complex, also still unknown and this disease often due to buccal facial feelings of cold or wind and heat after the attack. The onset is rapid, mostly are delayed paralysis of one side muscle. Taking effective treatment measures in time is very beneficial to the recovery and prognosis of the disease. Since January 2015 to October 2017, 757 patients with facioplegia have been hospitalized in our hospital. The overall rate of complete recovery was 97.6% with significantly faster recovery in younger children and in patients with NB as compared to idiopathic facial palsy.
Both patients with incomplete recovery were at least 14 years old and presented late in the course of the disease [1].
General information
From January 2015 to October 2017, 757 patients with facioplegia who were hospitalized and discharged from our hospital according to the International Classification Code of Diseases ICD-10 were analyzed retrospectively. Among them, there were 427 males (56%) and 330 females (44%). Age: From 6 months 14 days to 96 years old, including 13 cases (1.7%) ≤ 3 years old, 6 cases (0.7%) between 3-7 years old, 9 cases (1.2%) between 7-18 years old, 124 cases (16%) between 18-40 years old, 242 cases (32%) between 40-60 years old, 161 cases (21%) between 60-70 years old, 202 cases (27%) ≥ 70 years old.
The course of hospitalization was 1-49 days, most of which were 8-14 days. There were 578 cases (76%) from urban areas, 179 cases (24%) from rural areas. Occupation: 328 had retired, accounting for 43.3%,98 were in-service cadres, accounting for 12.9%, 96 cases (12.7%) were farmers, 71 cases (9.4%) were workers, 21 cases (2.8%) were students, 19 cases (2.5%) were individual household, 7 cases (0.9%) were medical staff, 3 cases (0.4%) were IT workers and 15.1% for other 114 cases [2].
Classification
280 cases were primary, accounting for 40%, 62 cases of facial neuritis, accounting for 8.2%, 33 cases with herpes zoster, accounting for 4%, 27 cases with pulmonary disease, accounting for 3.4%, 20 cases with diabetes, accounting for 2.6%, 19 cases with hypertension, accounting for 2.5%. There were 7 cases of fracture, 6 cases of brain injury and 1 case of Kawasaki disease [3].
Visiting department
There were 482 cases in neurology department, 63 cases in otorhinolaryngology, 29 cases in hepatocardiovascular department, 25 cases in digestive department, 25 cases in emergency department, 23 cases in rehabilitation department, 21 cases in endocrine department, 19 cases in pediatrics, 19 cases in oncology department, 17 cases in traditional Chinese medicine department, 16 cases in internal medicine, 13 cases in orthopedic department, 12 cases in neurosurgery, 11 cases in ophthalmology, 11 cases in other 11 cases, 6 cases in general surgery, 4 cases in respiratory and urology, 4 cases in hematology department, 3 cases in thoracic surgery, 3 cases in obstetrics and gynecology department. There were 2 cases in department of kidney, 1 case in anorectal surgery and 1 case in renal transplantation [4].
Primary disease
342 cases of simple facioplegia, 33 cases of herpes zoster, 107 cases of cerebral infarction, 27 cases of pulmonary disease, 19 cases of hypertension, 20 cases of diabetes, 7 cases of fracture, 6 cases of craniocerebral injury and 1 case of Kawasaki disease.
Outcome
87 cases (11%) were cured, 627 cases (83%) were improved, the total effective rate was 93%, 5 cases (1%) were uncured, 1 case died and 37 other cases, accounting for 4% [5].
Length of stay
There were 23 cases in 1-3 days, 169 cases in 4-7 days, 452 cases in 8-14 days, 110 cases in 14-30 days and 8 cases longer than 30 days (Figures 1-3).
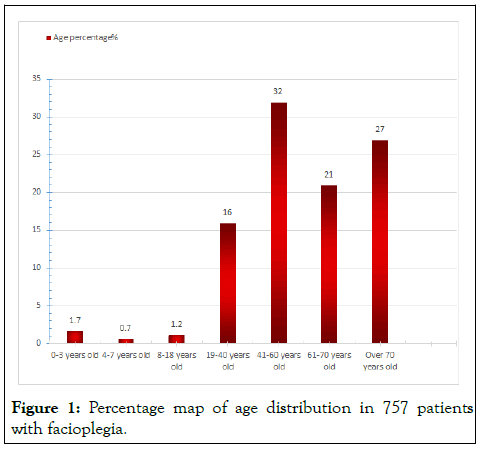
Figure 1: Percentage map of age distribution in 757 patients with facioplegia.
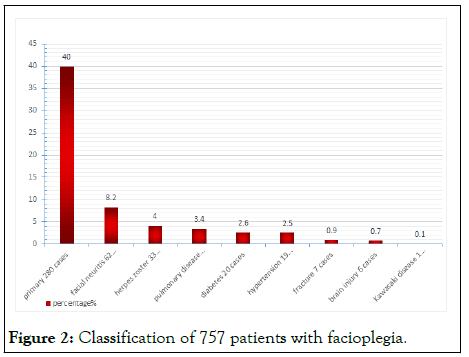
Figure 2: Classification of 757 patients with facioplegia.
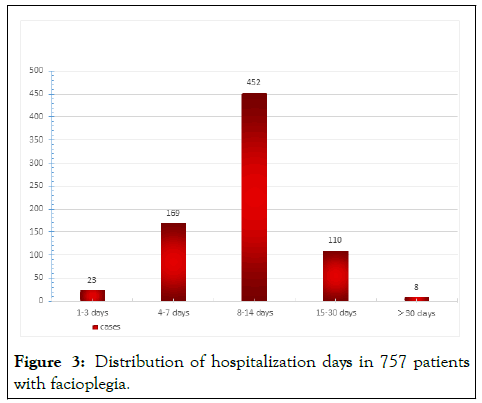
Figure 3: Distribution of hospitalization days in 757 patients with facioplegia.
Facial paralysis has been more common in recent years, caused by a variety of causes, clinically based on the areas of injury are divided into two categories, peripheral facial neuritis and central facial neuritis. Central facial neuritis is a lesion in the cortical medullary tract from the facial nucleus to the cerebral cortex, mostly caused by cerebrovascular disease, intracranial tumor, brain trauma, inflammation, etc; peripheral facial neuritis lesions appear in the facial nerve and facial nerve nucleus. The main cause is excessive contraction of local blood vessels, muscle spasm, leading to local tissue circulation, leading to diseases caused by ischemia [6].
Causes of peripheral facial neuritis: Acute facial nerve palsy in children may be caused by infection by Borrelia burgdorferi, but the incidence of facial nerve palsy and the proportion of facial nerve palsy caused by Lyme borreliosis may vary considerably between areas. Furthermore, it is not well known how often facial nerve palsy caused by Lyme borreliosis is associated with meningitis. In this population-based study, children admitted for acute facial nerve palsy to Stavanger University Hospital during 9 years from 1996 to 2004 were investigated by a standard protocol including a lumbar puncture. A total of 115 children with facial nerve palsy were included, giving an annual incidence of 21 per 100,000 children. 75 (65%) of these were diagnosed as Lyme borreliosis, with all cases occurring from May to November. Lymphocytic meningitis was present in all but 1 of the children with facial nerve palsy caused by Lyme borreliosis where a lumbar puncture was performed (n=73). In this endemic area for Borrelia burgdorferi, acute facial nerve palsy in children was common. The majority of cases were caused by Lyme borreliosis and nearly all of these were associated with lymphocytic meningitis.
• Otogenic diseases, such as otitis media
• Infectious diseases, caused by latent sensory activation of the
facial nerve
• Tumors
• Autoimmune reactions
• Traumatic
• Neurogenic
• Poisoning such as drugs or long-term exposure to poison
• Vascular insufficiency
• Metabolic disorders, such as diabetes, vitamin deficiency
• Congenital facial nucleus hypoplasia
In the past, the term "Beibei" was equivalent to "primary facial paralysis", which was the paralysis of primary low-level facial neurons. 27 consecutive cases with acute peripheral facial palsy were studied for Lyme borreliosis. In 16 out of 27 children Lyme borreliosis could be diagnosed by detection of specific IgM antibodies in CSF. CSF findings allow a clear distinction according to etiology [7]. All children with facial palsy due to Lyme borreliosis revealed lymphocytic CSF pleocytosis, whereas in cases of unknown etiology CSF was usually normal. Bilateral facial palsy occurred only in children with Lyme borreliosis. The diagnosis should be ruled out for other possible causes. While David put forward the hypothesis of herpes simplex virus, some studies have validated this hypothesis at serological levels. The facial nerve is a mixed nerve, which contains exercise, sensation, taste and autonomic nerve fibers. In addition to the hemifacial spasm, the patient may be accompanied by corneal reflex disappearance, tear secretion disorder and the taste may disappear [8]. The main pathological changes are facial nerve edema and there are different degrees of degenerative edema in the nerve sheath or axon, especially in the inner part of the neural tube of the stem surface. In any instance of facial paralysis in a child, an effort should be made to determine immediately whether it is caused by a specific, treatable entity. Of 61 cases of facial paralysis in children seen in a facial paralysis clinic, 38% were not Bell's palsy. Eight of the 61 children had disease amenable to specific therapy available today. Experience with 504 patients of all age groups seen within 4 years has led the authors to abandon facial nerve decompression in the treatment of Bell's palsy. Corticosteroids and antivirals given within 10 days of onset have been shown to help (Tables 1-3) [9].
| Part | Performance | Score | Part | Performance | Score |
|---|---|---|---|---|---|
| The frontal line | Normal | 0 | Normal | 0 | |
| Becomes shallower and shorter | 1 | Nasolabial fold | Becomes shallower and shorter | 1 | |
| Completely disappeared | 2 | Disappeared | 2 | ||
| Eyelids | Upper eyelids drooping | 3 | People middle ditch | Normal | 0 |
| Lower eyelids valgus | 2 | Gully to the healthy side | 2 | ||
| Eye crack | Normal | 0 | Mouth | Normal | 0 |
| Increase | 2 | Mouth shape to the healthy side | 1 | ||
| Normal | 0 | Suture of the affected side | 2 | ||
| Nostril | Deformation | 2 | Lip groove | Normal | 0 |
| Nasal collapse | 3 | Lighter | 2 |
Table 1: Facial nerve scoring system-static view score table (compared with the healthy side in static view).
| Complications | Performance | Score |
|---|---|---|
| Joint movement | When the eye of the affected side is closed, the affected side is connected with the angle | 1 |
| Eye of the affected side is involuntarily closed when the tooth is shown | 2 | |
| Involuntary contraction of the frontal muscle in the affected side of the eye | 3 | |
| Facial muscle contracture | Reduction of ocular fissure on the affected side | 3 |
| The nasolabial fold of the affected side is too deep or too long | 2 | |
| Oral ruminant to the affected side | 3 | |
| Facial muscle twitching | Only orbicularis muscle twitching | 1 |
| Facial expression muscle twitching | 2 | |
| Facial expression and neck dermatosus twitching | 3 | |
| Crocodile tears | Tears when eating thick food | 2 |
| Tears when eating light food | 3 |
Table 2: Facial nerve scoring system-complication score table.
| Status | 5 Points | 7 Points | 8 Points | 10 Points |
|---|---|---|---|---|
| Lift amount | No movement | Slight movement | Obvious movement, but the length of the frontal depth is lower than the healthy side | Normal movement, the depth of the forehead is the same as the number of the healthy side |
| Close eyes | Cannot be closed, the eye crack is equivalent to 1/2 of the eye | Cannot be completely closed, the eye crack is equivalent to 1/3 of the eye | Can be closed, but the eyelashes are positive and the eye cannot be opened while closing the affected side of the eye | Can be completely closed and the eyelashes are negative and can open the eye in the consensus of the affected side of the eye |
| Drumstick | When the drum is rubbed on both sides, it is impossible to swell | When the drum is double-sided, the sputum can bulge, but the intensity is small | The affected side can be swelled independently, but the intensity is slightly worse than the healthy side | The affected side can be independently swelled and the magnitude of the force is equal to the healthy side |
| Dry nose | No movement of the nose | Only slight movement of the nose | The nose has obvious movement, but the intensity is stronger than the healthy side | The nose has obvious movement and the strength is equal to the healthy side |
| Moving mouth | There is no movement in the affected side of the mouth. When the teeth are displayed, the upper and lower teeth of the affected side are not exposed. When the mouth is opened, the oblique eggs are round and round | There is slight movement in the mouth, but the range of strength is poor. When the teeth are displayed, the affected side is exposed and asymmetrical and the mouth is marked with a slanting egg mark | There is movement in the mouth, but the amplitude is slightly worse. When the teeth are displayed, the number of upper and lower teeth exposed on the affected side is basically symmetrical, but the mouth is thirsty and slanted oval and the mouth is slanted and/or the upper and lower lips are asymmetrical | The amplitude of the movement of the mouth is normal and the degree of exposure of the upper and lower teeth on the affected side is symmetrical. The mouth of the mouth is ovate, the sulcus is not slanted and the upper and lower lips of the affected side are symmetric |
Table 3: Facial nerve scoring system-dynamic view score table (compared with affected side in dynamic view).
Among the 757 cases in our hospital, the incidence rate of adults is higher than that of children. Adults account for about 96%, children only account for 3.6%, 41-60 years old have the highest incidence rate, accounting for 32% of the total incidence and simple facial paralysis is the most, accounting for 40%, and there is a case of Kawasaki disease with facial nerve paralysis. The majority of hospital days are 8-14 days and the cure rate is 87% [10].
Treatment
• Dexamethasone and mannitol intravenous drip can reduce
inflammation, dehydration, anti-exudation, eliminate nerve
edema, reduce nerve compression and avoid further nerve
damage.
• Compound danshen injection and dibazole can improve
blood circulation. Vitamin B1, vitamin B12 nutrition nerve.
• Facial acupuncture, moxibustion and infrared local irradiation
can effectively improve the cure rate of facial nerve paralysis,
with remarkable curative effect and good recovery [11].
Precautionary measures
• Avoid electric fans, air conditioners and strong winds. In the
cold weather, you can tap or tap on the face, neck and some
acupuncture points behind the ear to enhance your body's
ability to keep out the cold.
• The optimistic and peaceful attitude of daily life treats life and
work and reduces stress. Avoid being under high pressure.
• Strengthen exercise and enhance your physical fitness.
• Eat more fruits and vegetables, and enhance the body's ability
to resist disease [12].
The study highlights the importance of early diagnosis and appropriate treatment in facioplegia. Bell's palsy remains the most common etiology, with a high rate of recovery when treated promptly. Multimodal treatment approaches, including medication, physical therapy and in some cases, surgeries are essential for optimal outcomes. Facioplegia can result from a variety of causes, including Bell's palsy, trauma, infections and tumors. Understanding the distribution of these causes and the effectiveness of different treatments can help improve patient management and outcomes.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Jiao F, Li X, Wang L, Gu T, Zhang M, Liu J, et al. (2024) Clinical Analysis of 757 Cases of Facioplegia. Clin Pediatr. 09:274.
Received: 17-Feb-2020, Manuscript No. CPOA-24-3395; Editor assigned: 20-Feb-2020, Pre QC No. CPOA-24-3395 (PQ); Reviewed: 05-Mar-2020, QC No. CPOA-24-3395; Revised: 22-May-2024, Manuscript No. CPOA-24-3395 (R); Published: 19-Jul-2024 , DOI: 10.35248/2572-0775.24.09.274
Copyright: © 2024 Jiao F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.