Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2024)Volume 9, Issue 6
Objective: To analyze the clinical efficacy of "Siming Acupoints" massage technique in the treatment of myopia in children and adolescents and to explore the related factors influencing the therapeutic effect.
Methods: From January 2021 to January 2024, 257 cases of children and adolescents with true myopia and 475 eyes treated and followed up at the pediatric massage center of shandong hospital of traditional chinese medicine were included in this study. The clinical efficacy was analysed by comparing the observation indicators before and after the intervention. The occurrence of ineffective treatment was observed and the related factors of ineffective treatment were explored by using univariate comparison and multivariate logistic regression analysis.
Results: Clinical efficacy shows the effective rate of 257 children and 475 eyes was 93.05% the effective rate of 374 eyes in the low myopia group was 98.13% the effective rate of 76 eyes in the moderate myopia group was 81.58% the effective rate of 25 eyes in the high myopia group was 52.00%. The score of visual fatigue symptoms after the intervention was significantly lower than that before the intervention (p<0.001) the naked eye vision after the intervention was significantly higher than that before the intervention (p<0.001) NRA and PRA after the intervention were significantly enhanced compared with NRA and PRA before the intervention (all p<0.001). Risk factor analysis of ineffectiveness shows that there were 33 eyes in the ineffective group and 442 eyes in the effective group. The proportion of patients with a history of sweet tooth in the ineffective group was significantly higher than that in the effective group (p=0.020) the course of disease in the ineffective group was significantly longer than that in the effective group (p=0.001) and there were also significant differences in the degree of myopia between the two groups, with the proportion of high myopia in the ineffective group significantly higher than that in the effective group (p<0.001) the spherical equivalent, equivalent spherical power and cylindrical power in the ineffective group were all significantly higher than those in the effective group (all p<0.001) the axial length of the eye in the ineffective group was significantly longer than that in the effective group (p=0.005) the naked eye vision before treatment and the corrected naked eye vision at the first treatment in the ineffective group were both worse than those in the effective group (both p<0.001) the proportion of patients with outdoor activities <2 h/day and the proportion of patients with night sleep time <7 h/day in the ineffective group were significantly higher than those in the effective group (p=0.022, p=0.012). Binary multivariate logistic regression showed that combined outdoor activities <2 h/day (OR=8.270, p<0.001), equivalent spherical power (OR=2.724, p=0.005) and night sleep time <7 h/day (OR=2.507, p=0.014) were the risk factors for ineffective treatment of true myopia in children and adolescents with "Siming Acupoints" massage technique. The ROC curve showed that the area under the curve for outdoor activities <2 h/day was 0.603 the area under the curve for equivalent spherical power was 0.678 the area under the curve for night sleep time <7 h/day was 0.667.
Conclusion: The "Siming Acupoints" massage technique may be able to improve the naked eye vision of patients, improve NRA, PRA and visual fatigue symptoms and control the growth of axial length and equivalent spherical power. Outdoor activities <2 h/day, equivalent spherical power and night sleep time are the risk factors for ineffective treatment of myopia in children and adolescents with "Siming Point" massage technique.
Siming acupoints massage; Childhood and adolescent myopia; Clinical effect; Multi-factor correlation analysis
Myopia is the most common refractive disorder globally, which not only leads to a significant decline in vision but also constitutes a potential risk factor for other serious ocular diseases [1]. It is estimated that 1.4 billion people suffered from myopia in 2000 and this number is projected to reach 4.8 billion by 2050, among which the proportion of high myopia patients is as high as 10% [2,3]. From a socio-economic perspective, refractive errors, particularly uncorrected ones, can impact academic performance, restrict employability and lower the quality of life. Myopia is associated with multiple ocular complications, such as retinal detachment, glaucoma, cataract, optic disc alterations and macular disorders, etc [4]. Recent studies have revealed that 80% of school graduates in China have visual impairments and the myopic population in China is equivalent to the combined populations of the United States and Japan [5]. With the continuous increase in the number of myopic patients, the treatment and prevention of myopia have become key issues that urgently need to be addressed [6].
The "Siming Acupoints" massage technique has achieved remarkable results in the treatment of myopia in children and adolescents. Numerous published studies have demonstrated that this technique shows favorable therapeutic effects in improving the naked eye vision of children with myopia, delaying the development of diopter and the growth of the eye axis, etc. [7,8]. However, previous studies have been relatively limited, the clinical therapeutic effect analysis has been incomplete and the limitations of this technique have not been analyzed. Therefore, the aim of our present study is to further analyze its clinical therapeutic effect in detail, clarify the limitations of this technique and the risk factors affecting the therapeutic effect of the technique and provide more accurate theoretical support for clinical treatment.
General information
A retrospective analysis was conducted on the clinical therapeutic effects of 257 children and adolescents with myopia (475 eyes) who were treated at the pediatric tuina center of shandong provincial hospital of traditional chinese medicine from January 1,2021 to January 1,2024 and received follow-up for half a year (the treatment was performed by experienced practitioners of the same seniority). The patients were divided into an ineffective group of 33 eyes and an effective group of 442 eyes and the risk factors for ineffectiveness were analyzed. During or after data collection, authors were able to obtain information that could identify individual participants. All participants signed informed consent forms.
Inclusion criteria
• The routine eye examinations of the children met the diagnostic criteria of myopia in both Chinese and Western medicine.
• The follow-up time for the children was half a year. The guardians and the children signed the informed consent form.
• The age of the children was 3 to 12 years old.
Exclusion criteria
• Children with inflammation in the eyes, skin lesions on the face, or infectious foci.
• Patients with severe systemic diseases, such as those in the heart, cerebrovascular, liver, kidney, hematopoietic system and mental disorders.
• Those who adopted other treatment methods during the treatment period or did not complete the treatment course.
• Those with pathological myopic fundus changes and/or obvious visual impairment or other concurrent eye diseases that affected the determination of therapeutic effects.
The qualitative and quantitative diagnoses were made according to the definitions and classifications of myopia formulated in the white paper on myopia prevention and control research established by the International Myopia Institute (IMI) founded by the World Health Organization (WHO) and the classification of myopia in the "theory and methods of optometry" textbook of the "13th five-year plan" of the national health and family planning commission of china [9].
Qualitative: After using cycloplegic agents to examine the refractive power, if the myopia degree disappears and becomes emmetropia or hyperopia, it is considered pseudomyopia, if the myopia refractive degree does not decrease or the decrease is <0.50 D after using cycloplegic agents, it is considered myopia, if the myopia refractive degree significantly decreases (≥ 0.50 D) but does not return to emmetropia after using cycloplegic agents, it is considered mixed myopia.
Quantitative: When the eye is relaxed, if the equivalent spherical power of the eye ≥ 0.50 D, it is considered myopia; when the eye is relaxed, if the equivalent spherical power of the eye ≥ 0.50 D and <-3.00 D, it is considered low myopia; if the equivalent spherical power ≥ 3.00 D and <6.00 D, it is considered moderate myopia; if the equivalent spherical power ≥ 6.00 D, it is considered high myopia; the equivalent spherical power=spherical power +1/2 cylindrical power.
Treatment method
The patients were given pediatric tuina mainly on the "Siming Acupoints.
• Open the heavenly gate, push the palace of Kan, mobilize the Taiyang (EX-HN5) and knead the posterior auricular eminence (GB12) 24 times each.
• Press and knead the Jingming (BL1), Shangming (EX-HN19), Yiming (EX-HN13) and Guangming (GB37) acupoints for 2 minutes each; knead the Cuanzhu (BL2), Yuyao (EX-HN4), Sibai (ST2), Sizhukong (TE23), and Chengqi (ST1) for a total of 2 min.
• Scrape the upper and lower eye sockets and pinch the double eyebrow arches (from the beginning to the end of the eyebrows) 5 times each push around the eye sockets with the one-finger meditation variant peak for 2 min, iron the eyes 5 times.
• The child assumes a prone position for the back operation. Roll along the bladder meridians on both sides of the back for 2 min.
• The child sits for the head and neck operation. Press and knead the Taiwei (ST8), Qucha (BL4), Baihui (GV20), Sishencong (EX-HN1), Fengchi (GB20) and Dazhui (GV14) acupoints for a total of 2 min grasp the five meridians 5 times, sweep and disperse both temporal regions for 1 min, knead the neck and nape region for 1 min; grasp the Jianjing (GB21) with both hands 5 times to conclude the operation. The treatment was given every other day, 3 times a week, with 6 times as one course. After 4 consecutive courses of intervention, the intervention was given once a week for half a year.
Observation indicators
Uncorrected visual acuity: Before and after the intervention, the standard logarithmic distant vision chart (Jiangsu Suhong Medical Instrument Co., Ltd.) was used for examination and recording. All children used the same standard logarithmic distant vision chart light box, at a distance of 2.5 m with an illuminance of 160 cd m-2.
Refractive power after cycloplegia: Before and after the intervention, cyclopentolate hydrochloride eye drops (Cyclean) (10 g/L, Alcon Laboratories, Belgium, National Drug Approval No. HJ20160661) were instilled into the conjunctival sac for cycloplegia. After 30 min, the refractive power was measured and recorded using an automatic computer refractometer (NIDEK, Japan, ARK-1).
Axial length: Before and after the intervention, the ophthalmic optical biometer (Haag-Streit AG, HAAG-STREIT DIAGNOSTRICS, LS 900) was used to measure and record the axial length.
Record the age, gender, history of sweet food preference, obesity status, disease duration, outdoor activity <2 h/day, use of electronic devices >2 h/day, night sleep time <7 h/day of the children record the occurrence of adverse events in the children during the intervention period respectively record the visual fatigue symptom scores of the patients before and after treatment: Evaluation was conducted from 6 aspects including dry eyes, foreign body sensation, eye pain and swelling, photophobia, headache and fatigue, divided into four dimensions of none, mild, moderate and severe and scored 0,1,2 and 3 points in sequence. Record the Positive Relative Accommodation (PRA) and Negative Relative Accommodation (NRA) abilities before and after treatment.
Therapeutic effect evaluation
The evaluation was formulated with reference to the diagnostic and therapeutic standards for internal medicine syndromes of traditional chinese medicine of the people's republic of china and the actual clinical situation. Complete recovery after treatment, the uncorrected visual acuity increased to 1.0 or above, or the refractive power of myopia disappeared after mydriasis. Marked effectiveness after treatment, the uncorrected visual acuity increased by 3 or more rows, or the refractive power of myopia decreased by 1.00 D or more after mydriasis. Effectiveness after treatment, the uncorrected visual acuity increased by 2-3 rows, or the refractive power of myopia decreased by 0.25-0.75 D after mydriasis. Ineffectiveness after treatment, the uncorrected visual acuity increased by >1 row or remained unchanged, or the refractive power of myopia remained unchanged or increased after mydriasis.
Statistical analysis
SPSS 20.0 software was used for statistical analysis. Measurement data were expressed as (x ± s). When the data were normally distributed, independent sample t-tests were used for comparisons between two groups and within groups; when the data were not normally distributed, rank sum tests were used. Count data were analyzed using Chi-square tests or Fisher's exact tests. The Mann-Whitney U test was used for comparisons of ordinal data between two groups. A p<0.05 was considered statistically significant. Multivariate logistic regression analysis was conducted on statistically significant indicators to determine the risk factors for the ineffectiveness of the "Siming Acupoints" massage technique in the treatment of myopia in children and adolescents. The Receiver Operating Characteristic (ROC) curve of risk factors was described and the area under the curve was calculated. The Intra-Class Correlation Coefficient (ICC) was used to assess the consistency between two observers.
Clinical efficacy
257 patients with 475 eyes received and completed the treatment course on time. At the last follow-up, based on the clinical efficacy, they were divided into the ineffective group and the effective group. Among the ineffective group, there were 26 patients with 33 eyes, accounting for 6.95%, with an average age of 8.61 ± 2.29 years and a disease duration of 14.03 ± 10.70 months. Among them, 12 eyes had high myopia, accounting for 36.36%; 14 eyes had moderate myopia, accounting for 42.42% and 7 eyes had low myopia, accounting for 21.21%. Among the effective group, there were 231 patients with 442 eyes, accounting for 93.05%, with an average age of 8.24 ± 2.21 years and a disease duration of 8.71 ± 8.96 months. Among them, 13 eyes had high myopia, accounting for 2.94%; 62 eyes had moderate myopia, accounting for 14.02% and 367 eyes had low myopia, accounting for 83.03%. There was no significant difference in age, gender or the proportion of obese patients between the two groups (p>0.05).
Treatment effectiveness rate: After the intervention, a total of 257 children with 475 eyes were cured, 295 (62.10%), showed marked improvement, 69 (14.53%), showed improvement, 78 (16.42%), were effective, 33 (6.95%) were ineffective and the total effective rate was 93.05% the low myopia group had 374 eyes cured, 280 (74.87%), showed marked improvement, 39 (10.43%), showed improvement, 48 (12.83%), were effective and 7 (1.87%) were ineffective, with a total effective rate of 98.13% the moderate myopia group had 76 eyes cured, 15 (19.74%), showed marked improvement, 26 (34.21%), showed improvement, 21 (27.63%), were effective and 14 (18.42%) were ineffective, with a total effective rate of 81.58% the high myopia group had 25 eyes, 4 showed marked improvement (16.00%), 9 showed improvement (36.00%), 12 showed no improvement (48.00%) and the total effective rate was 52.00% (Table 1).
| Group | Recovery (only) | Efficacy (only) | Effectiveness (only) | Ineffectiveness (only) | Efficacy rate |
|---|---|---|---|---|---|
| Mild myopia | 280 | 39 | 48 | 7 | 98.13% |
| Moderate myopia | 15 | 26 | 21 | 14 | 81.58% |
| High myopia | 0 | 4 | 9 | 12 | 52.00% |
| Total number of eyes | 295 | 69 | 78 | 33 | 93.05% |
Table 1: Treatment effectiveness of myopia at different severity levels.
Changes in various indicators before and after the intervention
There were no significant differences in equivalent spherical diopter and axial length before and after the intervention (both p>0.05). The score of visual fatigue symptoms after the intervention (7.54 ± 1.58) was significantly lower than that before the intervention (11.87 ± 1.74) and the difference was statistically significant (p<0.001). The uncorrected visual acuity after the intervention (1.02 ± 0.46) was significantly higher than that before the intervention (0.43 ± 0.19). The abilities of NRA (2.10 ± 0.21) D and PRA (-2.03 ± 0.42) D after the intervention were significantly enhanced compared with NRA (1.86 ± 0.24) D and PRA (-1.86 ± 0.33) D before the intervention and the differences were statistically significant (both p<0.001) (Table 2).
| Indicators | Before intervention | After intervention | p-value |
|---|---|---|---|
| Equivalent spherical power (D, x̄ ± s) | -2.33 ± 1.90 | -2.35 ± 1.89 | 0.908 |
| Visual fatigue symptom score (x̄ ± s) | 11.87 ± 1.74 | 7.54 ± 1.58 | <0.001 |
| Eye axial length (D, x̄ ± s) | 24.07 ± 1.27 | 24.19 ± 1.27 | 0.155 |
| Naked eye vision (x̄ ± s) | 0.43 ± 0.19 | 1.02 ± 0.46 | <0.001 |
| Positive Relative Accommodation (PRA) (D,x̅ ± s) | -1.86 ± 0.33 | -2.03 ± 0.42 | <0.001 |
| Negative Relative Accommodation (NRA) (D,x̅ ± s) | 1.86 ± 0.24 | 2.10 ± 0.21 | <0.001 |
Table 2: Comparison of indicators before and after intervention.
Safety evaluation
No adverse events occurred during the treatment for all patients. The massage technique on the "Siming Acupoints" for treating myopia in children and adolescents is safe and effective.
Analysis of risk factors affecting therapeutic effects
Consistency results: To evaluate the consistency among and between observers, the ICC values were calculated. The intra-observer ICC value and inter-observer ICC value were 0.845 and 0.829, respectively, indicating good consistency.
Basic information
The proportion of patients with a history of sweet food preference in the ineffective group was significantly higher than that in the effective group and the difference was statistically significant (p=0.020). The disease duration in the ineffective group was significantly longer than that in the effective group and the difference was statistically significant (p=0.001). Moreover, there was a significant difference in the degree of myopia between the two groups, and the difference was statistically significant (Table 3).
| Indicators | Invalid group (n=33) | Valid group (n=442) | p-value |
|---|---|---|---|
| Age (years, x̄ ± s) | 8.61 ± 2.29 | 8.24 ± 2.21 | 0.357 |
| Gender (example, male/female) | 17/16 | 246/196 | 0.644 |
| Sweet tooth history (example, yes/no) | 13/20 | 96/346 | 0.02 |
| Obesity (example, yes/no) | 24-Sep | 69/373 | 0.081 |
| Duration of illness (months, x̄ ± s) | 14.03 ± 10.70 | 8.71 ± 8.96 | 0.001 |
| Myopia severity (example) | |||
| Mild myopia | 7 | 367 | <0.001 |
| Moderate myopia | 14 | 62 | |
| High myopia | 12 | 13 | |
| Number of patients (example, x̄ ± s) | 26 | 231 | |
Table 3: Comparison of basic information between the two groups of patients.
Vision indicators
The spherical equivalent refractive error, cylindrical refractive error and axial length of the ineffective group were significantly higher than those of the effective group, with statistically significant differences (all p<0.001). The axial length of the ineffective group was (24.66 ± 1.32) mm, which was significantly longer than that of the effective group (24.03 ± 1.25) mm, with a statistically significant difference (p=0.005). The treatment-before-treatment corrected visual acuity of the ineffective group (0.25 ± 0.17) was significantly lower than that of the effective group (0.44 ± 0.19), with a statistically significant difference (p<0.001). The first treatment corrected visual acuity of the ineffective group (0.05 ± 0.06) was also significantly lower than that of the effective group (0.60 ± 0.33), with a statistically significant difference (p<0.001). There were no significant differences in the proportion of astigmatic eyes, NPA, and PRA before intervention between the two groups (all p>0.05) (Table 4).
| Indicators | Invalid group (n=33) | Valid group (n=442) | p-value |
|---|---|---|---|
| Spherical lens power (D, x̄ ± s) | -4.30 ± 2.47 | -1.78 ± 1.48 | <0.001 |
| Eye axis length (mm, x̄±s) | 24.66 ± 1.32 | 24.03 ± 1.25 | 0.005 |
| Equivalent spherical lens power (D, x̄ ± s) | -5.20 ± 2.94 | -2.12 ± 1.60 | <0.001 |
| Treatment-free visual acuity (x̄ ± s) | 0.25 ± 0.17 | 0.44±0.19 | <0.001 |
| First treatment corrected visual acuity (x̄ ± s) | 0.05 ± 0.06 | 0.60 ± 0.33 | <0.001 |
| Cylindrical lens power (D, x̄ ± s) | -1.81 ± 1.60 | -0.69 ± 0.82 | <0.001 |
| Astigmatism (example, yes/no) | 30/3 | 266/76 | 0.077 |
| Pre-intervention NPA (D, x̄ ± s) | 1.86 ± 0.23 | 1.87 ± 0.24 | 0.82 |
| Pre-intervention PRA (D, x̄ ± s) | -1.88 ± 0.34 | -1.86 ± 0.33 | 0.791 |
Table 4: Comparison of visual indicators between two groups of patients.
Lifestyle habits
The proportion of patients with outdoor activities <2 h/d and night sleep time <7 h/d in the ineffective group was significantly greater than that in the effective group and the differences were statistically significant (p=0.022, p=0.012) there were no significant differences between the two groups in terms of using electronic devices for more than 2 h/d, preoperative visual fatigue symptom score and parents' myopia status (all p>0.05) (Table 5).
| Indicators | Invalid group (n=33) | Valid group (n=442) | p-value |
|---|---|---|---|
| Outdoor activities<2 h per day (example, yes/no) | 23/10 | 217/225 | 0.022 |
| Use of electronic devices>2 h per day (example, yes/no) | 18/15 | 174/268 | 0.087 |
| Nightly sleep duration<7 h per day (example, yes/no) | 13/20 | 91/351 | 0.012 |
| Treatment for symptoms of myopia (mean ± standard deviation) | 11.82 ± 1.79 | 11.88 ± 1.74 | 0.855 |
| Parents' myopia status (example) | - | - | - |
| Both parents are myopic | 10 | 140 | 0.079 |
| One parent is myopic | 17 | 270 | |
| Both parents are not myopic | 6 | 32 |
Table 5: Comparison of lifestyle habits.
Multivariate logistic regression analysis
Taking whether the treatment was effective as the dependent variable and other factors as independent variables, a binary multivariate logistic regression analysis was conducted as shown in Table 6. The model classification ability was 93.0% and the model was effective as verified by the chi-square test (x2=79.850, p<0.001). Combined outdoor activities <2 h/d (OR=8.270, p<0.001), equivalent spherical dioptre (Odds Ratio (OR)=2.724, p=0.005) and night sleep time <7 h/d (OR=2.507, p=0.014) were risk factors for the ineffectiveness of the "Siming Acupoints" massage technique in the treatment of myopia in children and adolescents (Table 6).
| Indicators | β | Standard Error (SE) | Wald value | p-value | Odds Ratio (OR) value | 95% Confidence Interval (CI) |
|---|---|---|---|---|---|---|
| Duration of illness | 0.015 | 1.305 | 0.407 | 0.524 | 1.015 | 0.970-1.062 |
| Sweet tooth history | -0.344 | 0.49 | 0.491 | 0.484 | 0.709 | 0.271-1.855 |
| Outdoor activity <2 h/day | 2.113 | 0.564 | 14.013 | <0.001 | 8.27 | 2.736-24.995 |
| Spherical lens power | -0.543 | 0.405 | 1.793 | 0.181 | 0.581 | 0.263-1.286 |
| Equivalent spherical power | 1.002 | 0.361 | 7.721 | 0.005 | 2.724 | 1.344-5.525 |
| Uncorrected visual acuity before treatment | 2.906 | 1.729 | 2.823 | 0.093 | 18.276 | 0.616-542.053 |
| Nightly sleep duration <7 h/day | 0.919 | 0.375 | 6.002 | 0.014 | 2.507 | 0.863-1.007 |
| Eye axial length before treatment | 0.014 | 0.228 | 0.004 | 0.952 | 1.014 | 0.649-1.584 |
Table 6: Multivariate logistic regression analysis of treatment failure.
ROC curve
The ROC curve reveals that the area under the curve for outdoor activities <2 h/d is 0.603; the area under the curve for the equivalent spherical diopter is 0.678 and the area under the curve for night sleep duration <7 h/d is 0.667 (Figure 1).
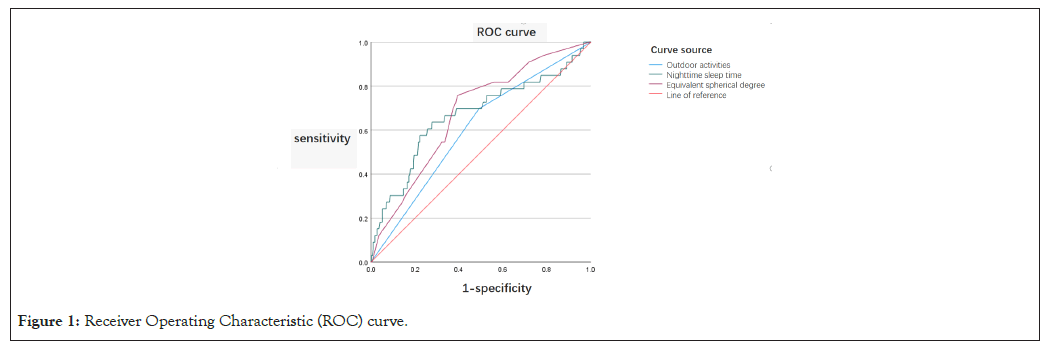
Figure 1: Receiver Operating Characteristic (ROC) curve.
The "Siming Acupoints" encompass Jingming (BL1), Shangming (EX-HN19), Yiming (EX-HN13) and Guangming (GB37) acupoints. Jingming (BL1) acupoints is situated adjacent to the eye in a slightly superior and depressed region of the inner canthus it serves as an intersection point for the hand taiyang, foot taiyang and foot yangming meridians. Stimulation of this acupoint facilitates the ascent of qi and nourishes ocular tissues. The area surrounding jingming contains abundant neurovascular structures superficially it includes the angular artery and vein as well as the superior and inferior trochlear arteries and veins along with their respective nerves. Deeper structures comprise the ophthalmic artery vein and nerve while superiorly lies the nasociliary nerve [10]. Liu et al., suggested that stimulation of Jingming enhances ganglion cell excitability, improves retinal function, accelerates stimulus conduction, increases periocular blood flow and exerts a protective effect on the optic nerve [11]. Guangming (GB37) functions as a collateral acupoint within the gallbladder meridian linked to liver health an organ associated with visual acuity. Stimulating Guangming promotes dilation of the Central Retinal Artery (CRA), enhances ocular blood circulation by increasing oxygenation and nutrient delivery to ocular tissues thereby improving metabolic conditions in structures such as retinae and sclerae [12]. Furthermore, massaging Guangming balances sympathetic and parasympathetic nervous activities effectively alleviating discomforts like muscle tension or dryness resulting from prolonged visual tasks [13,14]. Studies indicate that stimulating Guangming elevates activity levels in occipital brain regions responsible for processing visual information thus contributing to improved vision outcomes [15,16]. Yiming (EX-HN13) is classified as an extraordinary acupoint located at one posterior to Yifeng (SJ17) on the nape of neck where various nerves including greater auricular nerve and lesser occipital nerve are distributed alongside deeper vagus trunk and accessory trunk components. Research has confirmed that stimulation at Yiming significantly augments cerebral blood supply nourishing cranial nerves while promoting recovery in conduction reflex functions among brainstem neurons enhancing arterial circulation overall [17]. Yu et al., also highlighted its notable efficacy against refractory eye diseases through their investigations into this acupoint's therapeutic potential [18]. Shangming (EX-HN19) resides directly beneath midpoint between eyebrow arches within depression below upper orbital margin anatomically positioned amidst orbicularis oculi muscle containing supraorbital nerve superficially whilst deeper layers harbor temporal branch facial nerves plus frontal arteries. Luo et al., discovered effective reductions achieved via stimulating shang ming regarding both diurnal nocturnal intraocular pressures alongside improvements observed across visual fields optic nerves facilitating enhanced ocular perfusion rates [19]. Additional studies have demonstrated how targeted interventions here improve microcirculation around eyes bolstering metabolism amongst scleral, retinal and optic neural tissues concurrently amplifying bioelectrical activity present within centers governing sight restoring functionality therein [20]. Collectively these findings underscore significant roles played by “Siming Acupoints” when addressing ophthalmological disorders whilst enhancing overall eyesight quality. In prior research conducted by our team utilizing simulated stimulations targeting specific acupuncture points surrounding guinea pig models exhibiting myopia we found massage techniques derived from “Siming Acupoints” effectively inhibited progression related changes seen concerning refractive errors delaying axial elongation rates demonstrating intervention capabilities towards mitigating myopic developments [21]. This may correlate closely with massages ability maintain choroidal vascular integrity preserving structural coherence amongst scleral /retinal tissue morphology normalization processes. Additionally results indicated upregulation TGF-β1, Smad2, Smad3 protein expressions noted upon application whereas down regulation Smad7 expression occurred correlating tightly remodeling phenomena occurring during myopic states suggesting possible mechanisms underpinning effectiveness observed herein. Massaging four bright acupuncture points appears beneficial not only increasing patients naked-eye vision but also ameliorating NRA, PRA and symptoms associated fatigue controlling growth patterns axial lengths equivalent spherical lens degrees. Regulatory capacity constitutes vital metrics assessing onset progression pertaining myopia wherein children adolescents typically exhibit declines manifested through lagging responses insufficient relaxation reserves etc [22]. Enhancing regulatory abilities could play pivotal roles delaying preventing occurrences developments relating Myopia.
The "Siming Acupoints" massage therapy for treating myopia in children and adolescents is deemed safe and reliable however, a subset of patients remains unresponsive to treatment. Consequently, analyzing the risk factors associated with treatment failure and further delineating the applicability of "Siming Acupoints" massage therapy for myopia holds significant clinical relevance. The research identified excessive equivalent spherical power, outdoor activity less than 2 h per day and nightly sleep duration under 7 h as independent risk factors contributing to treatment ineffectiveness. Subsequent analyses will explore the mechanisms underlying these effects on myopia development.
This study concludes that equivalent spherical power serves as an independent risk factor for the ineffectiveness of "Siming Acupoints" massage therapy in addressing childhood and adolescent myopia. The efficacy rate within the high myopia cohort was merely 52%, indicating challenges in achieving substantial therapeutic outcomes. In contrast, low myopia participants exhibited an efficacy rate of 98.13% alongside a cure rate of 62.10%. These findings underscore notable limitations inherent to "Siming Acupoints" massage therapy, satisfactory results are particularly elusive among individuals with high myopia while those with low myopia demonstrate marked improvement. Thus, early intervention is critical for children and adolescents at risk of developing myopia to optimize therapeutic effectiveness.
Recent studies have revealed that environmental factors increasingly contribute to the onset and progression of myopia [23]. Extended outdoor time has been identified as the most significant environmental factor capable of delaying myopia's onset. A 2015 study indicated that for children aged 6-7, an additional 40 min of outdoor activity at school could effectively reduce the prevalence of myopia over a three-year period [24]. Evidence suggests that increased near work and study time, coupled with reduced outdoor activities during home quarantine due to the COVID-19 pandemic, correlates with worsening myopia [25]. Saxena et al., demonstrated that daily outdoor exposure exceeding two hours can significantly lower the incidence rate of myopia [26]. One proposed mechanism underlying this protective effect is that exposure to higher light levels stimulates retinal dopamine release, which in turn inhibits axial elongation. Animal studies have shown that retinal dopamine plays a critical role in regulating ocular growth and refractive errors [27]. Furthermore, high-intensity outdoor light promotes vitamin D synthesis, which may directly influence scleral tissue by exerting anti-proliferative effects, thereby delaying both axial growth and changes in refraction. Additionally, compared to indoor settings, outdoor environments provide a broader visual field, engaging in distant vision helps alleviate ciliary muscle tension and reduces eye fatigue. Some research indicates that insufficient ultraviolet exposure may inhibit genes associated with myopia protection, complicating efforts to control its development; conversely, moderate ultraviolet radiation can mitigate scleral remodeling and prevent axial elongation through collagen modulation thereby affecting ocular refractive development [28]. This study also identifies less than two hours of daily outdoor activity as an independent risk factor contributing to the ineffectiveness of "Siming Acupoints" massage therapy for treating myopia among children and adolescents. As highlighted above, engagement in outdoor activities is critical for both preventing and managing myopia; adequate participation in such activities supports effective treatment strategies while inhibiting disease progression.
Additionally, recent research has established a significant association between sleep duration and the development of myopia, revealing a negative correlation between sleep duration and the incidence of childhood myopia [29]. A cross-sectional study involving 3,625 participants aged 12-19 in South Korea found that for each hour of reduced sleep time, refractive error increased by 0.10 D [29]. In a study examining the relationship between sleep duration and myopia in Chinese children, it was observed that those who slept less than 7 h per night had a 3.37-fold higher risk of developing myopia compared to their peers who slept more than 9 h per night [30]. Research conducted by Chakraborty et al., indicated that shorter sleep durations (<7 h/d) and irregular sleep-wake patterns were significantly associated with self-reported risks of myopia among children and adolescents. Some studies propose that insufficient sleep disrupts the biological clock, subsequently affecting ocular circadian rhythms and contributing to the onset of myopia. The retinal circadian clock serves as a central mechanism regulating signals pertinent to ocular axial growth, interactions between retinal neurotransmitter responses and this clock control the diurnal rhythm governing eye growth and size, thereby influencing both axial growth and refractive development [31]. Previous animal studies have corroborated these findings regarding circadian influences on eye development [32]. Melatonin-one of the primary regulators of circadian rhythms-is secreted in greater quantities under dark conditions, it interacts synergistically with melatonin receptors on the retina to facilitate regulation of both eye growth/development and circadian rhythmicity [33]. Circadian rhythms are observed in parameters such as axial length, choroidal thickness and intraocular pressure [34]. Under normal circadian conditions, the axial length is longest during daylight hours and shortest at night, while the choroid exhibits maximal thickness at night and minimal thickness during the day [35]. Disruption of circadian rhythms due to sleep deprivation results in shifts in both daily axial and choroidal rhythms, which can contribute to myopia development [36]. Some studies indicate that sleep duration does not have a significant causal relationship with myopia incidence, however, factors such as good sleep quality, early bedtimes and late awakenings may offer protective effects against myopia [37]. The relationship between sleep duration and myopia remains ambiguous, nonetheless, this study found that nightly sleep durations of less than 7 h represent an independent risk factor for the ineffectiveness of "Siming Acupoints" massage treatment. Patients with nightly sleep durations below this threshold are unlikely to achieve effective therapeutic outcomes. Therefore, adequate night time sleep is likely beneficial for managing myopia.
In summary, "Siming Acupoints" massage therapy has the potential to enhance patients' unaided visual acuity, improve Near Response Amplitude (NRA), Positive Relative Accommodation (PRA) and alleviate symptoms of visual fatigue while also controlling axial length and mitigating increases in equivalent spherical power. This therapeutic modality demonstrates significant efficacy in treating mild myopia among children and adolescents however, it exhibits considerable limitations when addressing high myopia. Factors such as outdoor activity duration of >2 h per day, excessively high equivalent spherical power and night time sleep duration of >7 h per day may serve as independent risk factors that compromise the effectiveness of "Siming Acupoints" massage therapy for true myopia in this population. Therefore, early intervention and treatment are essential for achieving optimal therapeutic outcomes in children and adolescents with myopia. Sufficient outdoor activity time and adequate night time sleep duration are critical determinants ensuring the efficacy of "Siming Acupoints" massage therapy for managing true myopia in children and adolescents.
This research is a single-center one with a relatively small sample size. Consequently, the results are incidental and less convincing. Fewer factors were included and the analysis was not comprehensive. At present, the research on the intervention mechanism of "Siming Acupoints" in treating myopia is incomplete and its recognition remains inadequate.
This study was performed in line with the principles of the Declaration of Helsinki. The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of Affiliated Hospital of Shandong University of Traditional Chinese Medicine(2020-027-KY). All participants signed informed consent forms.
The authors declare no competing interests with regard to this manuscript.
Yan Liu: Methodology, Software, Investigation, Writing-original draft; Qi Xun: Supervision, Project administration, Yazheng Pang: Conceptualization, Resources, Xuan Zhang: Software, Investigation, Juan Yu: Conceptualization, Resources, Supervision, Project administration.
The work was supported by National Natural Science Foundation of China (82474670), the TCM science and technology project of Shandong Province (No: Z-2022088T) and the Jinan science and technology plan project (No :201907105).
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref]
[Crossref]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref]
[Crossref]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Liu Y, Yu J, Xun Q, Pang Y, Zhang X. (2024). Clinical Effect and Multi-Factor Analysis of "Siming Acupoints" Massage in the Treatment of Myopia in Children and Adolescents. Clin Pediatr. 9:283
Received: 21-Oct-2024, Manuscript No. CPOA-24-35648; Editor assigned: 23-Oct-2024, Pre QC No. CPOA-24-35648 (PQ); Reviewed: 06-Nov-2024, QC No. CPOA-24-35648; Revised: 13-Nov-2024, Manuscript No. CPOA-24-35648 (R); Published: 21-Nov-2024 , DOI: 10.35248/2572-0775.24.9.283
Copyright: © 2024 Liu Yet al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited