
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2023)Volume 14, Issue 5
Background: Since preventable by vaccination, tetanus is a rare condition, yet two-third of the worldwide cases of this potentially fatal condition occur in Africa. Most tetanus cases need a surgical procedure (wound debridement mostly), and anesthesia is challenging because of the disease’s potential to cause autonomic dysfunction and muscle stiffness. So far, no consensus for the better anesthesia technique has been described in the literature, and to our knowledge no data about sole ultrasound-guided locoregional anesthesia for limb surgical procedure of the tetanus patient has been published.
Case presentation: A 22-year-old male tetanus patient presented with an infected gunshot wound on the right forearm with a right radio-ulnar fracture and gangrene of the distal half of the right forearm planned for immediate amputation. The anesthesia was achieved by combining unilateral ultrasound-guided supraclavicular and infraclavicular brachial plexus block. The loco-regional anesthesia was effective throughout the duration of surgery without further need for additional anesthetic techniques.
Conclusion: It is an original case report, which raises awareness to consider loco-regional anesthesia as a possible safe alternative to general anesthesia in a tetanus case, which is interesting in low resources settings, where general anesthesia and intubation can be correlated with higher risks. Furthermore, it discusses the option of performing a combined blocks approach in case of concerns about partial failure with a single plexus block. We believe this report could be helpful for anesthesiologists confronted to the difficult and rare situation of taking care of a tetanus patient.
Tetanus; Amputation; Anesthesia; Supraclavicular brachial plexus block; Infraclavicular brachial plexus block
Tetanus is caused by a toxin generated by Clostridium tetani. It is a fatal condition marked by spastic paralysis and growing muscular tension [1]. Africa accounts for two-thirds of all tetanus cases worldwide [2]. Development, germination, and neurotoxic synthesis only occur in wounds with low oxidation-reduction potentials, such as gangrenous tissue, foreign substances, or unclean wounds; this might promote anaerobic growth [3]. Bacteria from an infected wound migrate backwards through the nervous system, infecting motor neurons before reaching the neuron cell body in the spinal cord and brain stem [4]. Anesthesia for tetanus patients may be more challenging because of the disease's potential to cause autonomic dysfunction and skeletal muscle stiffness. Remifentanil is only one of several new sedative and opioid medicines that have not undergone extensive testing for use in treating tetanus [5].
A 22-year-old man was admitted with an infected Gunshot Wound (GSW) on his right forearm, which had resulted in a radio-ulnar fracture and gangrene (Figure 1).

Figure 1: Patient presented with an infected Gunshot Wound (GSW) on the right forearm with a right radio-ulnar fracture and gangrene of the distal half of the right forearm.
On admission, the patient was fully conscious and oriented. The vital signs were heart rate 134 beats/min, blood pressure 110/70 mm/Hg, oxygen saturation 97% on room air, temperature 38.6°C, taking abnormal posture with extended neck and fully extending his body, sweating, clenching his teeth with speaking difficulty and a gangrenous right forearm. The patient was severely infected and borderline septic, mostly tetanus (clinically), indicating immediate above-elbow amputation surgery (Figure 2).
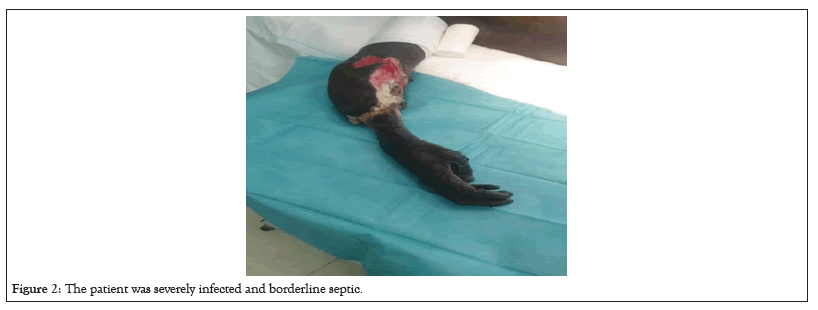
Figure 2: The patient was severely infected and borderline septic.
The case received Tetanus Toxoid vaccine, Tetanus Immunoglobulin 500 IU, and loading dose of Intravenous (IV) 2 gms Cefazoline, 500 mg metronidazole and 240 mg gentamycin as per the ICRC weapon wounded antibiotic protocol [6].
Intervention
Upon arrival at the operating room, an IV 16G-cannula was inserted. The patient was monitored (pulse oximetry, temperature probe, noninvasive blood pressure, and 5-lead ECG). The patient was placed on a face mask, and 1 L Ringer's lactate solution infusion was started, 1 mg of midazolam and 50 μg of fentanyl IV.
The decision was taken to administer regional anesthesia with a combined block on the same side to decrease the failure possibilities and avoid any stimulation effects and laryngeal spasms. In our low resource context where the inavailability of well-equipped high-dependency units including mechanical ventilation and well-trained staff, render general anesthesia less safe. In addition, other nonclinical factors such as a security curfew that might prevent the clinical team to monitor the patient freely in the postoperative period were also taken into consideration. The patient was kept supine with the head turned to the opposite side of the block. The combined block was achieved on the same side by supraclavicular brachial plexus block with 20 ml of lidocaine 1% with epinephrine 5 μg/ml and infraclavicular brachial plexus block with 15 ml of levobupivacaine 0.5% with epinephrine 5 μg/ml. A 6-13 MHz linear probe (Sonosite M turbo US machine) was placed in a parasagittal plane medial to the coracoid process and inferior to the clavicle under aseptic conditions. The pulsating axillary artery was visualized. The 5 cm, short-beveled, 20 gauge, stimiplex B. Braun needle was placed in-plane from cephalic to caudal below the clavicle. To create a U-shaped spread, 15 ml of levobupivacaine 0.5% with epinephrine 5 μg/ml was administered posteriorly.
Transducer placement for the supraclavicular block occurs in the transverse plane just proximal to the clavicle, somewhat posterior to the clavicle's midpoint. For cross-sectional imaging of the subclavian artery, the transducer was angled caudally, as if to scan the chest and the brachial plexus was identified. A short-beveled, 20-gauge, stimiplex, B. Braun needle was placed in plane toward the brachial plexus in a lateral to medial direction, then 20 ml of lidocaine 1% with epinephrine 5 g/ml was injected.
The surgery lasted about one and a half hours without further need for additional anesthetics or adjuncts (Figure 3).
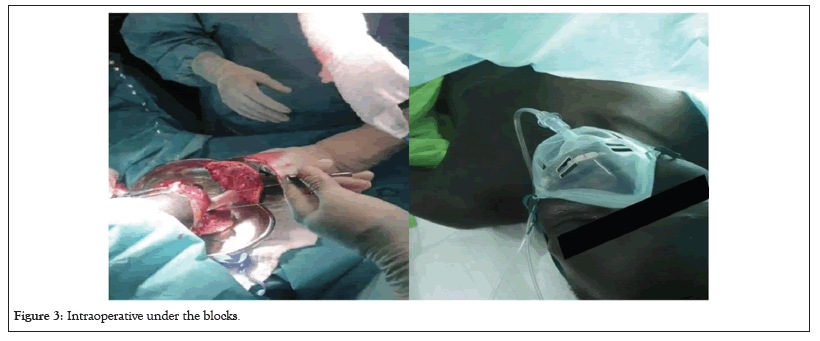
Figure 3: Intraoperative under the blocks.
Postoperatively antibiotics (Cefazoline 1 gm intravenous (IV) Three times a Day (TID), Metronidazole 500 gm (TID), Gentamycin 240 mg IV (OD), anti-convulsant (Diazepam 10 mg IV TID), Tramadol 100 mg IV TID, Paracetamol 1 gm PO QID, Ibuprofen 400 mg PO TID, Carbamazepine 200 mg two times a day (BID) for phantom limb pain prevention, RL 1L (BID).
Two days later, the patient’s condition regarding the tetanus infection deteriorated and the number of spasms was more frequent, hence tracheostomy was done under local anesthesia, followed by Nasogastric Tube (NGT) insertion, to protect the airway from any stimulus that may lead to stridor or laryngeal spasms showed in Figure 4. After 5 days, the Delayed Primary Closure (DPC) for the amputated stump was done using the same regional anesthesia approach (combined block) (Figure 4).

Figure 4: Intraoperative tracheostomy followed by NGT insertion.
Outcome and follow-up
The patient was closely monitored in the HDU in a dark and quiet place. He continued on Cefazoline, metronidazole for three weeks, morphine 5 mg BID IV was added to the analgesic plan, enoxaparin 40 mg SC OD started and continued till initiation of ambulation, feeding with blended diet trough NGT (2500 Kcal, 35 Kcal/Kg) and Lactulose 10 ml TID before each meal.
By day 11 post-amputation, the patient's symptoms started to improve and the patient was followed up in the HDU till 21 days’ post-amputation (Figure 5).
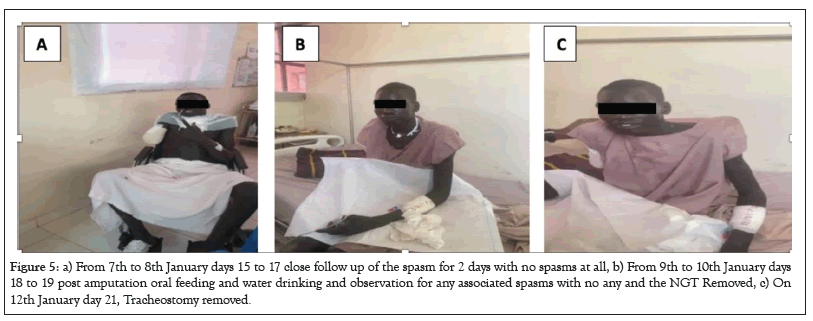
Figure 5: a) From 7th to 8th January days 15 to 17 close follow up of the spasm for 2 days with no spasms at all, b) From 9th to 10th January days 18 to 19 post amputation oral feeding and water drinking and observation for any associated spasms with no any and the NGT Removed, c) On 12th January day 21, Tracheostomy removed.
Tetanospasmin, a metalloprotease, disrupts the normal function and transmission of motor, sensory, and autonomic neurons, leading to the clinical manifestations of tetanus [3]. Tetanospasmin takes a backward route to the brain and spinal cord through axons. The clinical presentation of muscular stiffness is consistent with the findings of the radiolabelled assay revealed that tetanospasmin favors inhibitory motor neurons. Tetanus toxin reduces motor nerve inhibition and causes the typical muscle spasm by interfering with the development of the Soluble N-ethylmaleimide-sensitive factor Attachment protein Receptor (SNARE) complex. Autonomic dysregulation and hypertensive episodes can be caused by tetanus toxin because of its action at the central excitatory synapses, where it binds to sympathetic adrenergic neurons [3].
Control of skeletal and muscular stiffness, muscle spasms, and autonomic dysfunction may be challenging during anesthetic treatment for patients with severe tetanus [7]. Patients with tetanus require surgical operations such as debridement, tracheostomy, etc. There is a lack of data to support the use of any particular anesthetic technique [7].
To avoid causing spasms and hypertensive crisis, procedures on patients with mild tetanus should be performed when they are deeply anesthetized. Premedication with sedatives and analgesics and avoidance of excessive stimulation are imperative. Sedation in a quiet, dark environment are standard first steps in treating muscular spasms [8].
The risks associated with general anesthesia were too great to be taken. While in most tetanus cases general anesthesia is used, and the patient is then mechanically ventilated after surgery in the intensive care unit, this was not an option in our case, so we decided to combine brachial plexus block to eliminate the risk of anesthesia failure, as well as to prevent laryngeal stimulation and spasms. No previous study has combined supraclavicular and infraclavicular brachial plexus blocks for amputations due to tetanus when dealing with a neglected weapon-wounded patient.
In the present study, the surgery started 5 mins after anesthesia induction, lasted about one and a half hours, and was effective during the duration of surgery without further need for additional anesthetic techniques.
Procedures involving the upper arm (from the mid-humerus to the hand) benefit greatly from a block to the supraclavicular brachial plexus block. Blocking the brachial plexus at the level of the trunks produced by the C5-T1 nerve roots is most likely to affect all of the plexus's branches. Because of this, upper limb surgery and anesthesia are more likely to be successful (excluding the shoulder). An ultrasound device or an anatomical marker is used to perform this block (with or without the use of a nerve stimulator) [9].
The addition of the infraclavicular block would provide a denser block since it would simultaneously anesthetize the axillary, subscapular, and lateral pectoral nerves [9].
Supporting our results, Musso et al., [10] concluded that after total shoulder arthroplasty, a combination of suprascapular and infraclavicular nerve blocks was associated with a successful block in 95% of patients, a promising postoperative analgesic profile, a short performance time, and a favorable safety profile.
In a previous case report, forearm amputation patients who require acute pain management may benefit from an infraclavicular brachial plexus block, since it facilitates repeated visits to the operating room and postoperative rehabilitation while reducing perioperative blood loss [11]. Moreover, O'Brien et al., also support using regional anesthesia for patients undergoing limb amputation [12].
Kulkarni et al., [13] concluded that in the case of tetanus, Safe surgical techniques that include the use of volatile anesthetic agents include wound cleansing and debridement, removal of a foreign body, and incision and drainage of an abscess. However, a muscle relaxant that does not cause hypotension should be used.
We present a rare case of a 22-year-old male patient with an infected gangrenous gunshot wound and found that supraclavicular brachial plexus blocks, as a type of regional anesthesia and infraclavicular brachial plexus block is a potentially effective treatment modality for acute pain control for above elbow amputation in tetanus patient with no need for further anesthetic techniques.
A written informed consent has been obtained from the patient for publication of the submitted article and accompanying images.
All data generated or analyzed during this study are included in this article [and/or] its supplementary material files. Further inquiries can be directed to the corresponding author.
The authors certify that they have no commercial associations that might pose a conflict of interest in connection with the submitted report.
No funding sources are supporting the work. All institutional or corporate affiliations are acknowledged in the article.
We thank all the researchers who have uploaded and shared their databases to make this work possible.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Salman A, Elfarnawany A, Tekie Bahta A, Kumar Baral A, Naetio Ozoilo K, Crespo S (2023) Combined Unilateral Supraclavicular and Infraclavicular Brachial Plexus Blocks Anesthesia for above Elbow Amputation in Tetanus Weapon Wounded Patient in a Low Resource Context: A Case Report. J Anesth Clin Res. 14:1116
Received: 06-Oct-2023, Manuscript No. JACR-23-27594; Editor assigned: 09-Oct-2023, Pre QC No. JACR-23-27594 (PQ); Reviewed: 24-Oct-2023, QC No. JACR-23-27594; Revised: 31-Oct-2023, Manuscript No. JACR-23-27594 (R); Published: 07-Nov-2023 , DOI: 10.35248/2155-6148.23.14.1116
Copyright: © 2023 Salman A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.