
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 9
Background: The anesthesiologist is person solely responsible for airway management of the patients undergoing a surgical procedure. Airway management and endotracheal intubation are fundamental skills for the safe conduct of general anesthesia. Laryngoscopes play an important role in securing airway. They range from simple rigid scopes to complex fiber optic video devices. Successful direct laryngoscopy depends on aligning the axes of oral cavity, pharynx and larynx.
Materials and methods: A total of 60 ASA grade I, II and III adult patients, age 18-60 year, weighing up to 100 kgs posted for elective laparoscopic surgeries undergoing general anaesthesia were equally divided in three groups, twenty patients each after taking written informed consent from the patients, in their own vernacular language. All cases were induced by the same senior anaesthetist.
Group M (n=20)-Conventional Macintosh laryngoscope group.
Group A (n=20)-AirTraQ video laryngoscope group.
Group F (n=20)-FasTrach intubating LMA group.
Results: Duration to intubate in group M was 19.6 ± 4.67 (mean ± SD) seconds, in group A was 8.7 ± 3.27 (mean ± SD) seconds and in group F was 20.3 ± 27.90 (mean ± SD)seconds. Duration of endotracheal intubation between three groups, were comparable and shows statistically significant difference between the three groups. Group A was better than group M and group F.
Conclusion: From the present study it is concluded that AirTraQ video laryngoscope and FasTrach video laryngoscope, newer airway devices, is more user friendly, simple, easy to use as compared to conventional Macintosh laryngoscope.
Macintosh laryngoscope; AirTraQ video laryngoscope; General anaesthesia; Duration of intubation; Haemodynamic parameters
Airway management and endotracheal intubation are fundamental skills for the safe conduct of anesthesia. In any age group, anesthetics should produce rapid induction and recovery. Successful management of the normal and difficult airway requires both trained personal and the proper equipment. Many difficult intubations are not recognized until after induction of anesthesia due to absence of any single factor that reliably predicts the existence of difficult airway. The failure to successfully intubate the trachea and secure air way remains major cause of morbidity and mortality in anesthetic and emergency settings [1]. Macintosh laryngoscope remains the most popular device used to facilitate endotracheal intubation and constitute gold standard despite the recent developments in airway device technologies [2]. AirTraQ Video Laryngoscope is a new intubation device that has been developed to facilitate intubation in patients with normal and difficult airway. As a result of exaggerated curvature of blade and an internal arrangement of optical components, a high-quality view of glottis and surrounding structures is provided without sniffing position [3]. Fastrach laryngeal mask airway is a new intubating laryngeal mask airway device to facilitate intubation in patient with normal and difficult airway. It has a preformed curvature similar to that of the normal adult pharyngeal anatomy. It offers intubation without sniffing position [4]. The main objective of this is to evaluate the intubation time for AirTraQ Video Laryngoscope, Macintosh laryngoscope and Fastrach laryngeal mask airway in adult patients, number of intubation attempts, optimization maneuvers, ease of intubation and cardiovascular changes during intubating an adult patients.
The present study was done to compare endotracheal intubation criteria for conventional Macintosh laryngoscope (group m) versus AirTraQ video laryngoscope (group a) versus fastrach laryngeal mask airway (group f) in adult patients. After taking the institutional ethical committee approval for the study, sixty ASA grade I, II and III adult patients, age 18-60 year, posted for elective laparoscopic surgeries undergoing general anaesthesia were equally divided in three groups, twenty patients each after taking consent from patient in written and informed in their own vernacular language. Patient with following conditions were excluded from the study, age <18 year or >60 year, ASA grade Ⅳ and Ⅳ, patients with pathologies of head and neck region, patients with upper respiratory tract infection, coughing, cardiopulmonary diseases, coagulopathies, raised intracranial tension, allergic to the drugs used in the study and predicted difficult airway, patients undergoing emergency surgeries.
A pre-anaesthetic evaluation was done on the previous day of surgery and was reviewed on the day of surgery. A detailed medical history was taken. Systemic examination was carried out and relevant investigations were advised. The purpose and procedure of the study was explained in their own vernacular language and written informed consent was obtained from the patient in their own language as per hospitals rules and regulations. All the patients were kept nil by mouth 8 hours. Baseline values of pulse in radial artery, respiratory rate, SpO2 with finger probe pulse oxymeter and non-invasive blood pressure were recorded upon arrival of the patient to the preoperative room. After that the 18-gauge or 20-gauge venous cannula was inserted into the dorsum of the hand under all aseptic and antiseptic precautions.
Preparation of equipment
Conventional macintosh laryngoscope: As shown in Figure 1, Macintosh laryngoscope blade was checked before insertion. Circuit connection of Conventional Macintosh laryngoscope was checked before use. Appropriate cuffed portex endotracheal tube was checked for its integrity and was kept ready before insertion. Endotracheal tube was lubricated well. After each use disinfection of device was done.
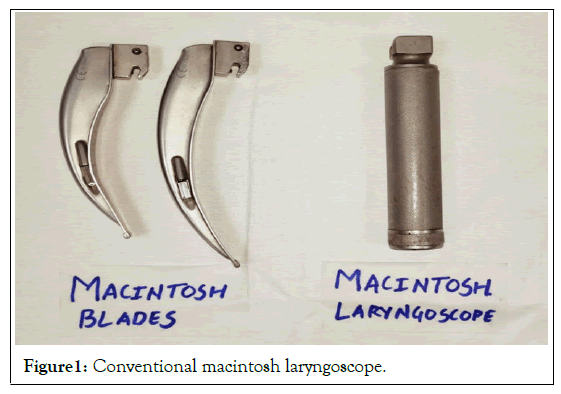
Figure 1: Conventional macintosh laryngoscope.
Airtraq video laryngoscope: As shown in Figure 2, wireless video monitor was kept fully charged. Circuit connection of blade was checked before insertion. Appropriate cuffed portex endotracheal tube was checked for its integrity and was kept ready before insertion. Endotracheal tube was lubricated well and preloaded in AIRTRAQ blade number 3(blue color). After each use disinfection of device was done.
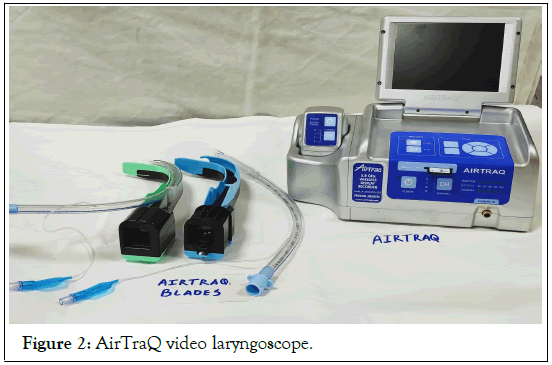
Figure 2: AirTraQ video laryngoscope.
Fastrach laryngeal mask airway: As shown in Figure 3, appropriate size Fastrach intubating LMA were checked and kept ready. Appropriate cuffed silicon endotracheal tube was checked for its integrity and was kept ready with stylet before insertion. Endotracheal tube was lubricated well.
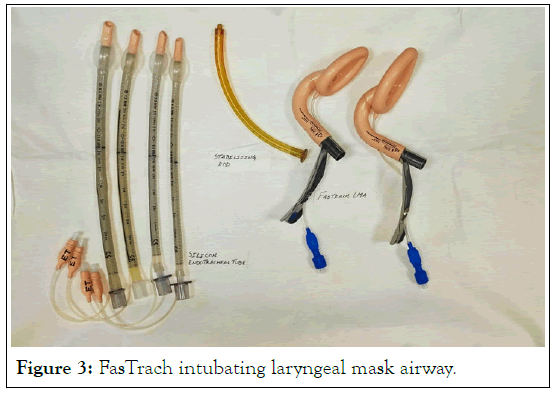
Figure 3: FasTrach intubating laryngeal mask airway.
After each use disinfection of device was done. AirTraQ video laryngoscope, conventional Macintosh laryngoscope and Fastrach LMA. All three devices, first cleaning was done with normal saline followed by disinfecting with 100% alcohol. All the patients were premedicated with Inj. Promethazine 0.5 mg/kg, Inj Pentazocine 0.5 mg/kg, Inj. Glycopyrrolate 4 mcg/kg deep intra muscular 30 min before induction. Inj. Ondansetron 0.1 mg/kg IV, Inj. Midazolam 0.1 mg/kg IV, Inj fentanyl 2 ug/kg IV was given 10 min before induction. After premedication vital data like temperature by palpation, pulse in radial artery, non-invasive blood pressure, respiratory rate and SpO2 with finger probe pulse oxymeter were recorded. All the patients were transferred to operation theatre for operation and monitors like pulse oxymeter, ECG and non-invasive blood pressure cuff were attached to the patient [1].
Induction of anaesthesia
• All the patients in three groups were induced by same consultant anaesthesiologist every time.
• Induction began with application of face mask and was achieved using 100% oxygen.
• Intravenous induction agents with Inj. Propofol 1.5-2 mg/kg i.v.
• After centralization of eyeball, Inj. succinylcholine 2.0 mg/kg i.v was given.
• After giving succinylcholine, intermittent positive pressure ventilation with 100% oxygen was.
At the time of facilitation of appropriate laryngoscope, following points were noted:
1. Time taken for endotracheal tube insertion (in seconds)
2. Numbers of attempts.
3. Any alternative intubation technique or any assistance is required or not.
4. External laryngeal pressure required or not.
5. Use of stylet required or not.
6. Compare hemodynamic stability.
Analgesia was given with Paracetamol 20 mg/kg i.v infusion after induction of anaesthesia. Maintenance of anaesthesia was carried out with 50% oxygen, 50% nitrous oxide, IPPV and bolus of Inj.Atracurium 0.5 mg/kg i.v followed by in doses of 0.1 mg/kg i.v as and when required.
At the end of surgery, port instillation from each port was done for postoperative analgesia with.
• Inj. Lignocaine 1% plain 10 ml (Inj. Lignocaine 2% 5 ml diluted till 10 ml with normal saline).
• Inj. Bupivacaine 0.25% plain 10 ml (Inj. Bupivacaine 0.5% 5 ml diluted till 10 ml with normal saline).
• Inj Tramadol 50 mg (1 cc).
• Inj Magnesium Sulphate 50 mg (0.1 ml).
All the anaesthetic agents were discontinued simultaneously at the end of surgery. After completion of surgery residual neuromuscular block was antagonized by Neostigmine 50 ug/kg and Inj. Glycopyrrolate 10 ug/kg. After adequate reversal of neuromuscular blockade which is observed by limb movements of patient and fulfilling the standard criteria of extubation, endotracheal tube was removed. After removal of endotracheal tube, patient was observed and was shifted to post anaesthesia care unit with pulse oximetry monitoring. Relatives were allowed to sit at the bedside immediately on admission to post anaesthesia care unit [2].
Postoperatively patients were followed up every hourly to asses pain due to surgery. Visual Analog Scale was measured every hourly. At VAS 3 patient were given rescue analgesia with Diclofenac 75 mg i.v Stat [3].
In group a mean age was 37 years with SD 10.62, in group M mean age was 32.55 year and SD 13.45 and in group F mean age was 30.05 years and SD 12.77 which was statistically insignificant. In group a mean weight was 62.5 kgs with SD 7.86, in group M mean weight was 57.95 kgs and SD 9.89 and in group F mean weight was 58 kgs and SD 8.94 which was statistically insignificant.
Table 1 shows comparison of duration of endotracheal intubation. In group M was 19.6 seconds with Standard deviation 4.67 seconds, in group A was 8.7 seconds with Standard deviation 3.27 seconds and in group F was 20.3 seconds with Standard deviation 27.90 seconds [4]. Duration of endotracheal intubation between three groups was comparable and shows statistically significant difference between the three groups. Group A was better than group M and group F (Table 2).
| Mean ± SD (sec) | P value | |||
|---|---|---|---|---|
| M: A | M: F | F: A | ||
| Group M | 19.6 ± 4.67 | <0.0001 highly Significant |
>0.05 not Significant |
<0.0001 highly Significant |
| Group A | 8.7 ± 3.27 | |||
| Group F | 20.3 ± 27.9 | |||
| Note: p value<0.05 is considered significant; NS: Not Significant, HS: Highly Significant, S: Significant | ||||
Table 1: Comparison of duration of endotracheal intubation between three groups.
| TIME | Group M (mean± SD) (per minute) | Group A (mean± SD) (per minute) | Group F (mean± SD) (per minute) | P value | Remarks | ||
|---|---|---|---|---|---|---|---|
| A: M | F: M | F: A | |||||
| Before premedication |
93.7 ± 11.93 | 91 ± 6.06 | 90.7 ± 8.8 | >0.05 | >0.05 | >0.05 | NS |
| After intubation | 108.3 ± 13.63 | 89.6 ± 11.36 | 92.4 ± 9.65 | <0.05 | <0.05 | >0.05 | HS |
| 30 sec | 109 ± 13.89 | 91.6 ± 11.76 | 90.05 ± 7.73 | <0.05 | <0.05 | >0.05 | HS |
| 1 min | 105.1 ± 12.98 | 89.9 ± 10.73 | 90.55 ± 7.25 | <0.05 | <0.05 | >0.05 | HS |
| 3 min | 102.1 ± 13.19 | 88.1 ± 10.18 | 90.1 ± 6.13 | <0.05 | <0.05 | >0.05 | S |
| 5 min | 98.7 ± 11.18 | 87.5 ± 9.21 | 87.4 ± 6.62 | <0.05 | <0.05 | >0.05 | HS |
| 10 min | 94.5 ± 10.15 | 86.8 ± 8.85 | 86.3 ± 6.53 | <0.05 | <0.05 | >0.05 | S |
| 15 mins | 93 ± 9.83 | 87.3 ± 8.51 | 87.4 ± 6.29 | >0.05 | >0.05 | >0.05 | NS |
| 20 mins | 91.1 ± 8.47 | 87.5 ± 7.75 | 86.1 ± 7.9 | >0.05 | >0.05 | >0.05 | NS |
| 25 mins | 90.5 ± 8.17 | 88.1 ± 7.49 | 86.1 ± 8.76 | >0.05 | >0.05 | >0.05 | NS |
| 30 mins | 89.8 ± 8.38 | 86.8 ± 7.43 | 87.3 ± 8.71 | >0.05 | >0.05 | >0.05 | NS |
| 60 mins | 93.22 ± 8.59 | 86.47 ± 8.88 | 87.05 ± 7.78 | >0.05 | >0.05 | >0.05 | NS |
Note: p value<0.05 is considered significant; HS: Highly Significant; NS: Not Significant; S: Significant
Table 2: Comparison of mean pulse rate at different time interval.
When compared with individual group there was no statistical significance for means of pulse rate when Group A and Group F were compared at any time. When compared to individual group there was statistical significance between Group A and Group M, Group F and Group M in mean pulse rate after intubation, at 30 seconds, 1 minute, 3 minutes, 5 minutes, 10 minutes with a P-value<0.05. When compared to individual group there was no statistical significance between Group A and Group M, Group F and Group M in mean pulse rate before premedication, at 15 minutes, 20 minute, 25 minutes, 30 minutes, 60 minute with a P- value>0.05 (Table 3).
| TIME | Group M (mean ± SD) (mmHg) |
Group A (mean ± SD) (mmHg) | Group F (mean ± SD) (mmHg) | P value | Remarks | ||
|---|---|---|---|---|---|---|---|
| A: M | F: M | F: A | |||||
| Before premedication |
91.9 ± 7.71 | 88.13 ± 8.89 | 89.73 ± b6.65 | <0.05 | <0.05 | >0.05 | NS |
| After Intubation |
100.1 ± 6.92 | 91.06 ± 5.41 | 91.33 ± 6.26 | <0.05 | <0.05 | >0.05 | HS |
| 30 sec | 100.83 ± 6.24 | 90.76 ± 6.26 | 91.23 ± 4.66 | <0.05 | <0.05 | >0.05 | HS |
| 1 min | 97.3 ± 6.72 | 89.26 ± 6.91 | 90.53 ± 4.38 | <0.05 | <0.05 | >0.05 | S |
| 3 min | 94.03 ± 4.9 | 90.46 ± 6.09 | 89.56 ± 5.06 | <0.05 | <0.05 | >0.05 | S |
| 5 min | 92.5 ± 5.03 | 90.53 ± 5.53 | 88.43 ± 4.65 | <0.05 | <0.05 | >0.05 | S |
| 10 mins | 88.7 ± 5.96 | 89.45 ± 5.32 | 89.6 ± 5.41 | <0.05 | <0.05 | >0.05 | S |
| 15 mins | 88.46 ± 5.68 | 89.46 ±5.31 | 89.16 ± 5.33 | >0.05 | >0.05 | >0.05 | NS |
| 20 mins | 88.9 ± 5.07 | 89.83 ± 4.67 | 89.1 ± 5.02 | >0.05 | >0.05 | >0.05 | NS |
| 25 mins | 89.43 ± 6.1 | 88.43 ± 5.58 | 88.83 ± 4.61 | >0.05 | >0.05 | >0.05 | NS |
| 30 mins | 91.5 ± 4.82 | 89.13 ± 4.48 | 88.5 ± 4.98 | >0.05 | >0.05 | >0.05 | NS |
| 60 mins | 92.14 ± 4.22 | 88 ± 4.77 | 91.33 ± 5.23 | >0.05 | >0.05 | >0.05 | NS |
Table 3: Comparisons of mean arterial pressure at different time interval.
When compared with individual group there was no statistical significance for means of mean Arterial pressure when Group A and Group F were compared at any time [5].
When compared to individual group there was statistical significance between Group A and Group M, Group F and Group M in mean of Mean Arterial pressure after intubation, at 30 seconds, 1 minute, 3 minutes, 5 minutes, 10 minutes with a P-value<0.05. When compared to individual group there was no statistical significance between Group A and Group M, Group F and Group M in mean of Mean Arterial pressure before premedication, at 15 minutes, 20 minute, 25 minutes, 30 minutes, 60 minutes with a P-value>0.05. Port instillation done with Inj Lignocaine 1% 10 cc, Bupivacaine 0.25% 10 cc, Tramadol 50 mg and Magnesium Sulphate 50 mg via all 3 ports, mean duration of analgesia is 7 hr [6].
Maharaj et al. conducted a randomized trial One hundred and six consecutive ASA I-III morbidly obese patients undergoing surgery were randomized to intubation with the Macintosh laryngoscope or the AirTraQ laryngoscope. If tracheal intubation failed within 120 s with the Macintosh or AirTraQ, laryngoscopes were switched. Success rate, SpO2, duration of tracheal intubation, and quality of airway management were evaluated and compared between the groups. Comparing Macintosh and AirTraQ laryngoscopes for tracheal intubation of morbidly obese patient found that the AirTraQ laryngoscope shorten the duration of tracheal intubation, prevented reduction in arterial oxygen saturation in morbidly obese patient [7].
A prospective randomized comparison of the LMA Fastrach, AirTraQ laryngoscope, and Glide Scope used for face-to-face tracheal intubation simulated to mimic an entrapped patient [8]. Thirty senior emergency medicine physicians were trained in the use of the LMA Fastrach, Glideslope, and AirTraQ laryngoscope with a standard airway trainer manikin (control). Participants were then asked to perform tracheal intubation in two difficult situations simulated on a difficult airway management manikin wearing a cervical collar [9]. In Situation 1, the manikin was in the supine position with a difficult airway caused by stiffening the cervical spine. In Situation 2, the manikin was positioned to simulate face-to-face tracheal intubation. We measured intubation times, success rates for tracheal intubation, and the difficulty of tracheal intubation. In control and Situation 1, tracheal intubation details were similar. In Situation 2, face-to-face tracheal intubation success rate was increased with the AirTraQ (100%), when compared with that of the GlideScope (70%, P<0.05) and LMA Fastrach (83%, P<0.05). Face-to-face tracheal intubation was less difficult (visual analogue scale: 0-100) with the AirTraQ 11 [10]. When compared with the GlideScope [33 (14) s, P<0.01)] and LMA Fastrach [22 (21) s, P<0.01]. The face-to-face tracheal intubation time was shorter with the AirTraQ 14 (6) s than with the GlideScope [27 (18) s, P<0.01] and Fastrach [28 (10) s, P<0.01]. The AirTraQ laryngoscope was superior to both the GlideScope and LMA Fastrach during simulated face-to-face difficult tracheal intubation [10].
A Sastre study to evaluate the success rate of blind intubations using two supraglottic devices, the Fastrach ILMA and the i-gel mask. A total of 80 patients (40 per group) were included [11]. After positioning them a leak test was performed, the glottis view was checked with a fibrobronchoscope, and an attempt was made to introduce an endotracheal tube through the device, and the procedure was repeated. Adequate ventilation was evaluated, as well as the grade of fibrobronchoscope view, the success of the intubation, and the complications observed after their use. There were no differences in the incidence of adequate ventilation with either device. The glottis view (Brimacombe scale) was better with i-gel (77.78% versus 68.42%) at the second attempt, but not on the first. A higher percentage of intubations were achieved with the Fastrach ILMA (70% versus 40%; P=013). The incidence of throat pain was similar with both devices, but post-operative dysphonia was more frequent with i-gel (20% versus 0; P=0053). Both devices were equally effective in achieving adequate ventilation; however, the Fastrach ILMA enabled a higher number of intubations to be made than i-gel and with a lower incidence of post-operative dysphonia [12].
The compared devices Aitraq, glidescope and FastracH in 120 patients. 40 patients divided into 3 groups. They concluded that AirTraQ device provided faster insertion and intubation times and enabled better Cormack-Lehane grades. Additionally, the AirTraQ device required the minimum number of optimization maneuvers and was associated with fewer complications and fewer intubation attempts than the Glidescope and Fastrach devices during face-to-face tracheal intubation [13].
Fastrach LMA and AirTraQ video laryngoscopes are boon for management of difficult airway in patients, but for that expertise skill is required which can be obtained after using the AirTraQ in patients with normal airway. From the present study it is concluded that Airtaq video laryngoscope and Fastrach intubating LMA, newer airway devices, is more user friendly, simple, easy to use as compared to conventional Macintosh laryngoscope. Patients with predicted difficult airway it should be kept ready to use in difficult airway cart and this video laryngoscope device are also included in difficult airway algorithm 2013, as recommended by ASA, further more clinical studies are suggested for better evaluation and comparison of conventional technique of endotracheal intubation with newer airway devices.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Gohil T (2022) Comparison of Intubation Criteria for Different Laryngoscopes-Macintosh Laryngoscope, Airtraq Video Laryngocope and Fastrach Laryngeal Mask Airway in Laparoscopic Surgery. J Anesth Clin Res. 13: 1083.
Received: 16-Aug-2022, Manuscript No. JACR-22-19319; Editor assigned: 22-Aug-2022, Pre QC No. JACR-22-19319 (PQ); Reviewed: 06-Sep-2022, QC No. JACR-22-19319; Revised: 13-Sep-2022, Manuscript No. JACR-22-19319 (R); Published: 20-Sep-2022 , DOI: 10.35248/2155-6148.22.13.1083
Copyright: © 2022 Gohil T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.