
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2023)Volume 14, Issue 5
Objective: Post-operative pain after modified radical mastectomy ranges from moderate to severe. Pectoralis (PECS) block has been found to be more effective than Erector Spinae Pain block in reducing pain and the consumption of analgesia in the post-operative period. This study aimed to compare the effect of ESP and PECS block on the quality of recovery after modified radical mastectomy with different dosage of drugs and different time of giving blocks.
Methods: The randomized controlled study was conducted at Indira Gandhi Medical College, Shimla, India, from March 2019 to March 2020. Patients were given blocks according to the computer-generated randomisation 30 minutes before shifting to the operation theatre. Group A received ESP block and group B received modified PEC block. Patient VAS score, NRS score and demand of rescue analgesia with patient satisfaction was recorded for 48 hrs post-operatively.
Results: A total of 60 patients were included (30 in each group). In the post-operative period, the mean VAS scores were statistically significant at 4, 8 and 24 hours postoperatively between the two groups with significantly lower VAS scores in Group A than in Group B. The total requirement of rescue analgesic was significantly lower in the ESP group than in the PECS group with p value 0.0154(<0.05). The time to first rescue analgesia was significantly higher in the ESP group (11.21 ± 3.14) hours than in the PECS group (6.15 ± 3.52) hours.
Conclusion: Both ESP and PECS block were effective in improving the VAS score and in reducing the consumption of rescue analgesia after modified radical mastectomy.
Cancer; Mastectomy; Post-operative pain; Post-operative recovery; PECS block; ESP block
Breast cancer is the most commonly occurring cancer in women worldwide and the second-most common cancer in India [1,2]. Modified Radical Mastectomy (MRM) is a common surgical modality performed under general anesthesia, however, practitioners are showing more interest towards regional anesthesia for MRM surgeries these days for better intraoperative stability and less postoperative complications [3]. Despite the latest advances in breast cancer surgery, MRM is frequently associated with postoperative pain, nausea and vomiting. The beneficial effects of regional blocks are peri-operative analgesia along with decrease incidence of post-operative nausea and vomiting also [4]. Acute postoperative pain is an integral risk factor in the development of chronic postmastectomy pain [5,6]. The Pectoral nerve (PEC) block and Erector Spinae Plane (ESP) block are both inter-fascial plane block described in breast surgery both as analgesic and anesthetic technique [7]. ESP provides multi-dermatomal sensory block across posterior, anterior and lateral thoracic wall [8].
Till date there have been very few studies regarding the efficacy of erector spinae plane block in MRM and the comparative efficacies of PEC and erector spinae blocks. Considering these facts, we have conducted a study on the comparative efficacy of ultrasound guided PEC vs. ESP blocks on postoperative analgesia in patients undergoing MRM.
After the approval of the research and ethics committee of the institution Indira Gandhi Medical College, and registered under Clinical Trials Registry India with CTRI registration CTRI/2019/12/022287 and written informed consents obtained from the patients. The proposed study was carried out in American Society of Anesthesiologists (ASA I and ASA II) patients, aged between 18 and 65 years, undergoing modified radical mastectomy at Indira Gandhi Medical College, Shimla from March 2019 to March 2020. The study was conducted in a controlled prospective randomized manner based on the 2010 Consolidated Standards of Reporting Trials (CONSORT) guidelines. After enrolment, the participants were randomly allocated to either the ESP group (Group A, n=30) or the PECS group (Group B, n=30). On the day of the surgery, a previously prepared and sealed opaque envelope containing the random group assignment was opened by research assistant who was not involved in this study. The group allocation was then conveyed to the block practitioner before block performance. To eliminate performance bias, all blocks were performed by experienced regional anesthesiologists. All anesthesiologists in charge of intraoperative anesthesia management, outcome assessors, patients and follow-up personnel were blinded to group allocation. Group A received USG guided Erector Spinae plane block and Group B received USG guided Pectoral Nerve block with 30 ml of 0.25% of bupivacaine each.
The patients were instructed on the use of the Visual Analogue Scale (VAS 0-10; 0 for no pain and 10 for worst pain). After routine pre-anesthetic check up with routine premedication, the patients were shifted to pre-operative preparatory room. The patients were connected to standard ASA monitors, which included non-invasive cuff blood pressure, pulse oxygen saturation, and 5-lead electrocardiography measurements. An 18-gauge or 20-gauge intravenous cannula for fluid infusion was placed in the contralateral forearm, and premedication (IV midazolam 2 mg and IV Fentanyl 0.5 μg/kg) was administered for anxiolytic effect before the block procedure. The patients received either PEC or ESP block 30 minutes prior to the surgery according to randomization.
With patients in sitting position depending on the surgical side, left- or right-sided ESP block shown in Figures 1 and 2 was given using a high-frequency linear USG transducer. The probe was placed in longitudinal orientation 2.5 cm lateral to the thoracic fifth spinous process. The trapezius, rhomboid major and erector spinae muscles were identified from the surface. A 22-gauge spinal needle was inserted in a cephalad-to-caudad direction until the tip lay in the interfacial plane between rhomboid major and erector spinae muscles, as evidenced by visible linear spread of fluid between the muscles upon injection. 30 ml of 0.25% bupivacaine was deposited into this interfacial plane. After checking for sensory dermatome from 2nd thoracic vertebrae to 8th thoracic vertebrae. general anesthesia is to be administered (Figure 2).
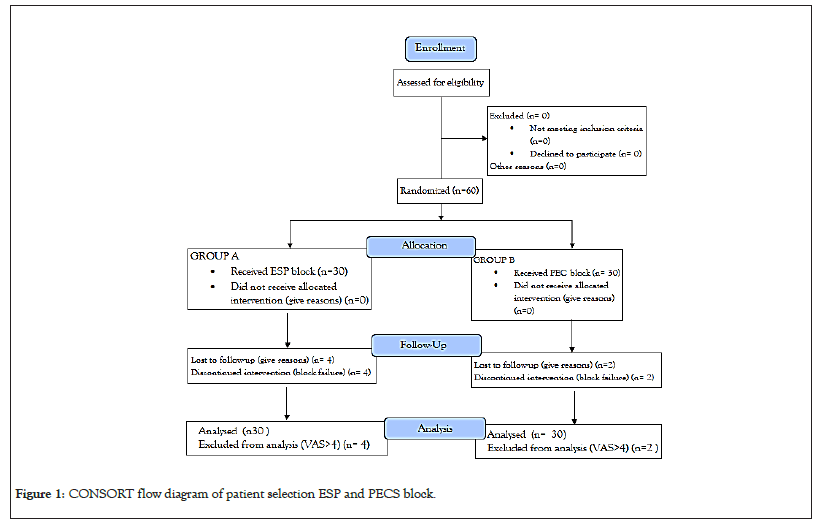
Figure 1: CONSORT flow diagram of patient selection ESP and PECS block.
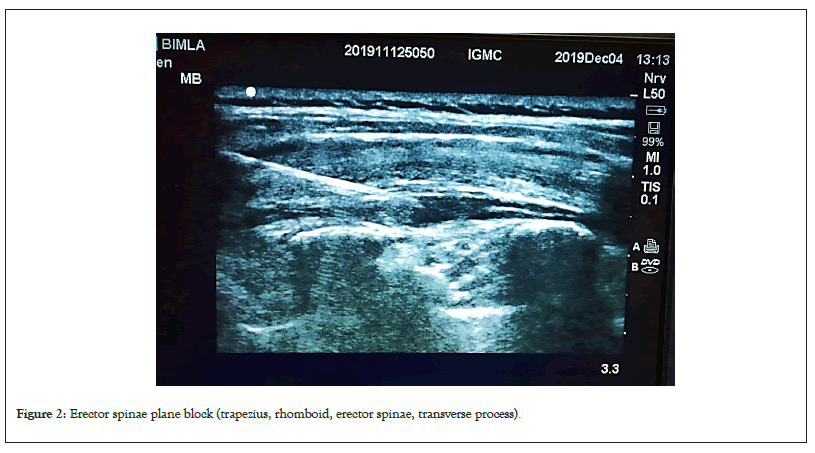
Figure 2: Erector spinae plane block (trapezius, rhomboid, erector spinae, transverse process).
Ultrasound guided (USG) Pecs block showed in Figure 3 was given with patient in supine position by placing the ipsilateral upper limb in abducted position, using a linear USG probe of high frequency (6-13 MHz, Sonosite). The USG probe was placed at the infraclavicular region where pectoralis minor and pectoralis major muscles were identified, 22 Gauge spinal needle was inserted in plane with the USG probe to the fascial plane between pectoralis muscles and 10 ml of total drug was injected. The USG probe was moved towards axilla till serratus anterior muscle was identified and the needle was then reinserted into the fascial plane between pectoralis minor and serratus anterior and 20 ml of the remaining drug was injected (Figure 3).
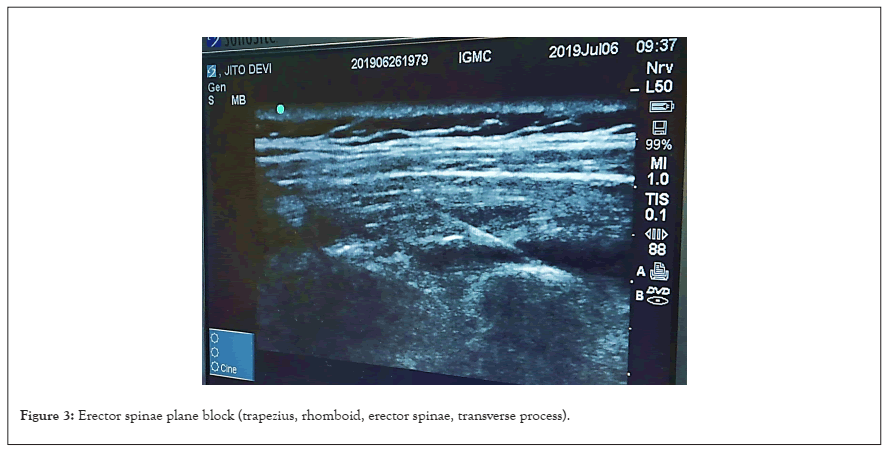
Figure 3: Erector spinae plane block (trapezius, rhomboid, erector spinae, transverse process).
After 30 minutes, patients were shifted to the O.T. and all the patients were subjected to routine intra-operative monitoring. General anesthesia was given by Injection (Inj) fentanyl 2 μg/kg Intravenous (IV) and Inj propofol 2 mg/kg IV and intubation was facilitated with Inj succinylcholine 2 mg/kg IV. Anesthesia was maintained with isoflurane 0.2%-2% and N2O and O2 mixture (66% and 33%). Neuromuscular blockade was achieved with Inj atracurium 0.5 mg/kg IV initially and then maintained with 0.01 mg/kg. Inj ondansetron 4 mg IV was given.
Throughout the surgery, non-invasive mean arterial blood pressure, heart rate and oxygen saturation was monitored continuously and recorded every 5 minutes till the completion of the procedure. Inj fentanyl 1 μg/kg IV in bolus doses were given to the patients when Mean Arterial Pressure (MAP) or heart rate exceeded 20% above the preoperative value. After completion of surgery neuromuscular blockade was reversed with iv neostigmine 50 μg/kg and glycopyrrolate 10 μg/kg.
Primary outcome
After surgery, patients were shifted to the recovery room or Post Anesthesia Care Unit (PACU). The level of postoperative pain was assessed at 0 min (on being shifted to recovery), 30 mins and 60 mins in PACU and at 2 hrs, 4 hrs, 8 hrs, 24 hrs and 48 hrs postoperatively in ward by VAS scores. Whenever the VAS score was >4 rescue analgesic was given with Inj. tramadol 50 mg iv and if the pain persisted/reappeared within 8 hours, Inj diclofenac 75 mg iv was given. Amount of doses of Injection diclofenac and Injection tramadol were recorded.
Secondary outcome
The level of postoperative nausea and vomiting was assessed with the Numerical Rating Scale (NRS 0-4): (0-no nausea, 1-nausea, 2-retching, 3-vomiting and 4-severe vomiting). Inj Ondansetron 4 mg IV was given as an antiemetic. Patients were also monitored for any post-operative complications like pneumothorax, haematomas, intravascular injections. Patient satisfaction ratings were also recorded and assessed using (4-totally satisfied and 0-not at all satisfied). The research assistant also recorded demographic data, including type of surgery; surgical duration (defined as the interval from skin incision to closure) and propofol consumption.
Sample size calculation and statistical calculation
We expected that a satisfactory percentage of patients receiving ESP and PECS block would have complete satisfaction regarding pain control. Therefore, we conducted a pilot study with 10 patients per group, none of which were included in this study. We calculated the sample size of 60 patients total to provide statistical power of 0.80 and one sided 97.5% CI. The data of the study was recorded in the record charts and the results were evaluated using statistical tests (ANOVA, Chi-square, Mann-Whitney Test, Post-hoc test) as applicable. P-value>0.05 was taken as not significant, while p<0.05 was considered significant.
The present study was conducted in a randomized double blind control manner in the Department of Anesthesiology, IGMC, and Shimla in ASA I and ASA II patients posted for Modified Radical Mastectomy. The patients in group A were given ultrasound guided Erector spinae plane block with 30 ml of 0.25% bupivacaine while the patients in group B were given ultrasound guided Pec I with 10 ml of 0.25% bupivacaine and Pec II block with 20 ml of 0.25% bupivacaine, 30 minutes prior to induction of general anesthesia.
Four patients from group A and 2 patients of group B complained of pain with VAS>4 in the PACU and received a rescue analgesic in the immediate post-operative period. Hence these patients were excluded from the study and considered as block failures.
All the data was selected randomly and tabulated, and then analysed with appropriate statistical tools “SPSS version 21”. Data was presented as mean with standard deviation or proportions as appropriate. Mean, median, standard deviation and variance was calculated and following statistical significance tests were applied.
1. Student’s paired T-test was used as the statistical tool as test for significance of observed mean differences.
2. Statistical analysis was done using “Chi-square Test”.
3. Composite scores were assessed by using “Wilcoxon Signed rank test”.
Finally, the calculated values were compared with the tabulated values at a particular degree of freedom and the level of significance was determined. A “p-value” was considered to be non-significant if p>0.05 and significant if p<0.05.
The following observations were made
The demographic data and baseline parameters with respect to HR, MAP and SPO2 were found to be comparable between the two groups (Figure 4).
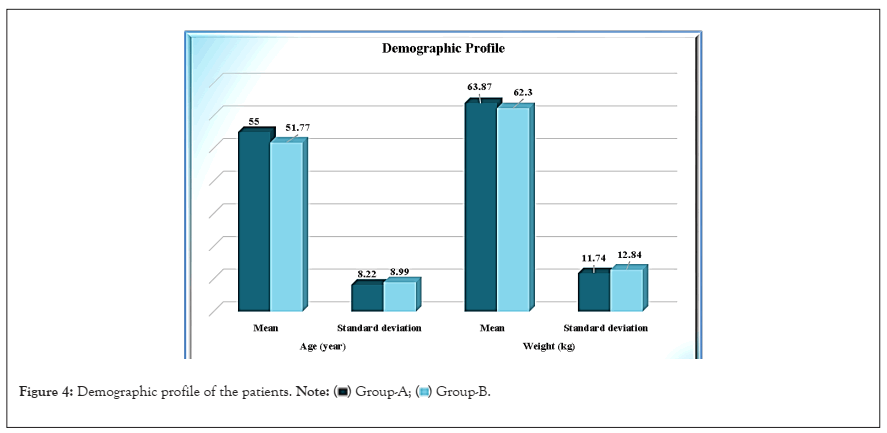
Figure 4: Demographic profile of the patients. 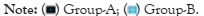
The difference in other intra-operative and post-operative vitals with respect to HR, MAP and SPO2 of the patients between two study groups was not statistically significant (Figure 5).
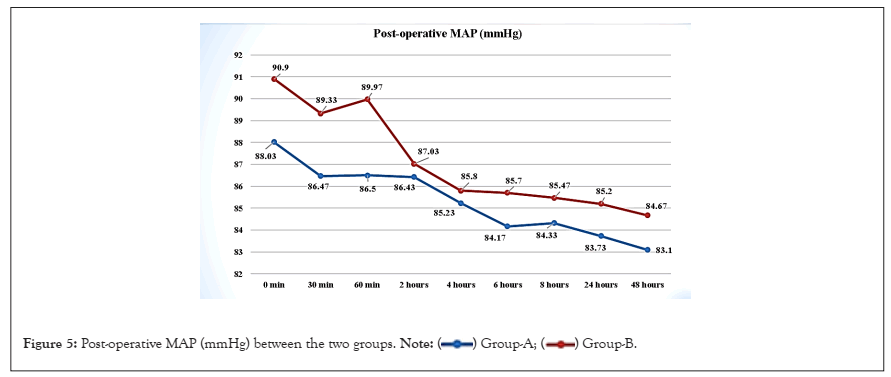
Figure 5: Post-operative MAP (mmHg) between the two groups. 
The post-operative VAS scores was not significant statistically for first 2 hours. The mean VAS score at 4 hours postoperatively in group A was 1.23 ± 1.19 while in group B was 3.07 ± 1.51 with a p value of <0.0001 which was statistically significant. The mean VAS score at 8 hours was 1.97 ± 1.07 in group A and 2.70 ± 1.49 in group B with a p value 0.0334 which was also statistically significant. The mean VAS values in Group B at 8 hours remained less than that recorded at 4 hours because many patients received doses of rescue analgesic by 8 hours postoperatively though it remained significantly greater as compared to the mean VAS scores recorded in group A during the same time intervals (Figure 6 and Table 1).
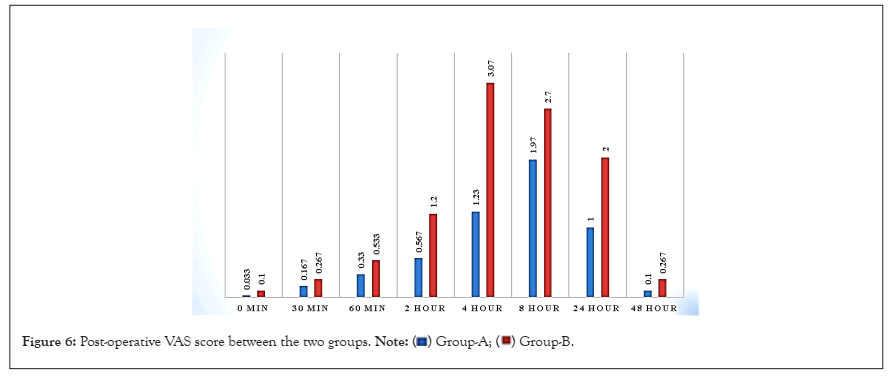
Figure 6: Post-operative VAS score between the two groups. 
| VAS | Group-A (n=30) | Group-B (n=30) | tcal | P value | Results |
|---|---|---|---|---|---|
| 0 min | 0.033 ± 0.18 | 0.10 ± 0.402 | 0.833 | 0.4082 | Not Significant |
| 30 min | 0.167 ± 0.461 | 0.267 ± 0.739 | 0.629 | 0.5319 | Not Significant |
| 60 min | 0.330 ± 0.596 | 0.533 ± 0.899 | 1.183 | 0.5416 | Not Significant |
| 2 hour | 0.567 ± 1.194 | 1.2 ± 1.584 | 1.748 | 0.0858 | Not Significant |
| 4 hour | 1.23 ± 1.19 | 3.07 ± 1.51 | 5.242 | <0.0001 | Significant |
| 8 hour | 1.97 ± 1.07 | 2.70 ± 1.49 | 2.18 | 0.0334 | Significant |
| 24 hour | 1.00 ± 0.69 | 2.00 ± 1.36 | 3.592 | 0.0007 | Significant |
| 48 hour | 0.1 ± 0.402 | 0.267 ± 0.583 | 1.292 | 0.2016 | Not Significant |
Table 1: Postoperative Visual Analogue Scores (VSA).
At 24 hours postoperatively, mean VAS score in group A was 1.00 ± 0.69 and in group B was 2.00 ± 1.36 with p value of 0.0007 which was statistically significant.
Mean NRS score postoperatively was found to be statistically insignificant when compared between the two study groups, (p>0.05) except for at 4 hours with mean NRS score of 0.100 ± 0.305 in group A and 2.03 ± 1.63 in group B with P value <0.0001 of which was statistically significant.
The mean time of 1st analgesic required in group A and group B was 11.21 ± 3.14 and 6.15 ± 3.52 hours respectively. The difference was statistically significant between group A and group B with p value (p<0.0001) (Table 2).
| Duration ( in hours) | Group-A (n=14) | Group-B (n=26) | tcal | P value | Results |
|---|---|---|---|---|---|
| Mean ± standard deviation | 11.21 ± 3.14 | 6.15 ± 3.52 | 4.496 | <0.0001 | Significant |
Table 2: Time of 1st analgesic required between two groups (duration of analgesia provided by block).
There was statistically significant difference in the number of patients receiving Rescue Analgesic between the two groups, with a p-value of 0.0154 (p<0.05) using the Chi-square Test (χ²-Test) (Figure 7).
Figure 7: Total rescue analgesic between the two groups. 
The requirement of antiemetic was found to be statistically significant between the two groups with p-value=0.0462 (p<0.05). “Chi-square Test (χ²-Test)” was used with χ² cal=3.976 (at 95% confidence limit, with degree of freedom 1, χ² tab=3.841) χ2 cal<χ² tab (3.976>3.841) at 5% level of significance.
Also there was a statistically significant difference between the two groups according to the difficulty encountered during the block with p value=0.0238 (p<0.05). The difficulty in recognizing the sonoanatomy during the block was found to be correlated to the breast size and weight of the patient.
There was a statistically significant difference between the two groups according to the level of patient satisfaction, with p value=0.0483 (p<0.05). Group A patients are more satisfied than group B (Figure 8).
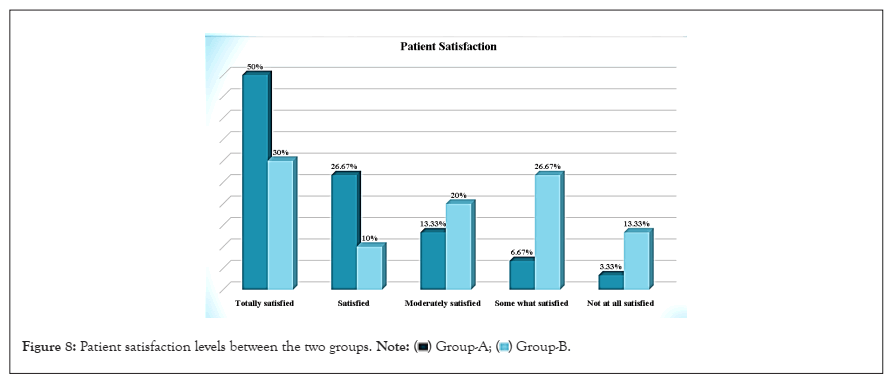
Figure 8: Patient satisfaction levels between the two groups. 
Breast cancer is the second most common cancer in India and MRM is the commonest surgery performed under general and regional anesthesia [9].
Regional anesthesia result in decrease in post-operative complications9 and may also reduce cancer progression by attenuation of the surgical stress response, better analgesia, and reduced opioid usage, and by the direct protective action of local anesthetics on cancer cells migration [10].
Lynch et al., and Lahiry et al., had observed that thoracic epidural anesthesia resulted in improvement in Visual Analogue Scores (VAS), which resulted in less incidence of PONV and less hospital stay [11,12].
Thoracic paravertebral block is considered the “gold standard” regional anesthesia technique but reported to be inadequate block for axillary clearance [13-16].
After understanding the neural supply of chest wall and breast, modified PEC block markedly improves the quality of postoperative recovery for patients while minimising the risk of complications associated with epidural and paravertebral blocks [17-19].
Erector Spinae plane block anaesthetized the anterior and posterior chest wall, axilla and medial aspect of upper arm by targeting the dorsal and ventral rami of spinal nerve roots [8,20]. It resulted in significant reduction in postoperative VAS and NRS pain scores along with less consumption of rescue analgesic proving it to be a promising technique in the context of surgical pain during radical mastectomy.
Our present study was conducted in a randomized double blind control manner to compare the benefits and difficulties encountered between two blocks both modified PEC and ESP for modified radical mastectomy.
The VAS score in post-operative period was observed for 48 hrs and it was found that ESP block was more effective as analgesic for long duration as compare to modified PEC block. The difference in the VAS score between two groups was found to be statistically significant till 24 hrs. In contrast the study conducted by Gad M et al., VAS score showed no significant difference between the two studied groups however E group (ESP) recorded significantly higher values at all other time points compared with P group (PEC) [20]. This may be due to the timing of the given block (given post induction in comparison to our study where the block was given 30 minutes pre induction) and due to the volume of drug given (20 ml of 0.25% bupivacaine).
It was also observed that the duration of analgesia was prolonged in ESP block in comparison to PEC block and the demand of first dose of rescue analgesia was delayed in ESP block.
The study conducted by Sinha et al., that mean duration of analgesia and demand of rescue analgesia was delayed in PEC group as compare to ESP group which was contrary to our study [21]. This may be probably due to variation as well as due to volume of the drug used. In the study conducted by Yao et al., it was found that the ESP block improves the pain QoR score in the post-operative period [22].
There was a statistically significant difference between the two groups according to the difficulty encountered during the block procedure, with p value = 0.0238 (p<0.05). The difficulty in recognizing the sonoanatomy during the block was found to be correlated to the breast size, volume of breast tissue and the weight of the patient. ESP block was found to be relatively easier to perform than PEC block.
There was a statistically significant difference between the two groups according to the level of patient satisfaction, with p value = 0.0483 (p<0.05) Group A patients were more satisfied than group B.
The limitation of our study was that the ESP block was new to us and hence more number of block failures were noted, i.e. 4 in ESP block, compared to 2 in PEC block. Secondly the dissatisfaction due to needle prick during block performance can be overcome by performing blocks after induction of general anesthesia. It is convenient to perform modified PEC block under general anesthesia. On the other hand, positioning for ESP block can be a challenge after induction of anesthesia and requires a dedicated team of operating room personnel for positioning only. Thirdly, the patients were not blinded. Block was given before general anesthesia to assess the level of sensory block in awake patients.
From our study we concluded that both PEC and ESP blocks can be used to provide postoperative analgesia with stable intraoperative haemodynamic with no complications, in MRM surgeries. However, ESP as compared to the PEC block has lower VAS scores, lesser demands for rescue analgesia and prolonged duration of analgesia with reduced incidence of PONV. Both ESP and PECS block were effective in improving the VAS score and in reducing the consumption of rescue analgesia after modified radical mastectomy. ESP is simpler, easy to perform and provides better patient satisfaction without causing any noticeable side effects.
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
[Google Scholar] [Crossref] [PubMed]
Citation: Bhattacharya S, Mahajan S, Sood A (2023) Comparison of Postoperative Analgesic Effect of Ultrasound Guided Pectoral vs. Erector Spinae Block in Patients Undergoing Modified Radical Mastectomy: A Randomised Controlled Study. J Anesth Clin Res. 14:1114.
Received: 06-Oct-2023, Manuscript No. JACR-23-27363; Editor assigned: 09-Oct-2023, Pre QC No. JACR-23-27363 (PQ); Reviewed: 24-Oct-2023, QC No. JACR-23-27363; Revised: 31-Oct-2023, Manuscript No. JACR-23-27363 (R); Published: 07-Nov-2023 , DOI: 10.35248/2155-6148.23.14.1114
Copyright: © 2023 Bhattacharya S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.