Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2020)Volume 11, Issue 4
Objective: To evaluate the accuracy of three calculation formulas of intraocular lens (IOL) on the refractive state of cataract patients with high myopia after cataract surgery, to study the influence of three formulas on axial length (AL), and to verify the advantage of Olsen formula over SRK/T and Haigis formula in predicting postoperative refraction in patients with high myopia and cataract, so as to provide a basis for selecting the degree of IOL in cataract patients with high myopia, so as to provide a basis for selecting the degree of IOL in cataract patients with high myopia. Methods We collected the data of sex, age, axial length, predicted value of SRK/T, Haigis, Olsen formula and postoperative true diopter of 101eyes of 10z eyes hospitalized in the First Affiliated Hospital of Guangzhou University of Chinese Medicine from 2016-10-10 to 2019-8-20. 101 cases were divided into three groups according to the AL. The prediction accuracy of the three formulas for different eye axis length was evaluated respectively,and the stability of the same formula for the prediction of different axial lengths was compared. Results Within the range of 26mm
High myopia; Cataracts; Calculation formula of intraocular
High myopia and its complications are one of the eye diseases that seriously threaten human vision [1-3]. Among several complications, high myopia with cataract is one of the main diseases causing blindness. Epidemiological surveys show that the prevalence rate of high myopia is 0.53% in central India [4], 2.7% in Europe [5], and 8.4% in Singapore, and the prevalence rate of high myopia of ethnic Chinese is significantly higher than that of Malays and Indians [6]. At present, the main treatment of high myopia with cataract is phacoemulsification combined with intraocular lens implantation. Studies have proved that the commonly used clinical formulas such as SRK/T and Haigis formula can not accurately predict the postoperative diopter of patients [7], and there is a common phenomenon of hyperopia drift after surgery [8]. As the representative of the fifth generation intraocular lens power calculation formula, Olsen formula can predict the effective position of intraocular lens by preoperative anterior chamber depth and lens thickness, which is expected to provide more accurate prediction of postoperative refractive state for cataract with high myopia [9]. In this study, through the comparison of three formulas of SRK/T, Haigis and Olsen in different eye axial length(AL), to evaluate the accuracy and stability of the three formulas in the prediction of postoperative diopter in patients with high myopia and cataract, and to provide a reliable basis for the selection of clinical intraocular lens diopter. The results are reported as follows.
Ethical approval
This is a retrospective study of cataract patients with high myopia hospitalized in the First Affiliated Hospital of Guangzhou University of Chinese Medicine from 2016-10-10 to 2019-8-20. A total of 101 eyes were found in 65 cases, including 21 males (29 eyes) and 44 females (72 eyes). The age was 41 to 82 years old. The Ethics Committee at First Affiliated Hospital of Guangzhou University of Chinese Medicine ruled that approval was not required for this study.
Inclusion criteria
• Patients accord with the diagnostic criteria of high myopia (diopter-6.0D, AL26mm)
• Patients accord with the diagnostic criteria of cataract in the third edition of Ophthalmology of the People's Health Publishing House
• Patients have complete case data
• Patients whose routine ophthalmology examination was completed and phacoemulsification combined with intraocular lens implantation was performed were included
• There were no other eyeball diseases affecting eyesight.
Exclusion criteria
• Patients with traumatic cataract or congenital cataract were excluded
• Patients with a history of ocular surgery except cataract surgery were excluded
• Patients wtih rupture of posterior capsule or postoperative high intraocular pressure or intraocular inflammation caused by operation
• Patients whose visual acuity, refraction, axial length and corneal curvature could not be measured were excluded.
Grouping
The patients were divided into three groups according to the AL. The Criteria was28mm, 28mm30mm, 30mm respectively. They were named group A, B, C respectively.
Routine preoperative examinations
Routine preoperative examinations include slit lamp examination, ultrasound biometrics (Aviso A/B, Quantel Medical), corneal topography (Pentacam HR, version 1.21r18, Oculus Optikgerate GmbH), intraocular pressure (TX-10 noncontact tonometry) and corneal endothelium calculation (EM-3000).
Mean absolute error
The axial length (AL), central corneal thickness ( CCT), anterior chamber depth (ACD), lens thickness (LT) and astigmatism ( Ast) were collected by HAAG-STREIT LS900 IOL-master in all patients. The theoretical diopter of SRK/T, Haigis and Olsen formula after lens implantation was calculated by using the formula calculation software of the machine. Three months after operation, all patients underwent computer optometry with TOPCON KR-800 computerized keratometer. Based on the values measured by the optometer, refractive examination was performed with lens insertion, and the postoperative refractive status was recorded. MAE is equal to the absolute value of the difference between the reserved diopter and the actual postoperative diopter.
Operation
All patients underwent phacoemulsification combined with intraocular lens implantation by the same physician. Preoperative compound tropicamide eye drops fully dilated the pupil, the operation area was fully disinfected, the eye drops were anesthetized with promevacaine hydrochloride, the keratoscleral margin made about 2.8mm incision, continuous circular capsulorhexis, water separation, delamination, cataract phacoemulsification, implantation of appropriate degrees of intraocular lens in the capsule bag, watertight incision, postoperative application of tobramycin dexamethasone eye ointment to prevent infection, aseptic dressing wrapped, The patients were followed up for 3 months.
Statistical analysis
SPSS 22.0 was used for statistical analysis. The MAE of the three formulas under different eye axis length were collected. the Dunnett analysis was used to compare the different eye axis length of the same formula, the one-way ANOVA was used to compare the different formulas under the same eye axis length, and the least significant difference (LSD) method was used in the pairwise test. The Bland-Altman diagram was made by Medcalc software to compare the prediction consistency of different formulas. The percentages of MAE between ±0.5D, ±1.0D and ±2.0D were calculated. P0.05 was considered to be statistically significant difference.
Basic data and preoperative biological parameters of patients
The data are shown in Table 1, and a total of 101 cases are included. According to the difference of AL, the subjects were divided into three groups. The general data and the biological parameters of eyeball before operation of the patients were collected.
| Axial length (mm) | All |
|||
|---|---|---|---|---|
| 2628 | 2830 | 30 |
||
| Enrolled subjects(n) | 29 | 41 | 31 | 101 |
| Gender, n(%) | ||||
| Male | 931.03 | 1331.71 | 722.58 | 2928.71 |
| Female | 2068.97 | 2868.29 | 2477.42 | 7271.29 |
| Age (y) | ||||
| Mean ±SD | 64.62±8.71 | 63.22±8.71 | 61.87±8.36 | 63.21±8.58 |
| Range | 5282 | 4182 | 4482 | 4182 |
| Anterior chamber depth (mm) | ||||
| Mean ±SD | 3.48±0.49 | 3.71±0.65 | 3.40±0.36 | 3.55±0.54 |
| Range | 2.524.99 | 2.826.67 | 2.424.01 | 2.426.67 |
| IOL power (D) | ||||
| Mean ±SD | 9.52±2.98 | 4.35±2.63 | 1.24±3.19 | 4.88±4.33 |
| Range | 313 | -19 | -5.57 | -5.513 |
Table 1: Basic data and preoperative biological parameters of patients in the group.
Analysis of MAE of three calculating formulas for the diopter of intraocular lens
The comparison of MAE of the three calculation formulas of intraocular lenses with different ocular axis length is shown in Table 2. It can be seen that with the increase of the eye axis length, the MAE of three calculation formulas increases gradually, suggesting that the prediction accuracy of the three formulas decreases with the increase of the eye axis length. In the lateral comparison of the same eye axis length, in the three groups respectively and as a whole, the refractive error was SRK/T Haigis Olsen.
| Axial length | (n) | SRK/T | Haigis | Olsen |
|---|---|---|---|---|
| 26mmAL≤28mm | 29 | 0.31±0.19 | 0.28±0.16 | 0.16±0.15 |
| 28mmAL≤30mm | 41 | 0.54±0.35 | 0.45±0.34 | 0.25±0.25 |
| AL30mm | 31 | 0.99±0.52 | 0.68±0.54 | 0.36±0.41 |
| All | 101 | 0.61±0.46 | 0.47±0.41 | 0.26±0.30 |
Table 2: Three formulas for calculating the diopter of intraocular lens MAE.
Figure 1 shows the MAE changes of three intraocular lens calculation formulas at different axial lengths. It can be seen intuitively from the figure that, similar to the results of Table 2, the accuracy of the three formulas decreases with the eye axis length, but the decrease of the accuracy of the three formulas are different. SRK/T is the most affected by the eye axis length, while Olsen has the least influence. In the range of each eye axis length, the performance of the prediction accuracy of Olsen is better than that of the other two.
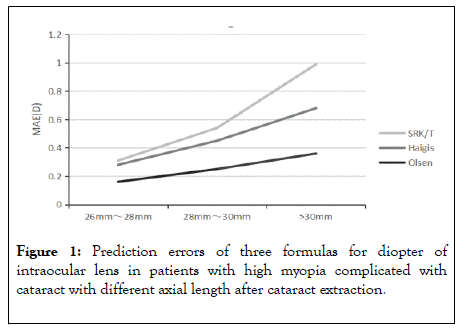
Figure 1: Prediction errors of three formulas for diopter of intraocular lens in patients with high myopia complicated with cataract with different axial length after cataract extraction.
Figure 2 shows the absolute error distribution of diopter predicted by three calculation formula. In terms of median, average and upper and lower quartile, the prediction accuracy of Olsen is significantly better than that of SRK/T and Haigis,. Within the range of 26mm AL 30 mm, there is no significant difference between SRK/T and Haigis. When AL 30mm, the stability of Haigis is significantly stronger than that of SRK/T, so it can be inferred that when AL 30mm, SRK/T is greatly affected by the length of eye axis.
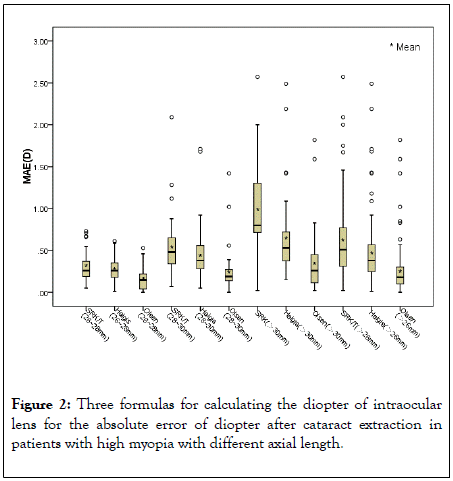
Figure 2: Three formulas for calculating the diopter of intraocular lens for the absolute error of diopter after cataract extraction in patients with high myopia with different axial length.
The MAE differences of the three formulas at different axial lengths are shown in Table 3. For SRK/T formula, 26mm AL 28 mm, 28mm AL 30 mm, AL 30mm had statistical significance (P0.05). For Haigis formula, 26mm AL 28 mm group had statistical significance compared with 28mm AL 30 mm, AL 30mm group respectively, but there was no significant difference between 28mm AL 30 mm and AL 30mm group. In Olsen formula, only 26mm AL 28 mm, AL 30mm had statistical significance, suggesting that the accuracy of Olsen prediction was least affected by eye axis length, while SRK/T was most affected.
| Eyes (n) | A-B | A-C | B-C | ||
|---|---|---|---|---|---|
| SRK/T | 101 | 0.003* | 0.000* | 0.000* | |
| Haigis | 101 | 0.016* | 0.001* | 0.078 | |
| Olsen | 101 | 0.216 | 0.040* | 0.398 | |
* Statistical significance; α=0.05
Table 3: Three formulas for calculating the diopter of intraocular lenses MAE difference of different eye axis length.
By analyzing the MAE of the three formulas for calculating the diopter of intraocular lenses (Table 4), it was found that within the range of 26mm AL 30mm, Olsen formula has statistical significance with SRK/T formula and Haigis formula (P0.05), but there was no significant difference between SRK/T and Haigis (P 0.05). When AL 30mm, the comparison of the three formulas was statistically significant respectively (P0.05).
| Axial length | Eyes (n) | SRK/T-Haigis | SRK/T-Olsen | Haigis- Olsen |
|---|---|---|---|---|
| 26mmAL≤28mm | 29 | 0.397 | 0.001* | 0.014* |
| 28mmAL≤30mm | 41 | 0.221 | 0.000* | 0.005* |
| AL30mm | 31 | 0.016* | 0.000* | 0.011* |
| All | 101 | 0.091 | 0.000* | 0.000* |
* Statistical significance; α=0.05
Table 4: MAE differences among three formulas for calculating the diopter of intraocular lens
Bland-altman diagram analysis the consistency between the predicted diopter by three calculation formulas and the actual diopter after cataract extraction in patients with high myopia complicated with cataract. The result is shown in Figure 3. The actual diopter is the closest to that predicted by Olsen formula and the least consistent with that predicted by SRK/T formula.
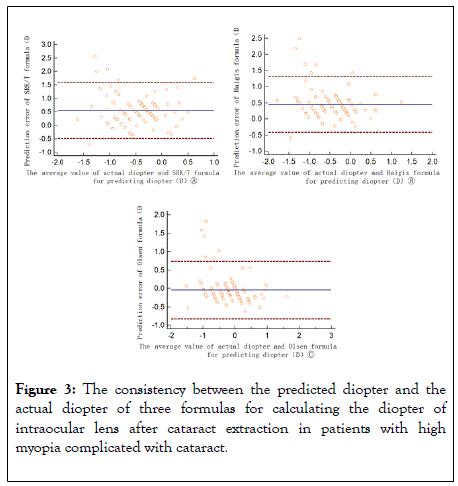
Figure 3: The consistency between the predicted diopter and the actual diopter of three formulas for calculating the diopter of intraocular lens after cataract extraction in patients with high myopia complicated with cataract.
By drawing the percentages of MAE in the range of 0.5D, 1.0D and 2.0D (Figure 4), Olsen was significantly better than the other two in the range of eye axis, and Haigis was better than SRK/T.
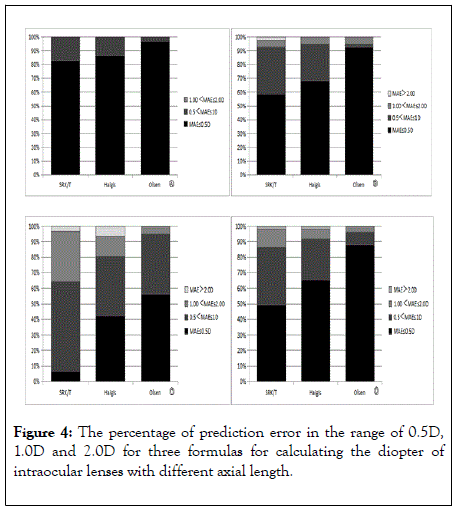
Figure 4: The percentage of prediction error in the range of 0.5D, 1.0D and 2.0D for three formulas for calculating the diopter of intraocular lenses with different axial length.
26mmAL≤28mm28mmAL≤30mmAL30mmAL26mm
Cataract surgery moves forward from the era of fuming to the era of refraction. Generally speaking, for ordinary cataract patients, ideal refractive effect can be achieved after surgery [6]. However, for cataract patients with high myopia, the third and fourth generation IOL diopter calculation formulas have some limitations, and with the extension of the axial length, the prediction accuracy is further reduced. In view of this, some scholars believe that when using the SRK/T /Haigis formula, the accuracy of the formula can be improved by individualizing the adjustment to the direction of myopia according to the needs of patients [9]. However, this not only tests the personal experience of doctors, but also does not meet the needs of modern medical accuracy.
At present, there is no unified conclusion on the formula for calculating the diopter of intraocular lens in cataract surgery for patients with high myopia complicated with cataract. The selection of appropriate calculation degree for different axial length and the preoperative prediction of reserved diopter mainly depend on the subjective experience of doctors and the actual needs of patients, and do not have universal standards and norms. We found that for the three groups of 26mmAL≤ 28mm, 28mmAL≤30mm, AL30mm, the prediction results of Olsen formula were closer to the real value than SRK/T and Haigis formula, which was consistent with the conclusion of Cooke [3]. However, there was no significant difference between SRK/T formula and Haigis formula in the range of 26mmAL≤30mm, and Haigis formula began to show superiority in prediction accuracy when AL30mm.By comparing the MAE of SRK/T formula in three groups of 26mmAL≤28mm, 28mmAL≤30mm, AL30mm, it was found that there were differences between each groups. Olsen formula performed best in this comparison, only 26mmAL≤28mm group and AL30mm group has different , suggesting that the accuracy of Olsen formula was least affected by axial lengths, while SRK/T formula was most affected by axial lengths. The reason for the analysis may be mainly related to the calculation method of each formula.At present, the formula for calculating the refraction of intraocular lens is mostly based on the theoretical formula of Gaussian optics, in which the third generation formula SRK/T belongs to the two-variable formula, and the prediction of the postoperative effective lens position (ELP) only depends on the axis length and corneal curvature [10], so the influence of the axis length is more obvious than the fourth and fifth generation formula, and the prediction accuracy of the long eye axis patients is lower.Although Haigis formula introduces predictive variables such as preoperative anterior chamber depth and horizontal corneal diameter on the basis of SRK/T formula [11], the prediction accuracy and stability of postoperative cataract patients with high myopia are better than the third generation formula [12], but the accuracy of prediction of ultra-long eye axis patients is still inadequate. Haigis [13] think that the geometric shape of intraocular lens changes greatly when it transfer from positive degree to negative degree, so for SRK/T and Haigis formula, the calculation of IOL degree of different degrees needs to be modified by different constants, which greatly affects the clinical practicability. The new generation of Olsen formula not only includes five variables: axial length, anterior chamber depth, corneal curvature, lens thickness and patient age, but also creatively puts forward a new concept of using C constant to predict ELP [14], which is helpful to improve the prediction accuracy of cataract patients with long axial.
Scholars from all over the world have been devoting themselves to the study of the formula for calculating the diopter of intraocular lens for many years. Hoffer [15] analyzed the study in the past 50 years and found that, Barrett Universal , Olsen, Haigis and SRK/T formula can be used to predict the postoperative diopter of patients with long eye axis, which is similar to the conclusion of other scholars [4,16-18]. However, some researchers have put forward different opinions. Chen [12] found that for SRK/T formula, when AL26mm, the increase of 1mm leads to an increase of 0.13D in the average absolute error of prediction, while for AL>33 mm, the increase of 1mm axis leads to an increase of 1.15D in the average absolute error of prediction.By analyzing the influence of Haigis, SRK/T, Hoffer Q and Holladay 1 formula on predictive error (PE= prediction of postoperative equivalent spherical refraction-actual postoperative equivalent spherical refraction), it is proved that Haigis formula is more accurate than SRK/T in predicting postoperative refractive error in patients with high myopia and cataract. The conclusion of Sharma [19,20] also proves this. In the study of 18501 patients, it was found that the prediction of postoperative refractive state by Olsen formula was better than that by Haigis and SRK/T formula, which was similar to the conclusion of this study. In addition, Rong [21] compared the postoperative predicted diopter of long-axis cataract patients with Haigis and Olsen, and used the median absolute error to analyze each axial subgroup. It was found that in the range of 26mmAL≤30mm, both Haigis and Olsen formulas were accurate for postoperative refractive state, but when AL30mm, the accuracy of Haigis prediction decreased significantly, which may be caused by more influencing factors.
In this study, IOL-master was used to measure ocular biological parameters and predict the diopter of intraocular lens, which has good stability and repeatability. At the same time, surgery was performed by the same physician in this study, which ensures to avoid the interference of other factors.
Our results show that for cataract patients with AL26mm, Olsen formula is significantly better than SRK/T and Haigis formula in predicting accuracy, and Olsen formula is less affected by eye axis length. For patients with ultra-long eye axis, the accuracy and stability of Olsen formula were significantly better than those of Haigis and SRK/T formula. Therefore, we suggest that the formula for calculating the degree of intraocular lens in patients with high myopia complicated with cataract is based on the predicted results of Olsen formula, which can make the patients obtain the diopter which is closest to the true value after operation.
Citation: Ze-Peng XU, Song-Tiao LI, Kun-Meng LI, Ruo-Jun GENG, Hai-Ke GUO, Hong-Yang, et al(2019). Comparison of Three Intraocular Lens Calculation Formulas for Predicting Postoperative Diopter in Patients with Cataract and High Myopia. J Clin Exp Ophthal. 11:845. DOI: 10.35248/2155-9570.20.11.845
Received: 05-Jan-2020 Accepted: 15-Jan-2020 Published: 22-Jan-2020 , DOI: 10.35248/2155-9570.20.11.845
Copyright: © 2020 Ze-Peng XU, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.