Translational Medicine
Open Access
ISSN: 2161-1025
ISSN: 2161-1025
Review Article - (2024)Volume 14, Issue 1
The theme of this report is the inspiration of incredible psychological therapy for Fever of Unknown Origin (FUO). We analyzed this remarkable phenomenon through psychological immunity, liver immunity, inflammation, aetiology, diagnostic methods and treatment strategies. A man, 44 years old, was dyed for more than 40 days due to abdominal distension with skin and scleral yellow and feathers accompanied him for four days to enter the hospital. Hepatitis virus test shows Hepatitis B Virus (HBV) infection. HBV Deoxyribonucleic Acid (DNA) detection offers negative. The detection of the respiratory tract nine-fold, tuberculosis, anaemia and gut-to-club ratio all show negative. Due to the weakness of the patient’s body, we cannot cooperate with more examinations. We use blood specimens to monitor and analyze for 25 days. In short, this is a case of chronic-acute liver failure, manic and fever, likely to be an FUO cause in terms of the treatment plan, general treatment, artificial liver treatment, surgical treatment, anti-infection therapy and psychotherapy. The patient reached the common treatment goal after 25 days of treatment. This report aims to provide psychotherapy programs and clinical characteristics for patients with chronic, acute liver failure, manic and FUO and inspirational thinking strategies for long-term blood specimen examination. The potential mechanism of psychological fever is immune disorders and the decline in the concentration of immunoglobulin A and E may be a direct factor.
Case report; Manic; Fever of Unknown Origin (FUO); Chronic-acute liver failure; Psychotherapy; Artificial liver support system
Development status of the ageing society in china
Hepatitis B virus infection is an infectious disease [1]. When patients with the hepatitis B virus are classified into decompensated liver cirrhosis by pathological classification, the liver loses most of its functions. It requires artificial liver support or transplantation [2]. To the best of our knowledge, there is no report on psychotherapy for acute-on-chronic liver failure in the decompensated phase of hepatitis B cirrhosis. In this type of patient, delaying disease progression is usually the preferred treatment goal. In chronic underlying diseases, liver failure may occur in daily life at any time. We report a rare clinical case of complete remission in a patient with chronic liver failure following combination therapy, including an artificial liver support system, anti-infective therapy, surgery and psychotherapy. The patient also had rare hepatic encephalopathy and unexplained fever, making it a highly complex clinical case. In addition, patient outcomes after treatment were also excellent. Therefore, summarizing the details of the illness and treatment process is very important for other colleagues to treat similar clinical cases in the future. In this study, we summarize the clinical data and discuss possible mechanisms. This case suggests that psychological interventions may be critical in improving clinical outcomes.
Psychological immunity is not a new concept. As early as 1998, some people tried to explore the mystery of this immunity with the key to psychology. Based on a psychological perspective, Abed [3] believes the human immune system can produce "risk scenarios" against adverse emotions to avoid risks. After the emotion can generate "risk scenarios," the person's avoidance of the danger in the future behavior, the avoidance behavior of "danger" is called "immunity." Subsequently, Oláh put forward a new understanding of psychological immunity in 2009. Psychological immunity is a system of adaptive resources and positive personality characteristics of psychological antibodies during pressure: Interconnection [4]. Bayesian [5] mind explains psychological immunity based on Bayesian thinking and Bayesian believes that the belief is the energy to maintain the psychological immune system.
The patient lost his pursuit of an active life and frequently lost control, shouted and fought. The lack of positive faith may be the potential factor of this fever and mania. The lack of positive beliefs that cause fever to cause fever is worthy of in-depth discussion. Rammal H [6] showed an anxiety reduction through animal experiments to reduce the number of general lymphocytes and Immunoglobulin A (IgA) and IgE. The concentration of the Serum Soluble Interleukin 2 Receptor (SIL-2R) will positively affect the severity of the mania and the unique immune response is activated instead of inhibitory [7]. The role of inhibiting the immune response and anti-infection is different. Patients' subsequent evidence of infection is a challenge to those mentioned above in utterly different research. We need more research evidence to explain the relationship between immune response inhibitory and anti-infection protection.
The unique immune response of fever and mania has become a complex factor for treating chronic, acute liver failure. Back to the research process of psychological immunity, we infer that enhanced psychological immune function can buffer environmental pressure, quickly eliminate negative emotions and strengthen protective immune response to anti-infection [8-11]. Our adoption of psychotherapy in clinical treatment will increase the number of "risk scenarios" of patients, giving patients a positive sense of self-efficacy. The positive state is related to the level of adenoceles hormones regulated by the sympathetic nervous system. The cleverness is that the projects of blood sample tests include liver function tests and kidney function tests, blood routine examination (Figures 1A-1D), blood biochemical examination (Figures 1D-1G) and coagulation function (Figures 1F-1I) (Figure 1).
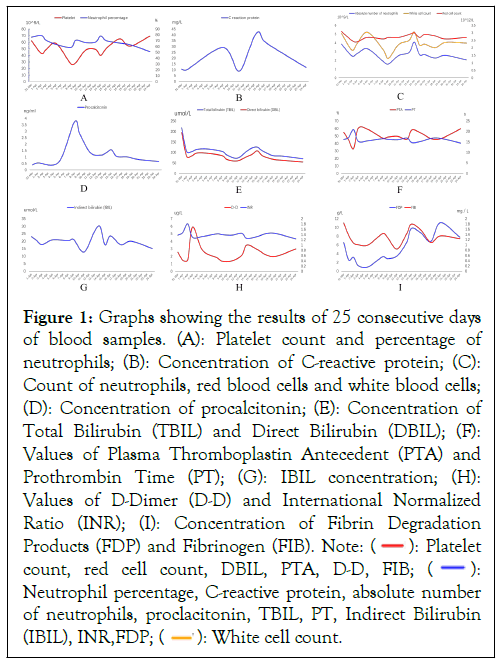
Figure 1: Graphs showing the results of 25 consecutive days
of blood samples. (A): Platelet count and percentage of
neutrophils; (B): Concentration of C-reactive protein; (C):
Count of neutrophils, red blood cells and white blood cells;
(D): Concentration of procalcitonin; (E): Concentration of
Total Bilirubin (TBIL) and Direct Bilirubin (DBIL); (F):
Values of Plasma Thromboplastin Antecedent (PTA) and
Prothrombin Time (PT); (G): IBIL concentration; (H):
Values of D-Dimer (D-D) and International Normalized
Ratio (INR); (I): Concentration of Fibrin Degradation
Products (FDP) and Fibrinogen (FIB).  count, red cell count, DBIL, PTA, D-D, FIB;
count, red cell count, DBIL, PTA, D-D, FIB;  Neutrophil percentage, C-reactive protein, absolute number
of neutrophils, proclacitonin, TBIL, PT, Indirect Bilirubin
(IBIL), INR,FDP;
Neutrophil percentage, C-reactive protein, absolute number
of neutrophils, proclacitonin, TBIL, PT, Indirect Bilirubin
(IBIL), INR,FDP; 
Some special items in the inspection can reflect the protective immune response of anti-infection, such as neutral granulocytes, platelets and lymphocytes. Meanwhile, C-reactive protein is an inflammatory indicator of the body. Using the above monitoring methods, we can more conveniently grasp the characteristics of psychological fever. Ultimately, we decided to use blood samples to monitor for 25 days (Figure 1). Convenient monitoring strategies are the highlights.
Due to the unique immune response mode of HBV, the effect of anti-infection regimens in the treatment of hepatitis B virus infection is limited, so this is the reason why it is difficult to cure HBV completely. Several lines of evidence show that HBV relapse may occur in exceptional circumstances. [12-14]. Negative stress from life events during treatment may exacerbate patients' emotional disturbances, which triggers altered levels of immune responses in the body. Emotions will transform into immune information, which regulates liver immunity through special pathways. Natural Killer (NK) cells are the primary cells in the liver that transmit virus immune information and are an important part of the liver immune system.
After NK cells are activated, they will continue to destroy the original hepatic parenchymal cells and accelerate the development of liver cirrhosis. The development of liver cirrhosis may come from the accidental activation of HBV and reinfection of liver cells. The currently known route of activation is radiation. After long-term clinical application and research, Natural Interferon Alpha (IFN-α) is the most promising substance for treating the hepatitis virus. Nearly half of chronic hepatitis B patients will benefit from life.
Meanwhile, IFN-α is a substance secreted by immune cells. Large amounts of exogenous IFN-α in the body can cause solid psychiatric symptoms, considered the most dangerous adverse reaction and there is evidence that it will directly lead to death. One piece of evidence that deserves our attention is the report by Altindag et al., [15]. On patients with chronic hepatitis who received IFN-α without other adjuvant therapy. Viral hepatitis induced unpredictable mania. As people's demand for a better spiritual life continues to increase, psychosomatic treatment has received more and more attention [15,16]. The liver can hydrolyse proteins in a multiphase reaction to perform detoxification functions. After hepatitic cirrhosis, many collagen fibers replaced hepatic cords and hepatic lobules and the original hepatic lobule model is likely to transform into a pseudo-lobular model. Liver macrophages and NK cells cannot complete liver immunity through the liver lobule model. At this time, the emergency plan is to activate the artificial liver support system to remove plasma inflammatory substances and wastes quickly, alleviate the progress of liver failure and gain valuable time to resist infection [17-19].
Demographic information and clinical findings
A 44-year-old retired policeman was admitted to the hospital in March 2022 due to a fever of unknown origin, scleral yellow staining and a manic episode for seven days. He has been diagnosed with viral Hepatitis B, Hepatitis B, Cirrhosis (HBC) and coagulation disorder. The treatment has been irregular for four years and there is little curative effect. Apart from fever, manic episodes and expectoration, there were no other clues. Physical examination showed epigastric tenderness, peritoneal effusion, spleen enlargement, painful gallbladder percussion and thick breath sounds without abnormalities of other organ systems. The patient is 175 cm tall, has recently lost 5 kg and now weighs 70 kg. The patient recently had insomnia throughout the night.
Diagnostic assessments and idea
Thoracic ultrasonography revealed right-sided pleural effusion (moderate volume), but left-sided pleural effusion was absent. Abdominal ultrasound showed a small amount of fluid in the abdominal cavity. Upper abdominal Magnetic Resonance Imaging + Magnetic Resonance Cholangio Pancreatography (MRI+MRCP) showed a small cyst under the left capsule of the liver and we considered cholestasis. The spleen has a mild enlargement-a small amount of fluid exuded from the peritoneal cavity. Chest Computed Tomography (CT) showed lung infection. There are calcifications on the back of the left lower lobe and there are small nodules in the lateral basal segment of the left lower lobe, which we consider to be inflammatory nodules. HBV-DNA’s quantitative polymerase chain reaction levels were tentatively harmful (Table 1). The patient had a temperature of 39.4°C (102.92 F) on admission for three days.
| Test | Result |
|---|---|
| TORCH | Rubella IgG(+) cytomegalovirus IgG(+)herpes simplex virus1 IgG(+) |
| The EB virus antibody test | EB IgG(+) |
| Hepatitis B antibody test | (+) |
| Hepatitis B DNA test | (+) |
| Hepatitis C antibody test | (-) |
| Quantitative urinalysis | Bilirubin(+) |
| Tuberculosis specific response test | (-) |
| ANCA vasculitis test | (-) |
| Screening for hepatocellular carcinoma | (-) |
| Respiratory tract | Pulmonary bacterium(-), Pneumonia stroma(-), Respiratory syncytial virulence(-), Adenopathy(-), Q hot ritsu katsuji body(-), Kou type flu toxin(-), Type B flu poison(-), side stream disease poison(-) |
| Digestive tumor test | CA199 test 129.5 ng/ml, CA125 test 125.46 ng/ml |
| Stool routine+occult blood | (-) |
| Enterococcus/Bacillus ratio | (-) |
| Anemia | Ferritin 462.9 ng/ml, folic acid determination 2.45 ng/ml, serum vitamin test 1319 pg/ml |
| Mycobacterium tuberculosis nucleic acid detection | (-) |
Note: TORCH: Toxoplasmosis; Rubella Cytomegalovirus; Herpes simplex and Human Immunodeficiency Virus; EB virus: Epstein-Barr virus; DNA: Deoxyribonucleic Acid; ANCA: Anti-Neutrophilic Cytoplasmic Antibody; IgG: Immunoglobulin G.
Table 1: Results of a comprehensive inspection to find the cause of the fever.
The patient was treated with a hibernation mixture and antiinfection with meropenem (0.5 g once daily). Due to the rapid progression of the patient’s liver failure, we used an artificial liver support system (twice a day on day 1; once a day on day 3) as a first-line treatment three times. Subsequently, biochemical analysis of liver function and blood coagulation tests showed a recurrence. The artificial liver support system's effectiveness led us to continue the original treatment plan. Therefore, we plan to do a comprehensive examination (Table 1) to determine the cause of this disease. At the same time, we chose to use the patient's blood samples for continuous monitoring. The patient could not complete imaging and pathological examinations during the treatment period due to extreme weakness.
After three laboratory tests of the artificial liver support system, the pictures (Figures 1E and 1G) showed that multiple test indicators had a trough on April 2. The yellowing of the patient's skin improved significantly and his life was temporarily out of danger.
However, the patient experienced another manic episode. Patients showed moodiness, beating, swearing and throwing things. The patient's friends always commented that he seemed to be possessed by a demon, like a lunatic. We invited a psychiatrist to consult and considered it a manic episode. Psychiatrists believe that the evidence for the diagnosis of schizophrenia is insufficient and at the same time, the patient encountered violence when he was young. Such a miserable state of mind may cause physical stress due to illness. On the first day of the patient's treatment, we thought he had a rare hepatic encephalopathy because the blood ammonia concentration was not high at 32 umol/L (Table 1). Nonsense, mania and fever were in line with the manifestations of hepatic encephalopathy. According to the psychiatrist's opinion after consultation, we denied the diagnosis of rare hepatic encephalopathy because the results of 3 consecutive days of blood sample testing and comprehensive examination could not prove the biological factors of fever. We hypothesized that the patient's fever and acute-on-chronic liver failure were independent factors.
After the above analysis, Quetiapine Fumarate extended-release tablets (400 mg once per night) and Magnesium Valproate sustained-release tablets (0.25 g twice daily) were applied for treatment. At the same time, we must combine it with psychotherapy. Patients with chronic liver disease are often in serious condition, long-term hospitalization, heavy ideological burden and shame for their family and family. We care about patients' psychological pressure, leading to language bias and talking to themselves.
On the 14th day, the patient suddenly developed insomnia and expectoration and the manic attack improved. At that time, the highest body temperature of the patient was 38.6°C. We discontinued Quetiapine Fumarate extended-release tablets and Magnesium Valproate extended-release tablets. An incidental imaging study found that MRI+MRCP of the upper abdomen showed a small cyst in the left outer lobe of the liver, cholecystitis, cholestasis and mildly enlarged spleen; exudate and a small amount of fluid in the abdomen. Chest CT showed lesions in the lungs. Small nodules can be observed in the lungs, considering inflammatory nodules. Elevated bilirubin and total bile acids suggest cholecystitis. At the same time, we found that in the 14 consecutive days of blood sample testing, there was a peak in the inspection indicators on the 14th day, such as the absolute value count of red blood cells (Figure 1C), neutrophils (Figures 1A and 1C), C-reactive protein (Figure 1B) and procalcitonin (Figure 1D). We cannot explain this phenomenon by aetiology. Combined with the patient's psychological factors and 14 consecutive days of blood sample examination, we believe that psychological factors promote the development of psychological cholecystitis because anxiety can reduce the concentration of IgA and IgE, which disturbs the body's immune function.
On the other hand, cirrhosis increases the burden of hepatic functions, such as the synthesis and secretion of immunoglobulins. In addition, mood disorders excite the sympathetic nerves and release large amounts of norepinephrine. The sympathetic nerves constantly regulate the intestinal tract, resulting in intestinal vasoconstriction, which is not conducive to maintaining the homeostasis of the body's biological immune barrier (Figure 2). There is also flora on the surface of the respiratory tract. Suppose the flora on the surface of the respiratory tract is disturbed and thus changes the homeostasis of local mucosal immunity. In that case, it is currently difficult for us to intervene with the flora. To sum up, we consider the use of surgical treatment and increase the intensity of psychological treatment.
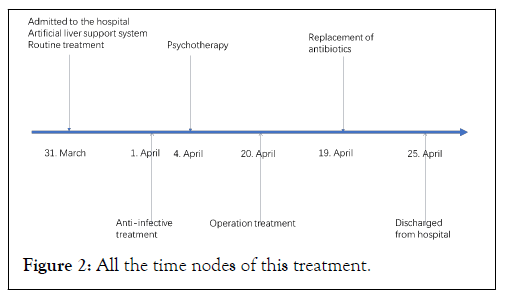
Figure 2: All the time nodes of this treatment.
On day 17, we performed a "percutaneous trans hepatic gallbladder drainage" surgically. Drainage fluid is 20 ml dark green liquid. We adjusted antibiotics based on susceptibility testing (Table 1). We then used a combination of anti-infective therapy and psychotherapy.
On the 25th day, the patient underwent another eight days of treatment to achieve the patient's expected goal. The indicators of the 8-day continuous blood sample inspection (Figure 1) tended to be stable. The patient deeply experienced the superiority of our treatment, so he wrote a letter of thanks to us.
Figure A shows the platelet count and the percentage of neutrophils. The patient's platelet count was lower than the level of the general population for 25 consecutive days and there was a high risk of bleeding. The results of the percentage of neutrophils showed that it was between 50% and 75%, which did not support the diagnosis of infectious diseases and hematologic malignancies. Figure B represents the concentration of C-reactive protein. The data from 25 consecutive days indicate non-specific inflammation in the body. After psychotherapy started on day 5, the CRP concentration decreased significantly on day 12 and on day 17, after surgical treatment, the combined anti-infection treatment and psychotherapy showed a significant decrease again. The two significant drops suggest that psychological intervention was effective in this case. Panel C represents absolute neutrophil count, red blood cell count and white blood cell count. The absolute values of white blood cells and neutrophils fluctuated within normal levels, which did not support infectious diseases and could not explain the sudden cholecystitis on day 14. The peaks of white blood cell count and an absolute value of neutrophils appeared on the 6th and 14th day, which may imply that psychotherapy affects the body's immune homeostasis. The red blood cell count is always slightly lower than ordinary people, indicating that the patient may be anemic. Panel D represents the concentration of procalcitonin. The figure shows that the systemic inflammatory response is more evident on the 9th and 15th day, which suggests that the patient may have multiple organ failure, infection and hyperthyroidism from the seventh day. Evidence that the patient had persistent manic episodes is more likely to add to the persuasion that the patient is hyperthyroid. Panel E shows the concentrations of Total Bilirubin (TBIL) and Direct Bilirubin (DBIL). On admission, we found that TBIL and DBIL exceeded the normal range by ten times, providing a diagnostic basis for liver failure and cirrhosis. TBIL and DBIL decreased after we used the artificial liver support system. Panel F shows the values of Prothrombin Time Activity (PTA) and Prothrombin Time (PT). The results of PT> 9.60 and PTA<75% show that the patient has coagulation dysfunction. Panel G represents IBIL concentrations. Panel H shows the values of D-dimer (D-D) and International Normalized Ratio (INR). The concentration of D-dimer (D-D) is generally stable. Both outcomes were associated with patients’ risk of bleeding tendency. Panel I represent the concentration of Fibrin Degradation Products (FDP) and Fibrinogen (FIB). The overall fluctuations are like those of the INR (Table 1).
Although the digestive tract tumor examination results were abnormal, it was related to body weight loss. This comprehensive examination showed that the cause of the fever was not the abovementioned factors (Figure 2).
After stepping into the old age stage, the body’s ageing is expected to directly impact one's behavioral characteristics. With prominent dull actions and a slow reaction speed, the elderly witness weaker movement coordination. In addition, the elderly is prone to getting exhausted and feeling fatigued. Finally, given the sharp decline in the physical function of the elderly, their resistance will also gradually weaken. In such cases, they must attach great importance to seasonal changes and diseases brought by climate change, which the elderly will cast their eyes on and fully leverage preventive measures in advance.
What happened to this patient was full of wonder? On admission, the patient presented with abdominal pain, abdominal distension, fever (39.3°C), mania and jaundice. Before being admitted, He treated himself in other hospitals for post-hepatitis B cirrhosis and liver failure. After one month, the effect was not noticeable. He had no history of mental illness, had a history of the hepatitis B virus hepatitis and had a strong belief in Buddhism. After admission, we asked about the medical history in detail. After a physical examination and routine laboratory tests, we could not make a precise diagnosis that met the WHO definition of fever of unknown origin.
The patient, in our case, had a nightmare childhood. He always said that the gods possessed him whenever we communicated with him. He could always talk for more than two hours. The patient's presentation resembled schizophrenia, mania and hepatic encephalopathy. After a final consultation with a psychiatrist, we confirmed the diagnosis of a manic episode. The patient’s blood ammonia concentration of 32 umol/L after admission does not support the diagnosis of hepatic encephalopathy and the evidence for the diagnosis of schizophrenia is not sufficient. The patient had an acute onset and the total bilirubin was 221.8 umol/L, the direct bilirubin was 193.7 umol/L, the albumin was 34.8 g/L, the prothrombin activity was 60%, the international normalized ratio was 1.39 and the procalcitonin was 0.535. nm/ml, combined with the previous history of hepatitis B, meets the diagnostic criteria for acute-on-chronic liver failure. Therefore, until more evidence emerges, we first consider acute-on-chronic liver failure, manic episodes and Fever of Unknown Origin (FUO).
To prolong his life, we started three times of artificial liver system supportive treatments and, at the same time, adopted a routine treatment plan. We monitored liver and kidney functions dynamically during this period. In addition, we tried to find the cause of the fever through laboratory tests. Due to the poor physical operation of the patient, the patient did not undergo imaging and pathological examination.
In a random physician discussion, we decided to use psychotherapy. The patient's childhood experience may have caused persistent psychological trauma, which makes the patient extremely concerned about his body and emotionally sensitive. We boldly speculate that the aetiology is psychogenic fever. After a period of psychological treatment, an unexpected examination found suppurative cholecystitis. We immediately performed transcatheter cholangiography on the patient and about 15 ml of fluid.
At this time, we made a new inference: purulent cholecystitis caused the fever. Therefore, we use anti-infective therapy and surgical treatment. A few days later, the patient's body temperature returned to normal, but the symptoms of manic were challenging, which puzzled us. What is the cause of gallbladder infection? According to the previously checked clues, the positive result we can find is Escherichia coli and sputum culture (Table 1). However, the results of laboratory inspections cannot explain this phenomenon. So we made it guess that patients attached too much attention to their experience because of their childhood trauma. This liver failure awakened the childhood trauma, which launched his psychological defense mechanism-for example, beating, scolding and attachment. Continuous hospitalization treatment may strengthen the psychological defense mechanism and lead to purulent cholecystitis. Psychological factors have exacerbated the progress of liver failure. In the end, we used anti-infection therapy and psychotherapy. The patient reached the ideal recovery state. After the patient left the hospital, he wrote a thank-you letter to us. The treatment results are enough to explain why the symptoms of patients with the combination of antibiotics and psychotherapy are incredible.
Underlying pathogenesis
Hepatic encephalopathy is a common complication of liver failure. The clinical manifestations of hepatic encephalopathy are also like manic episodes. Clinically, we can identify hepatic encephalopathy or manic episodes by the ammonia concentration in the blood. However, hepatic encephalopathy and fever often coexist, which is one of the reasons why patients with liver disease have difficulty in treatment after fever. With the development of psychotherapy, psychogenic fever has gradually come into people's field of vision. However, until now, there is still no definite evidence for the relevant mechanism or causal relationship. In our case, cholecystitis and psychological factors were almost equally important and more convincing clinical evidence was negligible due to the patient's functional inability to withstand imaging and pathological examinations. The previously reported psychogenic fever and psychogenic gastric ulcer provided clues to our final speculation. Calcitonin 0.4 ng/ml in blood samples (Figure 1D) did not explain infection in suppurative cholecystitis. The result provided a biased suggestion for psychogenic cholecystitis without clinical evidence.
Studies have shown that HBV combined with Hepatitis C Virus (HCV) infection can lead to manic symptoms. Physical factors can also change the immune status of the body. For example, radiation can promote endothelial cells to secrete IL-6 [20]. A long-term study pointed out that radiation is a factor in the reactivation of the hepatitis B virus. After we passed the hepatitis virus test, we only found that the hepatitis B virus infection was positive. The rest were regular (Figure 2). Some people use immune pathological biopsy of liver tissue to believe that the destruction of normal liver tissue will reduce liver immunity after the onset of liver failure and the activation of NK cells around the liver lobules. This factor makes patients with liver failure more susceptible to infection. In recent years, psychological immunology studies have produced much evidence for the interaction between psychology and immunity. These immune functions suppress the immune response by downregulating the levels of lymphocytes and immunoglobulins. In addition, emotions inhibit the biological function of sympathetic nerves by finely regulating the hypothalamicpituitary- adrenal axis. IFN-α is associated with manic episodes [21-24]. NK cells kill liver cells during liver failure. Downregulation of immunoglobulin levels [25-28]. Increased risk of opportunistic infections following Downregulation of immunoglobulin levels. Microorganisms that colonise the skin surface, intestinal mucosa and respiratory mucosa multiply by competing for the nutrients of the dominant microorganisms in the past, leading to opportunistic infections. Dysbiosis is a risk factor for immune suppression. Given the uncertainty of psychological factors, we believe psychological factors are more likely to cause this fever.
Significance of artificial liver support system in inflammation
Liver failure with unexplained fever is challenging to manage clinically. With the in-depth exploration of inflammatory substances in the complex mechanism of liver failure, the artificial liver support system has shown a new dawn [29,30]. Liver parenchymal cells become fibroblasts due to cirrhosis. Fibroblasts randomly switch between activated and quiescent states in an inflammatory microenvironment. Many mitochondria can undergo a transmission electron microscope in decompensated liver cirrhosis slices. The mitochondrial inner membrane is abnormally active in transmitting Q, which releases oxygen-free radicals [31]. Since fibroblasts do not have enough organelles to consume the electrons produced by mitochondria, this becomes a booster of the inflammatory storm [32]. The second driver of the inflammatory storm is impaired liver function because the pseudo lobule cannot perform the normal physiological functions of the hepatic lobules. There is strong evidence that artificial liver support systems can improve hepatic hemodynamics with the use of artificial liver support systems [33-36]. We provided patients with an artificial liver support system three times, which bought precious time for the liver to repair itself. The tremendous significance of artificial liver support systems lies in creating a favorable microenvironment for improving severely damaged livers.
Regrettably, this report does not involve liver biopsy reports. When someone discusses the value of artificial liver in inflammation, using transmission electron microscopy and light microscopy to observe liver biopsy samples may be more valuable.
Perspective on treatment options
We recommend using an artificial liver support system combined with liver protection therapy. For fever of unknown origin, wait for the results of laboratory inspection, bacterial culture and drug sensitivity test. Before deciding if the patient's current life is in danger or if it is difficult to control the patient to cooperate with the treatment actively, first use empiric antibiotics to try to control the condition urgently. After waiting for sufficient identification and investigation to determine that it is a psychogenic fever, we recommend using psychotherapy combined with psychoactive substances. In the acute phase, manic patients often have obvious symptoms such as excitement and desire. They are prone to destroy interpersonal relationships and hurt others, causing economic losses and infectious diseases. Therefore, the primary purpose of drug treatment is to control or relieve manic symptoms as soon as possible. Lithium and sodium valproate are the first choice for treating manic episodes. We are more likely to choose Sodium valproate for this treatment because of the high rate of adverse effects of lithium. A meta-analysis of 22 RCTs by Tamayo et al., [16] showed that lithium monotherapy was more effective than a placebo for acute manic episodes. However, there were more treatment interruptions due to adverse effects, so we should exercise caution.
Interestingly, a randomized clinical study by Oquendo’s group showed that lithium was more effective than valproate in preventing suicidal behavior in bipolar patients with suicidal thoughts. Lithium is appropriate for patients at very high risk of manic episodes, which may reduce suicidal behavior by reducing aggression and potential impulsivity [37-40]. In this case, we treated the patient's manic symptoms with valproate Because not only did valproate have fewer adverse reactions than lithium, but also the patients were not suicidal.
The combination of anti-infective therapy and psychotherapy, following the support of an artificial liver system, not only addressed the immediate life-threatening conditions but also catered to the overall well-being of the patient. This case highlights the importance of considering a broad differential diagnosis and the value of a multidisciplinary treatment strategy in managing complex liver diseases. Psychological intervention may have unexpected effects on complex liver diseases. The successful remission of the patient underscores the potential role of psychological support as a complementary treatment alongside conventional medical intervention. The integration of psychotherapy helped manage the psychological aspects, potentially improving the patient’s resilience and adherence to the treatment regimen, which may have contributed to the positive outcome. We cannot unthinkingly attribute fever and manic symptoms to hepatic encephalopathy.
This case serves as a reminder of the intricate interplay between the physical and psychological facets of health, particularly in the context of liver diseases that can profoundly affect mental status. It suggests that future treatment protocols for acute-on-chronic liver failure could benefit from incorporating psychotherapeutic interventions, especially in cases where psychological factors may influence the clinical presentation and recovery process. Psychological interventions combined with other treatment options may more easily meet patients’ treatment goals than existing treatment options.
The favorable outcome in this case provides a promising direction for future research and clinical practice, advocating for a more holistic approach to treating acute-on-chronic liver failure. It also calls for further studies to validate the effectiveness of such integrated treatment modalities and to establish guidelines that can be generalized to a broader patient population. In the future, diagnosing and treating patients with acute-on-chronic liver failure may focus on inconspicuous causes such as fever.
This study is an isolated clinical case. It is rare for people with liver failure to have psychological problems starting in childhood. Our hospitals focus on treatment and the testing capabilities of laboratory equipment are limited. For example, we cannot implement this test for the gene profile expression of inflammatory factors. In addition, the patient’s physical function cannot withstand pathological and imaging examinations. Relying on blood tests alone will affect the convincingness of clinical evidence and the lack of liver biopsy will also affect clinical evaluation.
Funding
Mr. Yan received funding from Fundamental Research Funds for the Central Universities (31920170197).
Ethics approval statement
The studies involving human participants were reviewed and approved by the Hong Kong Island Western Hospital Cluster of the Hospital Authority. (Reference No.: Reference UW 20-177).
Patient consent statement
The study has got approval from patient
Ethics approval and consent to participate
Not applicable. This study has not involved any human or animals in real or for experiments.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Bo Y, Li B, Wang Y, Sha R, Yu H, Miao C (2024) Complete Remission of a Patient with Acute-on-chronic Liver Failure with Rare Hepatic Encephalopathy and Fever of Unknown Origin Treated with Anti-infective Therapy Combined with Psychotherapy After Artificial Liver Support System. Trans Med.14:316.
Received: 14-Dec-2023, Manuscript No. TMCR-23-28492; Editor assigned: 18-Dec-2023, Pre QC No. TMCR-23-28492 (PQ); Reviewed: 01-Jan-2024, QC No. TMCR-23-28492; Revised: 08-Jan-2024, Manuscript No. TMCR-23-28492 (R); Published: 15-Jan-2024 , DOI: 10.35248/2161-1025.24.14.316
Copyright: © 2024 Bo Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Sources of funding : Mr. Yan received funding from Fundamental Research Funds for the Central Universities (31920170197).