
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2020)Volume 11, Issue 4
Chronic regional pain syndrome (CRPS) is a rare condition following percutaneous coronary intervention (PCI) via trans-radial (TR) approach. The pathophysiology of CRPS is still poorly understood, and it is often misdiagnosed and poorly treated in its initial phases leading to severely compromised quality of life. Here we present a rare case of a patient, who was diagnosed with CRPS type 2 after PCI via TR approach. CRPS presented with a classical triad of sensory, autonomic and motor dysfunction and signs of nerve lesion on electromyography (EMG). Patient received multimodal treatment with ketamine in addition which resulted in favorable outcome in less than six months. Ketamine is a promising agent in CRPS treatment, but more studies are needed.
Chronic regional pain syndrome; CRPS; Percutaneous coronary intervention; PCI; trans-radial; Ketamine
TR access is a frequently preferred site for cardiac catheterization among interventional cardiologists. The TR as compared to trans-femoral approach has fewer access site complications, reduced mortality and hospital length of stay [1-3,5]. However, invasive procedures, specifically to the upper extremity, are a risk factor for a rare, but severely disabling condition-CRPS, which is characterized by progressively worsening spontaneous regional pain with or without dermatomal distribution [4]. In this report we would like to present a rare case of CRPS type 2 and pain management following PCI via TR approach associated with a traumatic injury to the nerves, tissues followed haemostatic compression and hematoma formation.
A 71-year-old woman was admitted to our Cardiology Department with an acute myocardial infarction and a percutaneous coronary intervention (PCI), using a right TR approach was performed urgently. Patient has no pain or other condition previously at access site. During the procedure there were no complications, the haemostatic device was put on the entry site after removing the radial sheath. Immediately after admission to Intensive care department the patient began complaining of a severe burning and stabbing-like pain in her right arm. On the physical examination the arm was visibly swollen, and hematoma was present. After performing ultrasonography, which revealed no signs of a pseudoaneurysm, non-steroidal anti-inflammatory drugs (NSAIDs), heparin ointment and pentoxifylline 800 mg/day were prescribed together with physical therapy; gradually the swelling diminished and hematoma disappeared. However, during the rehabilitation period the patient continued experiencing episodes of debilitating pain on the PCI access site, requiring opioids (tramadol, morphine). During discharge from the rehabilitation unit the patient was prescribed gabapentin and tramadol for the continuous sharp pain in her right arm and referred to a plastic surgeon who ordered and EMG test. The EMG showed signs of severe median nerve neuropathy, both sensory and motor partial axonal degeneration of the right ulnar nerve; absent responses of the sensory part of the right radial nerve and signs of partial motor axonal degeneration. After EMG (1 month after PCI) the patient was referred to our outpatient Pain Clinic where the following pain characteristics were obtained: burning and stabbing pain of the right hand, the Verbal Rating Scale-the worst possible pain, 100 mm on the Visual Analogue Scale. The Numeric Rating Scale (NRS)-10 points; the Neuropathic Pain Scale-7/10. Hospital anxiety and depression scale (HADS): anxiety-4 points (normal) and depression-8 points (mild). During physical examination the right hand and wrist were warm, erythematous and oedematous (Figure 1); there was no change in nail or hair growth. Skin temperature of the right/left hand was 36.4/34°C respectively.
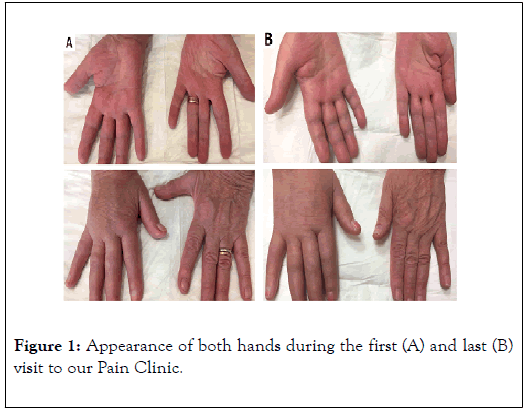
Figure 1. Appearance of both hands during the first (A) and last (B) visit to our Pain Clinic.
Sensory abnormality (hyperalgesia in ulnar nerve innervations zone, hyperalgesia and mechanic allodynia in median nerve innervations zone) and motor deficits were detected (inability to flex the fingers of the right hand-0 points, wrist flexion-3 points, adduction and abduction of the fingers-2 points, abduction of the thumb-2 points). Muscle power of the upper right arm was normal. A diagnosis of CRPS type 2 was made according to the current standard diagnostic criteria (Table 1).
| Budapest Criteria: clinical diagnostic criteria for CRPS |
| Continuing pain, disproportionate to any inciting event. |
| Must report at least 1 symptom in 3 of the 4 following categories: |
| Sensory: reports of hyperalgesia and/or allodynia |
| Vasomotor: reports of temperature asymmetry and/or skin color changes and/or skin color asymmetry |
| Sudomotor/edema: reports of edema and/or sweating changes and/or sweating asymmetry |
| Motor/trophic: reports of decreased range of motion and/or motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nails, skin) |
| Must display at least 1 sign at time of evaluation in 2 or more of the following categories: |
| Sensory: evidence of hyperalgesia (to pinprick) and/or allodynia (to light touch and/or deep somatic pressure and/or joint movement) |
| Vasomotor: evidence of temperature asymmetry and/or skin color changes and/or asymmetry |
| Sudomotor/edema: evidence of edema and/or sweating changes and/or sweating asymmetry |
| Motor/trophic: evidence of decreased range of motion and/or Motor dysfunction (weakness, tremor, dystonia) and/or trophic changes (hair, nails, skin) |
| There is no other diagnosis that better explains the signs and symptoms. |
Table 1: The Budapest Criteria. Diagnostic criteria for CRPS defined by an international consensus meeting [17,18].
Since physical therapy, which is considered to be the first line therapy, resulted in worsening of the symptoms, the treatment was initiated with 0.15 mg/kg intravenous (i/v) ketamine (10 mg in total) which showed significant reduction in pain from 10 points to 5according to NRS on the first visit. The patient was scheduled to visit the Pain clinic every 10 days and received multimodal treatment with ketamine, neuropathic medications, phosphodiesterase inhibitors and vitamin B complex (Table 2). After two months from the first visit, the patient was responding well to the treatment-the intensity of the pain reduced from 5 to 3 points according to NRS. At the follow up visit six months after the initiation of the treatment the patient had no complaints of pain.
| Pain Clinic | Visits | Medications | Treatment outcomes |
| 1st visit January, 2017 | Ketamine 10 mg IV (0.15 mg/kg) | Pain before medication: 10 points (NRS); Pain after medication: 5 points (NRS) | |
| 2nd – 6th visit January – February, 2017 | Ketamine 10mg(0.15mg/kg) IV during each visit | Pain on the 2nd visit: 5 points (NRS); | |
| Gabapentin 900 mg/d PO Pentoxifylline 800 mg/d PO Vitamin B complex IV, PO |
Pain on the 6th visit: 3 points (NRS) | ||
| 7th visit July, 2017 | None since June, 2017. | No pain on the 7th visit. |
Table 2: Treatment of the patient with CRPS type 2 in Pain Clinic.
Commonly known and well-recognized complications of TRA are vascular-hematoma, pseudoaneurysm, dissection, occlusion, arteriovenous fistula, thrombosis and embolism. Isolated neurological complications such as nerve damage (0.16%), motor disability (0.26%), sensory loss (1.52%), persistent pain (6.67%) are rarely present [5]. However, the preliminary results of ARCUS trial state that upper extremity dysfunction after TRA persists up to 6 months after procedure [6]. Only a few case reports on CRPS related to TRA [5,7,8] or vascular injury [9-12] have been reported worldwide. CRPS is a chronic pain condition most often preceded by a traumatic insult to the extremities with a prevalence of approximately 5.4-26.2 per 100,000 person [13]. The traumatic event may be a fracture (42%), blunt trauma (21%), surgery (12%), spontaneous vases (7%), carpal tunnel syndrome (7%) etc [14]. As the name implies, the pathophysiology behind the disorder is complex, including inflammatory changes from the initial traumatic injury, both peripheral and central nervous system sensitisation and autonomic dysregulation. Psychological factors such as catastrophizing and genetic predisposition may have a role as well [13]. The syndrome manifests as a complex regional pain disproportionate to the time and severity of inciting traumatic injury, with sensory system impairment (pain, hyperalgesia), autonomic signs (trophic changes, oedema) and motor dysfunction (paresis, tremor, dystonia) [8]. The International Association for the Study of Pain (IASP) divides CRPS according to the absence (CRPS type 1) or presence (CRPS type 2) of organic nerve lesion. CRPS type 2 accounts for the minority of CRPS cases. Ott and Maihöfner analysis of 1043 patients with CRPS [14] revealed that sharp traumas are among the most popular triggers for CRPS type 2 development. The main causes are median or radial nerve injury during the puncture [7], median nerve ischemiafrom radial artery occlusion secondary to prolonged haemostatic compression [15] and hematoma formation [9,16,18]. The EMG performed on our patient showed significant changes to the right median, radial and ulnar nerves. The patient met the criteria (Table 1) and the diagnosis of CRPS type 2 was made. Because of its complex and unclear pathophysiology and scarce evidence there is no golden standard of treatment. The typical approach is a symptomatical multimodal regime to target different components of the syndrome [4,19]. Our treatment of choice was standard neuropathic medication for the neuropathic component of CPRS, phosphodiesterase inhibitors for microvascular dysfunction and ketamine, which is under extensive research as etiology - based treatment [20]. Since its introduction into anaesthesiology ketamine has been the most controversial anaesthetic. A large amount of research has already established its role in management of acute perioperative pain [21] and some chronic pain conditions, including CRPS [22]. Ketamine acts by inhibiting N-methyl-D-aspartic acid (NMDA) receptors which are involved in acute and chronic pain pathways. Activation of these pathways leads to a central sensitization phenomenon, which is a component of CRPS. Ketamine was included in the UK, Dutch and American guidelines for treatment of CRPS, all of them stating that there is “moderate evidence for i/v ketamine, but more studies are needed ” [16,17,23]. American guidelines suggest using ketamine in anesthetic (22 mg/h for 4 days) or sub-anesthetic (0.35 mg/kg per hour over 4 hours daily for 10 days) doses. A few studies showed very promising results with i/v ketamine administered in anesthetic doses for refractory CRPS, however, safety issues, psychotropic side effects and intensive care nature of treatment remain a concern [24,25]. Our patient received treatment with sub-anesthetic ketamine doses, because to be linked with less frequent and milder side effects and there is no need for intensive care. Uncertainty about the possibility of shorter duration of pain relief after administration sub-anesthetic doses raises questions about the efficacy of treatment [20].
In conclusion, with the increasing amount of trans radial procedures performed everyday it is important for the practitioners to be aware of CRPS, even though uncommon, but severe complication, associated with a significant decrease in patients quality of life and be able to refer the patient to seek prompt care from a specialist, experienced in treating CRPS. Ketamine is a promising agent in CRPS type II treatment, but more studies are needed.
Citation: Urbonaite A, Brogiene L, Macas A, Zemgulyte G (2020) Complex Regional Pain Syndrome Type 2 after Percutaneous Coronary Intervention: A Case Report. J Anesth Clin Res. 11: 945. DOI: 10.35248/2155-6148.20.11.945
Received: 25-Mar-2020 Accepted: 10-Apr-2020 Published: 17-Apr-2020 , DOI: 10.35248/2155-6148.20.11.945
Copyright: © 2020 Urbonaite A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.