Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research - (2019)Volume 9, Issue 10
Background: Laparoscopic surgery in gynecology is a minimally invasive technique, which is not void of complications. Our objective was to assess the various complications which occur during gynecological laparoscopy and their associated risk factors at the Gonesse General Hospital (GGH).
Method: We carried out a cross-sectional study with retrospective data collection over a two year period from August 1, 2009 to July 31, 2011, at the maternity ward of the GGH. We included all the patients operated by laparoscopy during the study period. A complication was defined as any event that affected the normal course of the procedure and resulted in a rescue action like laparotomy or close surveillance. The proportions were calculated and compared using the Chi-square test. The statistically significant threshold was set at 0.05.
Results: A total of 266 women underwent gynecological laparoscopy during the study period. The mean age was 35.78 ± 12.34 years; up to 12.4% of the patients had a past history of laparotomy, while 17.3% had history of laparoscopy. Nearly half of the number of laparoscopic procedures was carried out in the context of an emergency (54.5%) and the major indications were ovarian cysts (25.2%) and ectopic pregnancies (20.3%). A total of 18 surgical complications were identified, representing 6.77% of the sample size. The complications were mostly hemorrhagic in up to 50% of the cases and laparotomy was the main recourse when the complications occurred in 66.7% of the cases. The occurrence of complications was significantly associated with major procedures, p=0.000.
Conclusion: There was a high rate of complications in our study and these complications were mostly haemorrhagic in nature and associated with major procedures. The most frequent method of management of these complications was by laparotomy.
Gynaecologic laparoscopy; Complications; Haemorrhage; laparotomy
Laparoscopic surgery is a very fancy surgical technique used in managing gynaecological pathologies. This type of minimally invasive surgery has many advantages over conventional surgery. It is known to be associated with better anatomical recognition of pelvic structures and allows direct diagnosis and therapeutic procedures with fewer traumas. Moreover, the operator has a better view of the cleavage planes.
Thus, classical surgery tends to be more often replaced by this type of modern and precise surgery [1]. Despite these advantages, both techniques share the same risk of major complications, such as pulmonary embolism, blood transfusion, fistula formation, and unplanned major surgery [2]. Therefore, laparoscopy surgery can also lead to serious and life-threatening complications. Early identification of these complications during the procedure and effective management may improve post-operative outcomes. In order to increase the awareness of practitioners on the possible surgical complications that may occur during the procedure and to explore conditions susceptible of inducing poor outcomes after a gynaecological laparoscopy, we carried out this study at the maternity ward of the Gonesse General Hospital.
We carried out a cross-sectional study with retrospective data collection over a two-year period, from August 1, 2009 to July 31st, 2011 at the maternity ward of the Gonesse Hospital.
We went through all medical records of women who have undergone gynecological laparoscopy during the study period in our hospital. We collected data from medical records and postoperatory reports.
Data collected consisted of anthropometric characteristics; past history (of laparotomy, laparoscopy and pelvic infection), the surgical indication, type of laparoscopy, the type of complication if any, the time of onset of these complications and the treatment initiated.
A complication was defined as any event that affected the normal course of the procedure and resulted in a rescue action, such as close monitoring or laparoconversion.
Anesthetic complications were not described in this study. We classified the type of laparoscopy as follows: Diagnostic laparoscopy: was classified as any laparoscopic procedure which consisted of doing methylene blue or carmine indigo tests, pelvic washings for pelvic infections and second-look laparoscopy without surgical procedures, Minor laparoscopy consisted of minimal adhesiolysis, destruction of minor endometriotic lesions, ovarian biopsy and tubal ligation.
Major laparoscopic surgery included any procedure for which laparoscopic techniques were well codified such as for ectopic pregnancy, pelvic inflammatory disease, polycystic ovary drilling, benign ovarian cysts, distal tuboplasty, moderate to severe endometriosis, extensive adhesiolysis.
Advanced laparoscopic surgery included any procedure whose surgical technique, although codified, required a more complex surgical technique such as myomectomy, hysterectomy, lymphadenectomy, promontofixation for genital prolapse, oncho-surgery with lymphadenectomy, and retroperitoneal endometriosis.
The Inclusion criteria were the availability complete medical records as well as complete post-operatory reports. Data collection was carried out with the use of a pre-tested survey form.
Administrative authorization was obtained beforehand from the Gonesse general Hospital ethics committee. Statistical analysis: Statistical analyses were done using SPSS.19.0 software. The proportions were calculated and compared using the chi-square test. The significance threshold was set at 0.05.
A total of 266 patients were included in the study. The mean age of the study population was 35.78 ± 12.34 years.
The mode was 38 years old and the extreme ages were 14 years for the youngest and 81 years for the oldest patient Figure 1. Concerning the past history, 12.40% of the participants had a history of laparotomy Figure 2.
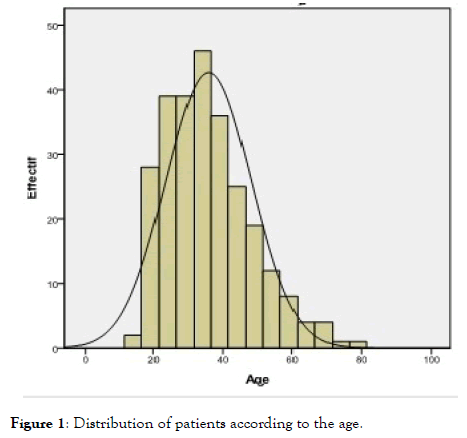
Figure 1. Distribution of patients according to the age.
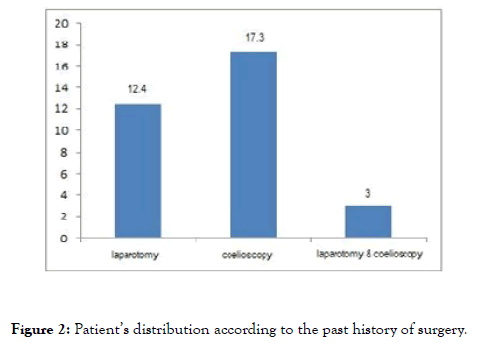
Figure 2. Patient’s distribution according to the past history of surgery.
Almost half of the laparoscopic surgery procedures were performed in the context of an emergency (45.5%) while 54.50% where elective with both ovarian cysts and ectopic pregnancies accounting respectively for 25.19% and 20.30% of the surgical indications as highlighted in Table 1.
| Variables | Effective n=266 | % |
|---|---|---|
| Indications of laparoscopy | ||
| Ovarian Cyst | 67 | 25,19 |
| Ectopic pregnancy | 54 | 20,30 |
| Infertility | 44 | 16,54 |
| Infections | 28 | 10,53 |
| Chronic pelvic pains | 24 | 9,02 |
| Fibroids | 12 | 4,51 |
| Adnexal torsion | 10 | 3,76 |
| Annexectomy | 7 | 2,63 |
| Endometriosis | 7 | 2,63 |
| Tubal sterilization | 7 | 2,63 |
| Migrant IUD | 3 | 1,13 |
| Cancer | 3 | 1,13 |
| Level of laparoscopy | ||
| Major | 156 | 58,6 |
| Advanced | 28 | 10,5 |
| Minor | 35 | 13,2 |
| Diagnostic | 47 | 17,7 |
| Type of complications | ||
| Hemorragic | 9 | 50,0 |
| Digestive | 3 | 16,7 |
| Infectious | 1 | 5,6 |
| Others | 5 | 27,7 |
| Treatment of complications | ||
| Laparoconversion | 12 | 66,7 |
| Observation | 3 | 16,7 |
| Laparoscopy | 2 | 11,1 |
| Antibiotics | 1 | 5,6 |
Table 1: Patient’s distribution according to the indications and type of laparoscopy, type, and treatment of complications.
Major laparoscopic surgery was the most performed type of surgery with 58.60%. The total of both major and advanced laparoscopic surgery made up 69.1% of the overall surgeries and the overall complication rate was 6.70% as shown in Table 1, with the most frequent complication being hemorrhagic in 50% of cases.
Complication-related environment: The history of pelvic surgery or type of laparoscopy amongst the patients of our study population, 33/266 (12.40%) had a past history of laparotomy. Of the 18 complications identified, 4 patients (22.20%) had already been operated on by means of laparotomy. This consisted of 12.10% of complications among patients with a history of laparotomy (4/33). No complication was observed among patients with a history of laparoscopy.
The Complications were mainly observed in patients who had undergone major or advanced laparoscopic surgery this type of surgery made up 184/266 (69.1%) of the sample size.
The higher we progressed on the type of laparoscopy, the more complications we found, and they mostly occurred during the procedure, in 77.8% of the cases. These complications were haemorrhagic in nature in 50% of cases, digestive in 16.7%, infectious in 5.6% and 27.7% were made up of other complications which consisted mostly of surgical difficulties during the procedure thereby prompting a conversion to a laparotomy procedure. The latter was the main recourse when complications occurred in 66.7% (12/18) of cases followed by laparoscopy and antibiotics as shown in Table 1.
When a major laparoscopic procedure was carried out, there was a 9.1 Odds of having complications (p<0.001), as highlighted in Table 2.
| Variables | Complication | |||
|---|---|---|---|---|
| No | Yes | |||
| n (%) | n (%) | OR (95%CI) | p value | |
| History of laparotomy | 29 (11,7) | 4 (22,2) | 3.3 (0.9-11) | 0.053 |
| Level of laparoscopy | ||||
| Advanced | 20 (8,1) | 8 (44,4) | 9.1 (3.2-25) | <0.001 |
| Major | 148 (59,7) | 8 (44,4) | 0.5 (0.2-1.4) | 0.211 |
| Minor | 33 (13,3) | 2 (11,2) | 0.8 (0.2-3.7) | 0.791 |
| Diagnostic | 47 (18,9) | 0 (0) | 0.133 |
Table 2: Association of complications with a history of laparotomy and the level of laparoscopy.
In a previous study carried by Mboudou et al. in Yaounde Cameroon, the mean age of patients undergoing laparoscopy was 31.8 ± 4.9 years, in our study population, the mean age was 35.78 ± 12.34 years [3]. In fact, our sample population was older. In addition to this age difference, there was also a difference in the surgical indications in both studies. In our study, ovarian cysts were the first indication for laparoscopy (25.2%) followed by ectopic pregnancy (20.3%) while in the Cameroonian study, infertility represented 60 to 76.3% of the indications [3-5].
While in our study, infertility was the 4th indication after ovarian cysts, ectopic pregnancy, and pelvic pain. Our results are similar to those found by Pierre F. in France [6] wherein, ovarian cysts were the first indication for laparoscopic surgery (22%) and ectopic pregnancies came in third position (10%) after tubal sterilization. This is because, in France where our study was carried out, infertility does not have the same etiology as in lowincome countries such as Cameroon.
Moreover, in our study, laparoscopic surgery is usually done as first intention unless contraindicated explaining why this procedure was done even during emergencies. The advanced age of the patients could justify not only the predominance of ovarian cysts but also of ectopic pregnancies, which is a complication of the infectious sequelae on the tubes [7,8]. Tubal sterilization is increasingly being replaced by ESSURE tubal ligation and may justify the low rate of tubal ligation in our study sample [9].
We observed a high rate of complications in our study. This was mainly seen when major or advanced laparoscopic surgeries were performed. Our findings are higher than those reported by other studies in the literature [2]. Indeed, the degree of surgical difficulty would be correlated to the risk of complications.
The risk factors found in our study differed from those described by other studies in literature, which were a past history of laparotomy, the complexity of the surgical procedure, the surgeon's experience and morbid obesity [10].
In our study, the past history of laparotomy was not significantly associated with the occurrence of complications due to our sample size, but the complications occurred mainly during elective laparoscopic procedures and increased with its complexity. Similar findings have been reported by Chi et al. [11] and its association with complications in this study could be due to the fact that. Advanced laparoscopic procedures, which had a higher degree of difficulty, were mainly performed electively in that study.
The total rate of complications for all the types of laparoscopy was 6.8% and those requiring laparotomy were 12/18 (4.5%).
The risk of complications was significantly associated with the complexity of the surgical procedure performed. This risk was 0% for diagnostic laparoscopy, 5.7% for minor laparoscopy, 5.1% for major laparoscopy and 28.6% for advanced laparoscopy respectively.
Most of these complications occurred during complex surgical procedures. Johnson et al. published similar results [12] and our results could be explained by the learning curve of our surgeons who were in the initial acquisition phase for some of the complex techniques such as hysterectomies, pelvic prolapse cures, and myomectomies. Complications mainly occurred during interventions and were made up mostly of hemorrhagic complications which were the most frequent in our study, followed by digestive and infectious complications.
Similar results have been found by Shastri et al who concluded that Laparoscopic surgery has many advantages, but it is not void of complications. Despite the rapid improvement of medical technology and surgical skill; complication rates and preventable injuries display a continuous pattern. Delayed recognition and intervention add to morbidity and mortality.
Each laparoscopic surgeon should be aware of the potential complications, how they can be prevented and managed efficiently [13].
Finally, laparotomy was the main recourse when complications occurred. Although several authors have correlated the mode of treatment of complications with the surgeon's experience, laparotomy remains the main recourse in case of severe complications especially haemorrhagic ones [14].
According to Chapron et al., laparoscopic surgical management of complications is increasingly used when the surgeon is very experienced [2].
In conclusion, the complication rate in our study was high and dominated by bleeding during the procedure. Major laparoscopy was significantly associated with the occurrence of complications and was mostly managed by laparotomy.
Citation: Belinga E, Ndoua CCN, Um EJN, Ayissi G, Ntsama JM, Chatour H, et al. (2019) Complications of Gynaecological Laparoscopy and Associated Factors at the Maternity Ward of the Gonesse General Hospital. Gynecol Obstet (Sunnyvale) 9:512. doi: 10.35248/2161-10932.19.9.512
Received: 07-Oct-2019 Accepted: 12-Oct-2019 Published: 19-Oct-2019
Copyright: © 2019 Belinga E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.