Virology & Mycology
Open Access
ISSN: 2161-0517
ISSN: 2161-0517
Case Report - (2022)Volume 11, Issue 1
Background: As India continues to cope with the existing rise in COVID-19 infections, mucormycosis has emerged as a formidable complication in COVID infected diabetics on steroid therapy.
Case presenation: We describe the imaging findings in 6 cases of invasive mucormycosis in sero positive diabetic COVID-19 patients on steroid therapy. Three cases had predominantly varying involvement of the paranasal sinuses with extension into the orbital compartment and 3 were also associated with pulmonary involvement.
Conclusion: Mucormycosis causes aggressive necrosis of the paranasal sinuses extending into the orbit and brain. Pulmonary Necrosis is also common owing to its angio invasive nature. Delay in treatment is often fatal so prompt treatment must be initiated even before histological confirmation using the knowledge of risk factors and characteristic radiological imaging appearances.
COVID-19; Mucormycosis; Bird’s nest sign; Necrosis
DM: Diabetes Mellitus; HTN: Hypertension; HTH: Hypothyroidism; CKD: Chronic Kidney Disease; COPD: Chronic Obstructive Pulmonary Disease
Mucormycosis is a systemic fungal infection caused by members of the class Zygomycetes, order Mucorales. It is seen in patients debilitated by immune or metabolic disorder. Phagocytes are the main defense mechanism against mucormycosis2 by preventing the multiplication of fungal spores. They are inhibited by corticosteroids. Angioinvasiveness with vessel thrombosis and tissue necrosis is characteristic of mucormycosis 3. Uncontrolled diabetes mellitus and the use of corticosteroids for the treatment of COVID-19 infections are the main risk factors in the current scenario.4 Other risk factors are long-term neutropenia, intravenous drug use, malnutrition, stem cell or solid organ transplantation, severe skin damages notably burns and surgical suture sites. COVID-19 had wreaked havoc on the world since the first detected case on December 2019. Of late the situation has been complicated with a rise in the number of confections notably mucormycosis especially in India. Mucormycosis can be life threatening as it has a high mortality rate of over 506%. Recently, chest computed tomography (axial and coronal sections) has given a highly accurate and noninvasive modality of accurately imaging and early treatment of invasive mould pneumonia in immune compromised patients. Final diagnosis of mucormycosis was made based on clinical details, imaging findings, and histopathology. We have come across 6 cases of Invasive Mucormycosis following COVID-19 infection with varying involvement of lung parenchyma; paranasal air sinuses and orbits. Histopathological evaluation of nasal specimen of all 6 cases was done on potassium hydroxide (KOH) wet mount for confirmation.
We retrospectively reviewed six cases of invasive mucormycosis in patients with recent history of seropositive COVID-19 infection admitted to our hospital and managed by department of otorhinolaryngology. Their medical records, clinical data and demographics were reviewed along with radiological and histopathological findings. All the patients were previously treated or currently undergoing treatment for COVID-19 at our hospital and they subsequently developed symptoms namely facial pain, nasal blockage with or without discharge, epistaxis, chemosis and swelling of the eye and even loss vision in one patient. The mean age was 54.1 years (range 42-73 years). 5 of the 6 patients were diabetic. All 6 patients had received steroids for at least 5 days. Remdesivir had also been administered to 5 patients. All the patients bar one had other co-morbidities like hypertension, Chronic Kidney Disease (CKD) and Chronic Obstructive Pulmonary Disease (COPD). Two patients had severe COVID-19 infection while the rest had moderate disease. Contrast enhanced CT of the Paranasal Sinus (PNS) and Thorax revealed thickening of the mucosal of the paranasal sinuses with adjacent bone erosion and even extension into the orbit in some cases. A few cases also revealed a central area of ground glass opacity with irregular intersecting lines surrounded by consolidation referred to classically as a bird’s nest sign [1,2].
Mucormycosis is an invasive fungal infection first described by Paulltauf A in 18858. Even though it can involve different organs the most common type is the rhinocerebral form. In our case series we observed 6 patients with recent history of proven moderate to severe COVID19 infections, 5 of them were diabetic with one having coexisting kidney disease and another suffering from COPD. All of them had received systemic steroid therapy for at least 10 days. CT of the head and PNS region showed infiltration of the left retro antral fat plane Figure 1 which raised the suspicion of it being something other than just a case of simple sinusitis. Complete pacifications of the right maxillary sinus and anterior ethmoidal air cells with internal foci of air without an air fluid level was appreciated and right Ostiomeatal Unit (OMU) was blocked. A small defect was noted in posterior-lateral and infer medial maxillary wall on left side. In one of the cases we found mucosal thickening in bilateral sphenoid and maxillary sinus and left ethmoidal sinus. Irregular outlined soft tissue density lesion seen at infer medial aspect of left orbit and left side of mid cheek anterior to left maxillary antrum (Figure 2). The lesion is communicated within left anterior ethmoid sinus through small bony erosions. Inflammatory changes noted in left retro maxillary region. Both maxillary Ostia are blocked associated with left sided apoptosis. In 2 of our cases we also did HRCT thorax to look for pulmonary involvement. In one case we found a few thick walled cavitation lesions with little residual fibrotic opacity. In another, we found a cavity surrounded by a dense area of consolidation with few intersecting irregular areas of stranding within it resembling the classical reverse halo sign or Bird’s nest sign (Figure 3). Gamba had previously showed that early disease manifested as mucosal thickening on CT scans, usually without air fluid levels10. Silverman described, presence of retroantral, facial and orbital fat stranding indicated the aggressive nature of the infection. On the study done by Sethi H.S, they found peripherally arranged ground glass opacities with surrounding atelectasis changes in all the lobes of bilateral lungs features typical for COVID-19 and mucosal thickening in right ethmoidal and bilateral maxillary sinuses (right>left) with collection in right maxillary sinus with small defect is in posterolateral and infer medial maxillary wall on right side and minimal soft tissue thickening in right orbit abutting inferior rectus muscle with a blocked OMU12.In the study done by Mandeep garg, they found that the most frequent CT findings were consolidation and cavitation, while the ‘reverse halo’ was seen in two patients. All the patients were operated on at the department of otorhinolaryngology and the surgical specimens were sent for histopathology to the department of pathology. In one of our cases on gross specimen we found part of maxilla with necrotic material and congestion throughout the specimen. On H and E stain we found wide areas of necrosis and some fungal elements. PAS stain confirmed mucormycosis by showing broad branching PAS positive fungal hyphae. In the study done by Sunil V Jagtap, they found that areas of inflamed granulation tissue, hemorrhage and congestion. Necrotic areas showed colonies of mucormycosis consisting of broad, non-septate hyphae. The PAS, Grocott’s methenamine silver stain showed fungal hypae of mucormycosis (Figure 4) [3-12].
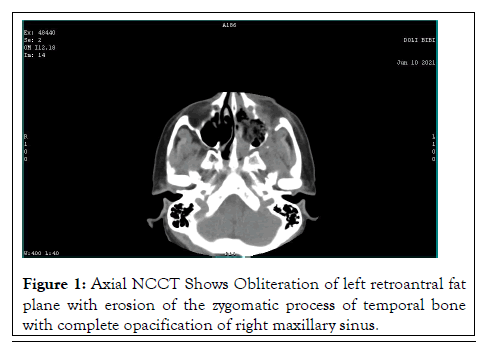
Figure 1: Axial NCCT Shows Obliteration of left retroantral fat plane with erosion of the zygomatic process of temporal bone with complete opacification of right maxillary sinus.
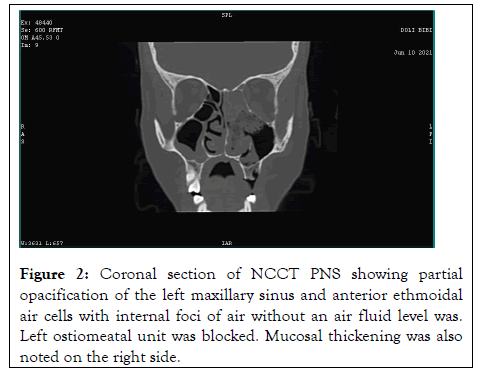
Figure 2: Coronal section of NCCT PNS showing partial opacification of the left maxillary sinus and anterior ethmoidal air cells with internal foci of air without an air fluid level was. Left ostiomeatal unit was blocked. Mucosal thickening was also noted on the right side.
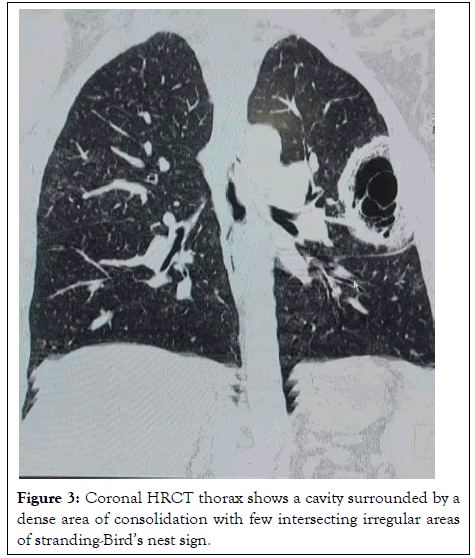
Figure 3: Coronal HRCT thorax shows a cavity surrounded by a dense area of consolidation with few intersecting irregular areas of stranding-Birdâ??s nest sign.
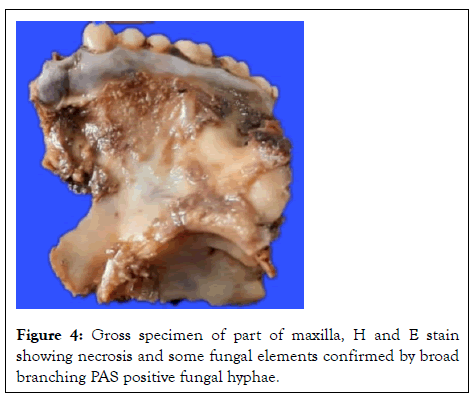
Figure 4: Gross specimen of part of maxilla, H and E stain showing necrosis and some fungal elements confirmed by broad branching PAS positive fungal hyphae.
We propose that, patients with moderate to severe COVID-19 infection with compromised immunity due to diabetes, chronic lung and kidney disease and prolonged systemic steroid therapy are susceptible to mucormycosis because of impairment of barrier defense, dysfunction of phagocytes and lymphocytes. Early diagnosis can be made from imaging features seen on CECT PNS and HRCT thorax which can aid treating clinicians for prompt treatment of secondary fungal infections and substantially reduce morbidity and mortality.
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
[Crossref], [Google Scholar]
Citation: Saha R, Das P, Bhattacharyya S, Karmakar M, Basu SP (2022) Computed Tomographic Findings of Invasive Mucormycosis in Diabetic COVID-19 Patients on Steroid Therapy: Case Report. Virol Mycol. 11: 222.
Received: 30-Dec-2021, Manuscript No. VMID-21-42380; Editor assigned: 01-Jan-2022, Pre QC No. VMID-21-42380 (PQ); Reviewed: 15-Jan-2022, QC No. VMID-21-42380; Revised: 19-Jan-2022, Manuscript No. VMID-21-42380 (R); Published: 26-Jan-2022 , DOI: 10.35841/2161-0517.22.11.222
Copyright: © 2022 Saha R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.