Orthopedic & Muscular System: Current Research
Open Access
ISSN: 2161-0533
ISSN: 2161-0533
Research Article - (2014) Volume 3, Issue 3
This is a retrospective, consecutive, single-surgeon case series which examines the clinical and radiographic outcomes of 19 hips with the incidental finding of hip abductor tears during primary Total Hip Artroplasty (THA). The incidence of abductor tears was 0.68% during our study period from 1994 – 2008. We found that positive preoperative Trendelenburg gait was a positive predictor of the presence of an abductor tear. Seven out of 19 patients had an intraoperative change in surgical approach due to the extent of the abductor tear. Bilaterality and the presence of sclerosis preoperatively were significantly associated with a longer limp period postoperatively. In conclusion, idiopathic abductor tears are rare during primary THA, however there is a high likelihood of changing the intraoperative approach if they are encountered.
Keywords: Abductor tear; Total Hip Arthroplasty
Primary Total Hip Arthroplasty (THA) is the definitive treatment of choice for patients with hip osteoarthritis. This demand is growing due to positive clinical outcomes, and is projected to grow by 174% by 2030 [1]. Patients undergoing primary THA are occasionally found to also have gluteus medius and/or minimus (hip abductors) tears, and surgical repair is often done during the same operation [2]. Limited data is available in the literature about the incidence and clinical outcomes of primary THA patients with idiopathic hip abductor tears.
Hip abductor tears can lead to lateral hip pain, a Trendelenburg gait, and a decreased quality of life, especially in patients with concomitant joint problems [3]. In patients with hip osteoarthritis, gluteus medius and minimus tears are a potential cause of pain in the greater trochanteric region independent of the pain from osteoarthritis, and often go undiagnosed unless identified during THA [2-4].
Howell et al found that 20% of patients who underwent THA for osteoarthritis had degenerative pathology of the abductor mechanism [2]. Bunker et al reported a 22% prevalence of abductor mechanism tears in patients with femoral neck fractures [5] and Hendry et al found the prevalence of abductor mechanism tears in patients undergoing THA to be 25.4% [6]. All three of these studies used a lateral (Hardinge) approach to the hip. When THA was performed using a posteriorlateral approach, Cates et al reported a 1.6% incidence of gluteus medius tears [4].
This retrospective, consecutive, single-surgeon case series examines the clinical and radiographic outcomes of patients who were noted to have hip abductor tears during primary THA. Our aim is to better characterize this unique patient population and report their clinical outcomes. The purpose of this study is to (1) identify the incidence of hip abductor tears at primary THA and (2) describe the radiologic and clinical outcomes following a standardized repair technique.
After approval from our institution’s ethical review board, a retrospective chart and radiographic review was conducted to examine the demographic data, patient characteristics, preoperative factors, postoperative factors, and outcome results of our study group. The senior surgeon’s database was queried for hips undergoing primary THA with the incidental finding of hip abductor tear(s) between 1994 and 2008. All hips that met criteria were included in the study. Data was gathered by reviewing operative data sheets, office visit notes, and radiographs.
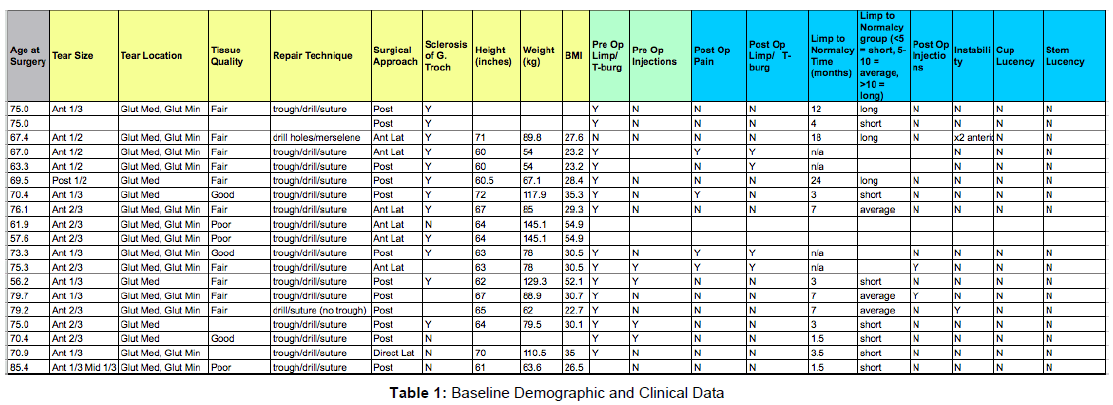
During the study period, 19 hips were identified that satisfied the inclusion criteria. Fifteen of the hips were from female patients. There were 11 left hips in the study. The average age was 71.0 (StDev 7.53; Range 56.2 – 85.4). The average follow-up was 24 months (StDev 21; Range 1-89), and 13/19 hips had a follow-up greater than 12 months. Only 2 of the 6 hips with less than 12 months follow-up did not have adequate time to assess clinical outcomes and were removed from our functional outcomes analysis. Eight hips in the study were from patients with bilateral THAs. See Table 1.
All THA and abductor repairs were performed by the senior surgeon and began with the posterolateral approach. Intraoperatively, the anterior 2/3rd of the gluteus medius tendon was analyzed for tear pathology and if present, was repaired through the posterolateral approach or converted to an anterolateral approach if better access was needed. Of the 19 hips that demonstrated abductor tear pathology, 12 continued the case without modification while 7 were converted to the anterolateral approach.
Surgical Technique
Patients were placed in the lateral decubitus position. A posterolateral approach was attempted and changed to an anterolateral approach if needed for better access depending only on intraoperative findings of size and location of the abductor tear; preoperative findings were not taken into account. Following arthroplasty, the abductor tear was then addressed. The abductor tear was first characterized by location, size of tear, and tissue quality. Initially, the abductor tear was mobilized and a number 5 heavy cotton suture was passed into the torn portion of the tendon in a locking fashion. Following this, the tendon was then freed of adhesions and advanced distally to the bony bed from where it was avulsed from. In the majority of cases, a transverse bony trough was made just proximal to the vastus lateralis ridge. The heavy cotton sutures were then passed through drill holes into the bony ridge by a standard suture passer. The hip was then abducted and the tendon was repaired into the bone trough through a drill hole (See Figures 1 and 2). Closure was performed in a layered fashion and hip abductor precautions were instituted, consisting of no active hip abduction for 3 months and use of assistive device for 6 weeks. Followup appointments recorded pain, gait pattern, presence of limp, hip instability, and component loosening.
Statistical Analysis
Statistical analysis was performed using SPSS software (PASW Statistics 18; SPSS Inc, Chicago, IL) with a two-tailed p ≤ .05 for statistical significance. Data are presented as mean and standard deviations for continuous variables and percentages for categorical variables. Pearson chi-square tests are used for categorical variables to determine if the relationship between crosstabulated variables is statistically significant.
Between 1994 and 2008, a total of 2,800 consecutive hips underwent THA by the senior author. Indications for THA included osteoarthritis (87%), avascular necrosis (8%) and inflammatory arthritis (5%). There were a total of 19 hips with idiopathic abductor tears discovered during primary THA. The incidence of idiopathic abductor tears in hips undergoing primary THA was less than 1% (0.68%). The incidence of idiopathic abductor tears in hip undergoing primary THA for osteoarthritis was 0.78%.
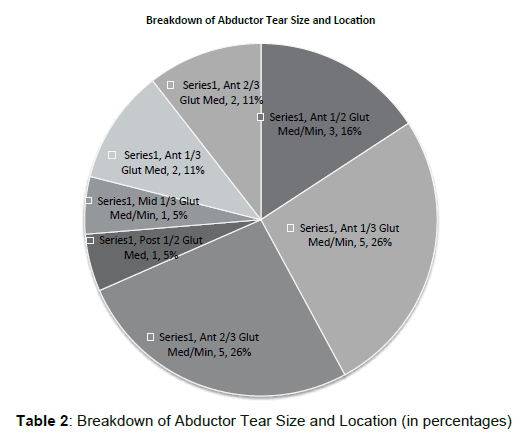
The underlying diagnosis leading to the primary THA was osteoarthritis in all hips with idiopathic abductor tears. Seventeen of the 19 abductor tears were anterior, and more than 50% were either anterior 1/2 or anterior 1/3 gluteus medius and minimus tears. A breakdown of the tear sizes and locations is illustrated in Table 2 below. Tissue quality was determined by intraoperative assessment by the senior surgeon, based on his experience and the ability of the tissue to withstand suturing. Tissue quality was reported as good in 3 cases and fair to poor in 13 cases. Tissue quality of 3 hips was not recorded.
Preoperatively, all patients reported having hip pain and 15 out of 19 patients were noted to have a preoperative Trendelenburg gait. There was no correlation between size, location, or tissue quality of abductor tear with presence of preoperative Trendelenburg gait. At the latest follow up after the procedures, 4 out of 19 patients continued to have hip pain and 4/19 had a positive Trendelenburg gait, while 15/19 patients reported no hip pain and normal gait. One out of 4 patients who received corticosteroid hip injections prior to surgery continued getting them postoperatively, and 3 other patients started receiving them postoperatively. On postoperative AP pelvic and AP/lateral hip x-rays, no patients had any evidence of cup or stem lucency at latest follow up. The average time it took for patients after surgery to have a normal gait (post-op Trendelenburg gait to normalcy) was 7.27 months (Stdev 6.9; Range 1.5-24).
On preoperative AP pelvic x-ray, none of the hips had any evidence of calcification or ossification around the tendinous insertions of the abductor muscles on the greater trochanter. However, 12 out of 19 hips had evidence of sclerosis on the greater trochanter (See Figure 3). A Pearson chi-square test showed that the presence of sclerosis on the greater trochanter was significantly associated with longer limp to normalcy time. In addition, hips from patients with bilateral THAs were significantly associated with a persistent post-operative Trendelenburg gait (p = 0.031). The four cases of persistent Trendelenburg gait all belonged to patients with bilateral THAs. A Pearson chi-square test showed that bilaterality was also significantly associated with longer limp to normalcy time. There was no significant association between age, sex, or presence of preoperative injections and persistence of Trendelenburg gait.
Our study population can be divided into two main groups: those that underwent an intraoperative change in surgical technique from a posterolateral approach to an anterolateral approach (Ant Lat group) and those that did not undergo any changes in approach and continued with the posterolateral approach to the end (Post group). While a significant decrease in incidence of Trendelenburg gait was noted after surgery in our study population, we examined the effect of surgical approach on Trendelenburg gait and found no significant correlation using the Pearson chi-square test (p = 0.639). In addition, no correlation was found between surgical approach and limp to normalcy time.
Two posterior hip dislocations were documented in the follow up period. Both were reduced under general anesthesia without further episodes of instability. No revisions or loosening was identified in any of the components during the study period. One dislocation was from the Ant Lat group and the other from the Post group and there was no significant correlation between surgical approach and dislocation rate.
The current literature has characterized the incidence and patient demographics of THA patients with hip abductor tears. However, limited data are available in the literature describing clinical and radiographic outcomes of these patients after repair. The purpose of our study was to (1) identify the incidence of hip abductor tears at primary THA and (2) describe the radiologic and clinical outcomes following a standardized repair technique.
Bilaterality and the presence of sclerosis were the only variables in our study found to be significantly associated with a longer postoperative limp period. We theorize that the presence of abductor pathology in both hips of patients with bilateral THA makes individual abductor strengthening difficult thereby leading to a longer limp period. Bunker et al. found that the presence of sclerosis on the greater trochanter made reattachment of abductor tendons more difficult and frequently resulted in postoperative weakness and Trendelenburg gait.
Seven out of 19 patients had an intraoperative change in surgical approach to exploit the abductor tear. This has not been previously reported and underlies the importance of hip surgeons utilizing different approaches during THA. No difference in limp to normalcy was found between patients with an intraoperative change in surgical approach and those without a change.
In the current literature, the incidence of idiopathic abductor tears in hips underoing THA using a lateral (Hardinge) approach ranges between 20% and 25.4% while the incidence using a posterolateral approach was found to be 1.6% [2-6]. In our study, the incidence using a posterolateral approach was 0.68%. Hendry et al postulated that when using a posterior approach, a vast majority of low-grade tears are not repaired because they are not identified [6]. Although the single surgeon in this study carefully examined the anterior 2/3rd of each gluteus medius tendon, the comparatively low incidence supports the hypothesis that the posterolateral approach may limit the evaluation of abductor pathology and under report its true incidence. Howell et al found that degenerative tears were more common in women and the prevalence increased with age for both women and men [2]. Our finding that 79% of incidental abductor tears were in women supports Howell et al finding, but we did not establish a correlation between age and abductor tears.
In a survey of French orthopaedic surgeons, Cormier et al showed that gluteal tendon tears are under recognized with only 55% of respondents of the survey even aware that tears could occur in the hip rotator cuff [8]. One reason abductor tears are under recognized is due to the difficulty in diagnosing them. Kagan et al reported no diagnostic findings on physical examination in patients with abductor tears [9] and plain radiographs are typically negative [10, 11]. The Trendelenburg sign is the most sensitive and specific physical sign for the detection of gluteus medius tears [5]. In our study, 15 patients (79%) were found to have a Trendelenburg gait preoperatively. The vast majority of patients who had a preoperative Trendelenburg gait were found to have a normal gait at latest follow-up, with the average limp to normalcy time being 7 months. This underlies the relatively long recovery periods for abductor repairs and appropriate counseling should be performed. A study by Beck et al. showed that one of the rotator cuff muscles of the hip, the gluteus minimus, has multiple actions such as being a flexor, abductor, internal rotator, external rotator, and a stabilizer of the head of the femur in the acetabulum by tightening the joint capsule [12]. Great care should therefore be taken to preserve and reattach all abductor tendons if found to be torn during THA.
Two posterior hip dislocations were documented at latest follow up and were successfully repaired. Osteolysis was another potential complication in our study. Harwin et al reported a 3.7% incidence of osteolysis of the greater trochanter when suture anchors were used for abductor repair in THA [13]. Despite this potential risk, there was no evidence of osteolysis in any of our patients.
The strength of our study lies in its relatively large sample size (19 hips) and its detailed clinical and radiologic evaluation of outcomes after repair. The main limitations of this study are its retrospective nature and lack of control group.
In summary, despite not being a common finding, the importance of recognizing and treating abductor tears cannot be diminished. Understanding the characteristics and outcomes of this unique patient population is of increasing importance since the number of THAs done annually is increasing. Results of this study will hopefully shed light on the issue of the incidental finding of abductor tears during THA and will guide orthopaedic surgeons in repair techniques.