Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2020)Volume 11, Issue 5
This report describe the anatomical and visual outcomes of concurrent pars planavitrectomy (PPV) and Descemet
stripping automated endothelial keratoplasty (DSAEK) for the management of a case with pseudophakic bullous
keratopathy (PBK) and intraocular lens (IOL) dislocation following complicated phacoemulsification surgery.
A 72-year-old woman was referred to our clinic 7 days after complicated phacoemulsification surgery. Severe corneal
edema and IOL dislocation into the vitreous cavity was noticed on examination. After 2 months of conservative
treatment, corneal edema remained persistent, so concurrent 23-gauge PPV, DSAEK and iris supported IOL
implantation were performed in the single surgical procedure.
One year after operation, the cornea was clear, retina was attached and best corrected visual acuity was 20/32. This
report showed that concurrent PPV and DSAEK may be safe and effective option for the management of severely
complicated Phacoemulsification surgery with PBK and IOL dislocation into the vitreous cavity.
Pars plans vitrectomy; Descemet stripping endothelial keratoplasty; DSAEK; IOL dislocation
Cataract is a major cause of visual loss in old patients and cataract surgery is the most common ocular surgery worldwide [1]. Todays, phacoemulsification (PE) has become a surgical procedure of choice for cataract surgery [2], however, it may resulted in different complications including intraocular lens (IOL) dislocation into the vitreous cavity (IOL drop) and pseudophakic bullous keratopathy (PBK). IOL drop may result in cystoid macular edema or retinal detachment and leads to severe visual loss [3].
Dislocated IOL can be managed with pars plana vitrectomy (PPV) and IOL removal with repositioned IOL or exchanged with another IOL [4]; however, clear cornea and clear media are necessary for PPV and IOL management.
In this study we report the surgical outcomes of simultaneous PPV and Descemet stripping automated endothelial keratoplasty (DSAEK) to manage a case of complicated PE surgery with IOL drop and PBK.
A 72-year-old woman was referred to Ophthalmology Clinic of Baqiyatallah Hospital due to complicated PE surgery 7 days after operation. Visual acuity at presentation was hand motion. Slitlamp examination revealed severe corneal edema. Iris defect due to surgical trauma was visible at superior part. Posterior segment was not visible because of severe corneal edema. B-Scan ultrasound was performed and revealed attached retina with dislocated IOL into the vitreous cavity.
Conservative management including topical hypertonic saline, topical steroids, short-time systemic steroid and bandage contact lens was performed. After 2 months of conservative therapy, corneal edema was stable and no improvement in best corrected visual acuity (BCVA) was occurred, therefore surgical management was considered.
Surgical procedure
Surgical procedure was performed under general anesthesia. First, corneal epithelium was removed using surgical blade NO. 15 to improve posterior segment visualization. 23-gauge (23-G) cannula was placed in the inferotemporal quadrant for the infusion port and two 23-G cannulas were placed in the supratemporal and supranasal quadrants. Following core vitrectomy, 0.50 ml of perflurocarbone (PFCL) was injected into the vitreous cavity to transpose the IOL into the mid-vitreous cavity and also, to protect the macula from inadvertent IOL drop during IOL removal. After vitreous base shaving, the dislocated IOL was transposed into the anterior chamber using a 23-G intraocular forceps and removed through limbal incision. Artisan iris-fixated IOL (Ophtec BV, Groningen, the Netherlands) was implanted and the limbal incision was sutured using 10-0 nylon. All 23-G cannulas were removed and sutured.
At the end of vitrectomy procedure, anterior chamber maintainer was implanted at 6 O,clock. Descemet membrane was removed with Sinsky hook and then removed using forceps. Donor cornea (pre-cut by Tehran Eye Bank) was punched 8 mm (endothelium upside). Before folding, a thin layer of sodium hyaluronate 1% was injected on the endothelial surface of donor and then it was inserted into the anterior chamber with Busin-glide from the superior limbal incision that was made for IOL removal and Artisan implantation. The lenticule was opened and centered and the anterior chamber was filled by air completely for 10 minutes, and then was replaced partially (about 50%) with balanced salt solution.
One year after operation, the cornea was cleared, Artisan was in good position, retina was attached and BCVA was 20/32 with a refraction of +0.75 -1.25 × 75 (Figure 1).
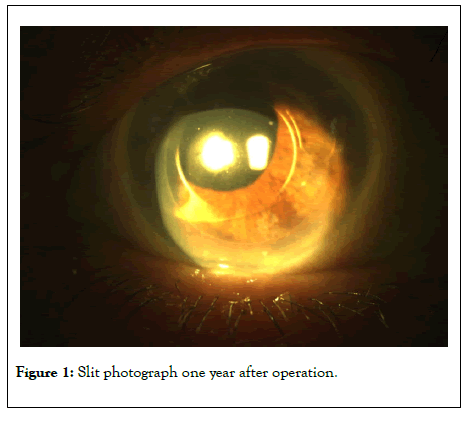
Figure 1: Slit photograph one year after operation.
Here we report a patient with PBK and IOL drop due to complicated PE surgery. Simultaneous PPV and DSAEK with Artisan implantation were done and lead to good anatomical and visual results.
Rauen et al, reported a patient with Fuch,s endothelial dystrophy and previous Neodymium:Yttrium-Aluminum-Garnet (Nd:YAG) laser capsulotomy who underwent DSAEK [5]. 10 days after operation, air bubble was injected into anterior chamber because of DSEAK graft detachment. On postoperative week 4, diagnosis of graft failure and IOL dislocation into the vitreous cavity was made. Concurrent PPV and penetrating keratoplasty (PK) using temporary keratoprosthesis and also, sulcus IOL implantation was performed as a surgical management. One year after operation, BCVA was 20/60 with irregular astigmatism and neurotrophic keratopathy. Unlike Rauen and coworkers, who performed PK combined with PPV, we used simultaneous PPV and DSAEK for the management of PBK and IOL drop with better visual and refractive resu lts. However, corneal edema may have been less in our patient and as a result PPV was possible without temporary keratoprosthesis. Yokogawa and coworkers performed PPV and DSAEK and flanged intrascleral IOL fixation for the management of 3 eyes with PBK and posterior segment problems [6]. They reported that BCVA improved from 20/30 to 20/60 and from 20/600 to 20/130 in two cases however, repeat DSAEK procedure was required in one eye because of endothelial graft detachment. No vitreoretinal or IOL complications including retinal detachment, vitreous hemorrhage or IOL dislocation were reported.
Because it may be difficult and hazardous to perform PPV despite corneal edema, PPV and DSAEK can be done in two separate steps. In this case, DSAEK can be done, and once the cornea had cleared, PPV and management of dislocated IOL were done in the second operation. However, performing PPV and management of dislocated IOL as a second procedure may result in DSAEK graft failure or lenticule dislocation and recurrent corneal edema. Because of high age of the patient and to avoid second surgical procedure we performed PPV with IOL removal and Artisan implantation and DSAEK in the single procedure. We found that PPV can be performed safely after corneal epithelium debridement in cloudy edematous cornea without temporary keratoprosthesis implantation.
This case showed that concurrent PPV and DSAEK may be safe and effective option for the management of severely complicated PE surgery with PBK and IOL dislocation into the vitreous cavity.
Citation: Torabi H, Daryabari SH (2020) Concurrent Pars Plana Vitrectomy and DSAEK to Manage Pseudophakic Bullous Keratopathy and Intraocular Lens Dislocation: A Case Report. J Clin Exp Ophthalmol. 11:853. DOI: 10.35248/2155-9570.20.11.853
Received: 07-Jul-2020 Accepted: 21-Apr-2020 Published: 28-Jul-2020 , DOI: 10.35248/2155-9570.21.11.853
Copyright: © 2020 Torabi H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.