Journal of Phonetics & Audiology
Open Access
ISSN: 2471-9455
ISSN: 2471-9455
Case Report - (2022)Volume 8, Issue 4
Background: A concussion is a mild form of Traumatic Brain Injury (mTBI) caused by a bump, blow, or jolt to the head. The primary injury in a mild concussion is a contusion (bruising) of the brain. But in moderate to severe cases, hemorrhaging (bleeding) of the brain can also occur. The most common causes of concussions are sports injuries, bicycle and car accidents, and falls. The aim of the present study was to use behavioral and electrophysiological assessments to analyse the connection between hearing loss and traumatic brain injury.
Casereport: The current study describes a 27-year-old male cricket player brought to the department with complaint of bilateral hearing loss with no other ontological symptoms. History from the patient stated a hit on the right side of the head while wrestling two weeks ago. Meanwhile, the patient had no hearing problems before the insult.
Conclusion: The patient presented in this case study had gone through multiple tests including Behavioral, Physiological and Electrophysiological evaluation. All the evaluation leads to the conclusion that TBI does have an effect on the auditory system and can lead to hearing loss. The present study highlighted the specific impacts of the TBI on auditory function and therefore, the importance of receiving a full audiological assessment post TBI.
Brain injury; Concussion; Bilateral hearing loss; Audiometry; Consciousness
A concussion is a mild form of Traumatic Brain Injury (mTBI) caused by a bump, blow, or jolt to the head. The primary injury in a mild concussion is a contusion (bruising) of the brain. But in moderate to severe cases, hemorrhaging (bleeding) of the brain can also occur. The most common causes of concussions are sports injuries, bicycle and car accidents, and falls. People who have already sustained one concussion tend to be more susceptible to having another. Although a concussion is not a life-threatening injury and people generally recover quickly, it can cause serious symptoms, including headaches, dizziness, and loss of consciousness, confusion, and fatigue and vomiting. A concussion can affect both hearing and balance [1]. Hearing loss can occur due to physical damage to the peripheral auditory system [2]. Vestibular and balance difficulties, which may include dizziness, vertigo, nausea and visual impairments, after a concussion can occur due to damage to the peripheral or central vestibular systems [3,4].
Concussions have become an increasingly popular medical topic over the last 20 years. Medical specialists have realized that no matter the degree of impact, a concussion can have a wide array of symptoms and negative effects. A neurological evaluation must be performed to measure your sensory and motor responses, including your vision, hearing, balance and coordination. Your brain is a very delicate organ that is protected by the skull. An accident, fall, or sudden impact may result in a concussion or Traumatic Brain Injury (TBI) [5]. Because of the uncertainties regarding mild TBI, the focus should not be on diagnosis. Diagnosis, or rather misdiagnosis, can lead to inappropriate treatment. Mild TBI can be transient in nature, but it can also cause significant disruption in employment, education, and relationships and it should not be minimized. Audiologists should also note that auditory manifestations of TBI can significantly affect treatment and rehabilitation outcomes and are the reason that audiologists should be part of an interdisciplinary approach to TBI care [6].
There have only been a few studies that have aimed at describing the audio logical status of individuals suffering from TBI. The aim of the present study was to examine the hearing status of a cricketer who suffered TBI while playing cricket and to see whether there is a link between TBI and hearing loss. Detailed audio logical evaluation and concussion assessment tests were carried out on the patient [7].
A 27-year-old male cricket player presented to the department with complaint of bilateral hearing loss with no other ontological symptoms. History from the patient stated a hit on the right side of the head while playing cricket two weeks ago. Meanwhile, the patient had no hearing problems prior to the insult. Furthermore, detailed history of the incident revealed that the patient had no apparent skull injuries as observed by temporal bone Computed Tomography (CT) and there was no loss of consciousness. The patient remained in altered sensorium for 12-14 hours. His Glasgow Coma Score (GCS) score upon arrival to the hospital was 13 (E4; M5; V4) and the severity of his concussion was classified as grade II [8].
A detailed case history was obtained followed by which orthoscopic evaluation to visualize the external auditory canal and tympanic membrane status. All the audio logical evaluations were carried out in a sound treated room. Pure tone audiometry was carried out with MAICO MA42 dual channel audiometer. Both air conduction thresholds and bone-conduction thresholds were measured. The thresholds (minimum level of hearing) for air conduction were estimated using standard headphone TDH39 (770 Park Ave, Huntington, NY11743, US), from frequency range 250 Hz to 8 KHz, with intensity level-10 dBHL to 120 dBHL, and the pure tone average was measured using an average of four frequencies, that is 500 Hz, 1 KHz, 2 KHz and 4 KHz. Bone conduction was tested with test frequencies from 250 Hz to 4 KHz, with intensity level from -10 dBHL to 70 dBHL (with standard bone conductor B71, Radio ear). Speech audiometry was performed, including speech reception threshold using spondee words, and speech discrimination score, using phonetically balanced words. Tympanogram and Acoustic reflex thresholds were assessed using GSI Tympstar instrument. Tympanogram was measured using a 226 Hz probe tone, with sweep pressure starts point at -200 dapa to end point of +400 dapa. Ipsilateral and Contralateral acoustic reflex were obtained using pure tone activator stimuli 500 Hz, 1 kHz, 2 kHz and 4 kHz at 90 dBHL, 100 dBHL and 110 dBHL. The patient was instructed to sit quiet and not to move during the procedure. Distortion Product Oto Acoustic Emissions (DPOAEs) were recorded using IHS Jr instrument to check to outer hair cell (OHC) function. Tone pair was sequential, with an F2/F1 ratio of 1.2. Intensity of the tone pairs was 65 and 55 dB SPL for L1 and L2, respectively. Two separate runs per ear were collected for determining repeatability. Validity and reliability of normal outer hair cell function was determined by analysing each distortion product frequency separately. Passing criteria for DPOAE was 6 dB SNR. ABR was measured using IHS Jr. ABR Instrument. Three electrodes were placed on the vertex (non-inverted), the ipsilateral mastoid (inverted), and the contralateral mastoid (ground). Inter electrode impedance was kept below 5 kΩ. The acoustic stimuli were rarefaction clicks with 0.1 ms duration that were delivered monaurally through ER-3A insert earphones presented at a repetition rate of 31.1/sec. Responses to 2048 clicks were preamplifier and band pass between 100-3000 Hz. The analysis time of the screen was set 12 ms. The electrode impedance was regularly monitored. Recording was obtained in a sound proof condition. Duplicate recordings were made to check reproducibility. Absolute latency values of waves I, III and V and interpeak latencies (IPL) of I-III, III-V, and I-V, were measured [9].
Post-concussion tests were administered by a medical professional and the tests included were Post-Concussion Symptom Score (PCSS) and The Standardized Assessment of Concussion (SAC) respectively.
Post-concussion symptom score
One of the most commonly used symptom evaluations is the PCSS. The PCSS includes a battery of concussion-related symptoms (including headache, nausea, vomiting) and a severity scale from 0-6 with 0 being none and 6 being severe [10,11].
The standardized assessment of concussion
The SAC is a five to 10-minute paper and pencil test. It is a neuropsychological assessment tool developed to identify the effects of mild traumatic brain injury on the side-line and does not require specific training in neuropsychology for the purposes of administration or interpretation. The test assesses orientation, immediate recall, concentration, and delayed recall (McCrea, 2001). Performance on each component is summed for a total possible score of 30 with higher scores indicating better functioning.
Otoscopic examination
Otoscopic examination revealed bilateral cone of light present with no other abnormalities present for the ear canal and tympanic membrane.
Pure tone audiometry
Pure tone audiometry revealed bilateral mild to moderate sensor neural hearing loss results are shown in Figure 1.
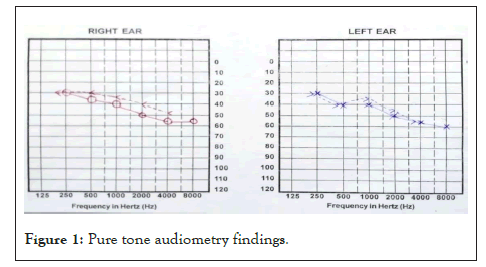
Figure 1: Pure tone audiometry findings.
Speech audiometry
Speech recognition threshold (SRT) and Speech Discrimination Score (SDS) results are shown in Table 1.
| Ear | SRT | SDS |
|---|---|---|
| Right ear | 45dBHL | 85% |
| Left ear | 45dBHL | 85% |
Table 1: Speech audiometry results.
Immittance and reflexometry
Bilateral ‘A’ type tympanogram with ipsilateral reflex present at 500 Hz and 1000 Hz and absent contralateral relexes suggestive of no middle ear pathology (Tables 2 and 3).
| Measures | Right | Left |
|---|---|---|
| Tympanogram type | A | A |
| Ear canal volume | 1.6 cc | 1.8 cc |
| Static compliance | 1.5 ml | 1.7 ml |
| Peak pressure | 10 dapa | 9 dapa |
Table 2: Immittance and reflexometry results.
| Reflexometry results | Frequency (Hz) | |||
|---|---|---|---|---|
| 500 | 1000 | 2000 | 4000 | |
| Right ipsi | 100 | 105 | NR | NR |
| Right contra | NR | NR | NR | NR |
| Left ipsi | 100 | 105 | NR | NR |
| Left contra | NR | NR | NR | NR |
Table 3: Reflexometry and frequency results.
Oto acoustic emission
Distortion product oto acoustic emission revealed bilateral absent oae’s suggestive of outer hair cell dysunction (Figure 2).
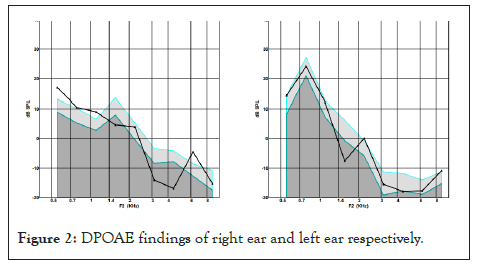
Figure 2: DPOAE findings of right ear and left ear respectively.
Auditory brainstem responses
Revealed bilateral clear and replicable Vth peak obtained till 50 dBnHL which leads to the impression mild to moderate hearing loss (Figure 3). The absolute latencies of wave III and V as well the inter peak latenices I-V was found to be prolonged in both the ears.
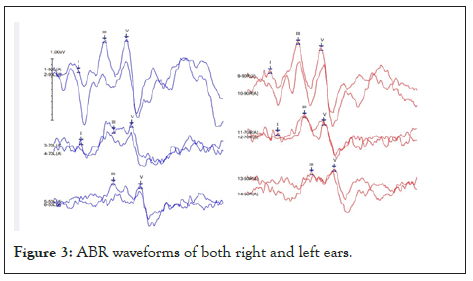
Figure 3: ABR waveforms of both right and left ears.
Post-concussion assessment
Post-Concussion Symptom Score showed a Total PCSS score: 46/132=34.8% which indicate presence of mild concussion symptoms.
The Standardized Assessment of Concussion showed an overall score of 20/30 (higher scores indicates better functioning).
Hearing loss often happens in conjunction with other invisible injuries, such as traumatic brain injury, or TBI. Hearing and balance issues are often overlooked in polytrauma patients because other visible wounds often take medical priority. Still, hearing loss may mask or confuse the correct diagnosis of other injuries. For example, a TBI patient could be misdiagnosed as unresponsive when hearing loss is present. Given the interconnectedness between hearing loss and other invisible injuries, it’s important to understand each condition.
An undiagnosed case of hearing loss can interfere with the effectiveness of medical care and rehabilitation for TBI patients. Auditory problems could be mistaken for signs of cognitive deficits attributed directly to TBI. Factors associated with both hearing loss and TBI, such as attention, cognition, neuronal loss, and noise toxicity, can lead to misdiagnosis. Hearing loss may also exacerbate the social, emotional, and cognitive effects of TBI. Also n mild cases, standard neuroimaging is unlikely to find structural brain damage.
Audiological findings in patients with TBI are extremely rare. However, hearing impairment may result from alterations in any part of the auditory pathway (external ear, middle ear, inner ear, cranial nerve, trunk, or subcortical and cortical regions). TBI can cause a series of hearing losses that may include cochlear losses, vestibular alterations, and central auditory modifications.
In the present study the pure tone audiometry revealed bilateral mild to moderate sensorineural hearing loss. Hearing in 60 subjects with head injury and found out that On the type of hearing loss, 8 cases (13.3%) has normal hearing bilaterally, and 34 cases (56.6%) of bilateral sensorineural, 9 cases (15%) of bilateral or unilateral mixed, and 3 cases (5%) of unilateral conductive hearing loss were observed. Similarly Chen et al. in their study also reported that Hearing loss after TBI in the absence of bony injury appears to be a clinically significant but poorly characterized phenomenon.
Tympanometry results showed Bilateral ‘A’ type tympanogram with ipsilateral reflex present at 500 Hz and 1000 Hz and absent contralateral relexes suggestive of no middle ear pathology. Olusola, Emmanual and Olatundun (2019) in their study revealed that in most of the subjects tympanometric measures revealed type A (normal) tympanograms in 27 (50.9%) ears, type B tympanogram in 11 (20.8%), and type C tympanogram was found in 10 (18.9%) ears. Acoustic reflex was absent in 33 (62.3%) of the ears.
DPOAE evaluation revealed bilateral absence of OAEs and similar findings were seen in a study by Emerson et al., who reported in case of mild hearing loss on PTA, there was absence of emissions in 70% at 1000 Hz, 69% at 2000 Hz, 83% at 4000 Hz. They also suggested that damage to outer hair cells becomes more pronounced when there is manifest hearing loss on PTA.
Auditory brainstem responses revealed mild to moderate hearing loss with prolonged absolute latencies of wave III and V as well as inter peak latencies of I-V in both ears. Similar findings in this study on 290 participants with TBI which showed positive associations between the severity of TBI and prolonged Waveform V and I-V interweave latencies. The findings of their study indicate the involvement of the brainstem as a direct consequence of the severity of TBI [12].
Results of the current study revealed that the majority of participants with mTBI may experience auditory dysfunction in the peripheral and central auditory systems, regardless of the number, type, and severity of the TBI(s). The present study highlighted the specific impacts of the TBI on auditory function and therefore, the importance of receiving a full audio logical assessment post TBI. This is essential for planning interventions aimed at returning to daily living activities, such as work, school, and leisure. Interventions could be tailored for each patient according to the specific auditory dysfunction, thereby increasing the chances of improving the quality of life for patients after a brain injury. Hence all the patients with Minor head injury should undergo detailed audio logical evaluation even if they do not complain of hearing loss.
[Crossref][Google scholar][PubMed].
[Crossref][Google Scholar][PubMed].
Citation: Nithin AK, Swati SSJ, Mustafa F (2022) Concussion and Associated Hearing Loss in a Cricket Player: A Single Case Study. J Phonet Audiol. 8:179.
Received: 04-Jul-2022, Manuscript No. JPAY-22-18203; Editor assigned: 06-Jul-2023, Pre QC No. JPAY-22-18203 (PQ); Reviewed: 21-Jul-2022, QC No. JPAY-22-18203; Revised: 26-Jul-2022, Manuscript No. JPAY-22-18203 (R); Published: 08-Aug-2022 , DOI: 10.35248/2471-9455.22.8.179
Copyright: © 2022 Nithin AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.