Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2021)
Localized scleroderma; Morphea; Neonatal; Congenital; Connective tissue disorder
Scleroderma is a spectrum of disorders characterized by thickening of the skin and subcutaneous tissue with increased collagen deposition. The two clinical patterns are systemic sclerosis and localized scleroderma (Morphea). The latter is ten times more common in children than systemic sclerosis [1].
The incidence of morphea is generally estimated to be 0.4 to 2.7 per 100,000 people with a female: male ratio of (2 to 3:1) [2]. A study in the UK and Ireland estimated an incidence rate of 3.4 cases per million children per year aged ≤ 16 years [1]. Morphea can be divided into several clinical subtypes, including circumscribed (with superficial and deep variant), Linear (with trunk/limb variant and head variant), generalized, pansclerotic and mixed type [3]. Linear morphea is the predominant form of localized scleroderma in childhood. Extra-cutaneous manifestations occur in over 20 percent of children with Localized scleroderma [4]. Congenital Localized Scleroderma (CLS), a form of morphea that presents at birth, is exceedingly rare and few cases have been reported in the literature to date [5,6].
Patients with morphea have demonstrated periods of inactivity or quiescence followed by reactivation of the inflammation, induration, and tissue loss that characterize the disorder [7]. Diagnosis is often delayed by several years, probably because the lack of awareness of the condition and its similar initial morphology to other skin lesions [5]. Little is known about CLS clinical presentation and disease progression. Previously reported cases showed that it might be progressive and might be associated with a clinically profound extra-cutaneous involvement, which necessitate early diagnosis and treatment [5,6]. Here we describe a case with a unique presentation of CLS that was noticed since birth.
A 2-month-old baby girl, full term, a product of normal spontaneous vaginal delivery presented to the dermatology clinic at King Abdullah Specialized Children’s Hospital in Riyadh, Saudi Arabia, with a skin lesion that was noticed at birth and described by the parents as lightly pigmented patch over the left forehead, almost 2 × 3 cm, with a central depression shown in Figure 1. Patient was referred to Pediatric Rheumatologist in the same hospital based on suspicion of localized scleroderma.
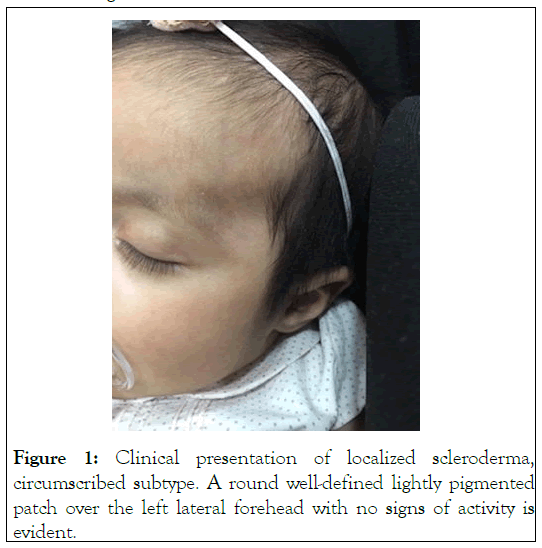
Figure 1: Clinical presentation of localized scleroderma, circumscribed subtype. A round well-defined lightly pigmented patch over the left lateral forehead with no signs of activity is evident.
Patient was thriving well with no associated systemic symptoms. There was no history of extra-cutaneous involvement such as ocular, neurologic or osteoarticular involvement. In regards to pregnancy and labor, a comprehensive clinical history was obtained and revealed unremarkable findings as no medications, infections, or other factors potentially involved in the disease onset. No family history of similar presentation, rheumatological or autoimmune diseases.
Upon physical examination, the baby was looking well, vital signs were normal with normal systemic examination. The skin lesion appeared as a slightly hyperpigmented oval patch, hypotrophic in its center but with mildly indurated borders. No skull depressions or other skin lesions were noticed.
The initial laboratory workup including, CBC, CRP, ESR, liver and renal profile, were normal. ANA test was negative. A skin biopsy was obtained and showed thin epidermis with epidermal pigment incontinence, along with mucin deposition, patchy perivascular lymphocytes and mild fibrosis, indicating fibrotic disease process which is consistent with the diagnosis of scleroderma shown in (Figures 2 and 3). The mucin deposition was highlighted by the use of Alcian blue stain. The diagnosis of CLS, circumscribed subtype, was made. Further evaluation by facial cone beam CT (CBCT) scan and Brain MRI were done and revealed normal results. Furthermore, she was referred to ophthalmology with a normal ocular examination.
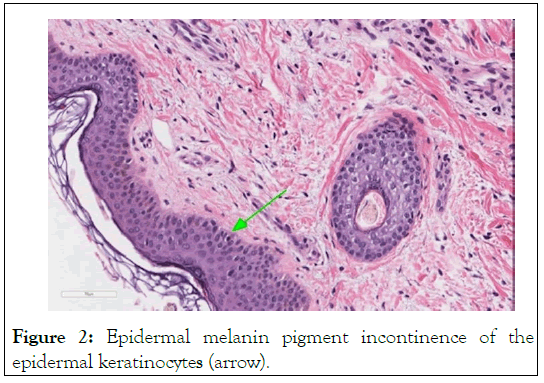
Figure 2: Epidermal melanin pigment incontinence of the epidermal keratinocytes (arrow).
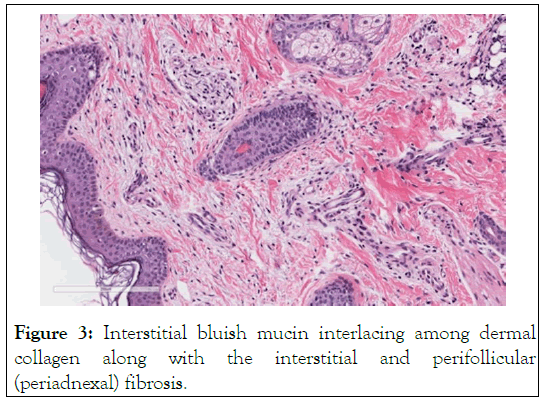
Figure 3: Interstitial bluish mucin interlacing among dermal collagen along with the interstitial and perifollicular (periadnexal) fibrosis.
Patient was started on Topical Tacrolimus 0.1% ointment to be used twice daily. Skin lesion did not progress. After 12 months of follow-up, the lesion was stable in size with no signs of activity in terms of expansion or induration. Indeed, no other lesions in the face or in other part of the body were noticed. Infrared thermography and CBCT scan confirmed the inactive state of the disease.
CLS is a rare and probably underestimated condition in neonates that it might take around 4 years for the patients to be correctly diagnosed [6]. The delay in the diagnosis can be accredited to the lack of awareness in appreciating localized scleroderma in the newborns/infants and its similar initial morphology to other skin lesions [5]. Initial diagnostic considerations of common congenital conditions include congenital melanocytic nevus and Café-au-lait macule. Mastocytosis (urticaria pigmentosa) may also present in the neonatal period but it has a characteristic morphology. Lesions of mastocytosis usually become urticated, edematous upon rubbing or scratching the lesion (darier sign).
CLS in our case was of a circumscribed type, which is slightly in contrast to what has been already reported in the literature. Previous studies showed high proportion of congenital linear morphea [5]. Given the underestimation and under diagnosis of the condition, its activity and lesion location suggest that the case we are reporting here may be part of a full spectrum of congenital cases [5].
Localized scleroderma lesions have the potential to become active despite their quiescence nature at the time of diagnosis, necessitating long‐term follow‐up. We suggest a possible theory that CLS might have started early during pregnancy and now the lesion might be in a quiescence\inactive stage. Possible triggers during pregnancy including, but not limited to, viral infection, hormonal changes or medications in a predisposed individual. Early recognition in infancy is essential and monitoring over time for any signs of reactivation to minimize the life‐long complications [5]. Given the rarity of the congenital form of morphea, reactivation has not yet been reported in the literature. However, in the pediatric-onset morphea, particularly the linear subtype, reactivation has been reported to occur in 27% of patients [5]. The patient herein reported is still being followed up and the lesion is monitored for any signs of activity.
This case report represented a diagnostic challenge and suggests that CLS should be considered in the differential diagnosis of neonates or infants with cutaneous erythematous to lightly pigmented fibrotic lesions to avoid delay in the diagnosis which could lead to functional and cosmetic consequences and allowing for prompt therapy.
We thank Dr. Nada Shokor for providing histopathology pictures.
The authors declare no conflict of interest.
No Funding Sources is relevant to the study.
Citation: Alajroush W, Al-Marzoug A, Bayazeed L, Al-Rasheed A, Alqahtani N, Zulian F, et al (2021) Congenital Localized Scleroderma: A Rare Presentation in a Newborn Baby. J Clin Exp Dermatol Res. S10:573.
Received: 23-Jul-2021 Accepted: 06-Aug-2021 Published: 13-Aug-2021 , DOI: 10.35248/2155-9554.21.s10.573
Copyright: © 2021 Alajroush W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.