Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2022)Volume 12, Issue 2
A healthy newborn baby girl was born with caesarean section due to fetal bradycardia around the time of delivery and aspiration of meconium and amniotic fluid into the lungs was detected and tracheal suction was used to clear the airways of meconium in addition supplemental oxygen was needed. The portosystemic shunt problem was detected and congenital portosystemic venous shunts are rare vascular anomalies that occurred to be a secondary abnormal development or involution of fetal vasculature. At week 36 the mother underwent amniocentesis which was normal. After birth the neonate transferred to the nursery to be under observation due to events of hypoglycemia and hyperbilirubinemia. Normal ammonia and normal coagulation functions was detected. Radiological finding were postpartum ultrasound of the liver and bile ducts of upper abdomen showed evidence of liver and gallbladder with normal dimensions and epigyny and normal bile ducts. Laboratory findings were glucose was 50 mg/dL at first and later ranged from 75 to 100 mg%, blood gases were normal PH 7.3-7.4, Normal Bicarbonate 22-24, O2 saturation were 96%, normal electrolytes including normal calcium potassium and sodium normal thyroid function, normal Blood Proteins Albumin 4.2 mg/dL, CPK was 200 (mcg/L).
Infant; Portosystemic shunt; Cardiovascular; Hepatic vein; Hypoglycemia; Vein
Portosystemic shunt is also known as a liver shunt, is a bypass of the liver by the body’s circulatory system. It can be either a congenital or acquired condition.
Congenital Portosystemic Venous Shunts (CPSVS) are rare vascular anomalies that occur secondary to abnormal development or involution of fetal vasculature.
Congenital portosystemic shunts can be divided into two types: Intrahepatic shunts and less commonly the extrahepatic type. It occurs with a prevalence estimated to be in the range of 1 in 30,000 births. CPSVS are associated with multiple congenital abnormalities, most commonly involving the cardiovascular system [1]; however, their association with biliary, urogenital, and gastrointestinal anomalies as well as some syndromes has also been described. We report a unique case of a neonate with an intrahepatic congenital portosystemic venous shunt.
Extra hepatic CPSS were antecedently referred to as Abernethy malformations. CPSS are generally characterized into Intrahepatic (IH) and Extrahepatic (EH). This distinction has relevancy as a result of extra hepatic shunts seldom shut impromptu, while intrahepatic shunts appear a lot of liable and decreasing their clinical significance. The persistent Patent Ductus Venosus (PDV), although considered as ANIH shunt, is unlikely to shut impromptu when 1-3 months getting on, and therefore is usually enclosed within the class of EH CPSS [2]. CPSS will go unperceived for an extended time, and many conditions, that multiple functions of the liver. Infant acholia, liver tumors, Hepatopulmonary Syndrome (HPS), pneumonic blood vessel cardiovascular disease (PAH), high output cardiac failure, hyperinsulinemic symptom, hyperammonemia, hyperandrogenism, precocious pubescence, tall stature, amenorrhea, adenosis, macrohematuria and neurocognitive disorders are very recent empirical.
The accumulative incidence of a minimum of one major EH CPSS manifestation (hepatic brain disorder, PAH, HPS, hepatoma or adenoma) at 25, 30, 40 years getting on was 35, 45, 58, severally. Early liver physicist of USA permits for prompt management of doubtless serious manifestations, ultimately up the result in these patients [3]. Therefore, the aim of the current article is to expand on 3 cases with variable shows to debate the severe clinical consequences of CPSS. Clinical presentation and initial designation, with a quick summary of management for the final medical specialist, so as to extend awareness within the medicine community and reduce diagnostic delay.
A healthy newborn baby girl was born with caesarean section due to fetal bradycardia around the time of delivery, aspiration of meconium and amniotic fluid into the lungs was detected and tracheal suction was used to clear the airways of meconium in addition supplemental oxygen was needed. In the first examination after birth the Apgar score was around 7-8. History was taken from the parents, and the prenatal history showed that the neonate was born to a 44 year old religious mother. No frequent fetus scan was done during gestational period at week 35 due to premature contraction celestone was given to the mother. At 36th week the mother underwent amniocentesis which was normal. After birth the neonate transferred to the nursery to be under observation due to events of hypoglycemia and hyperbilirubinemia. Thrombocytopenia appeared on repeated blood tests.
Complete chemistry includes normal blood clots was normal. Normal physical examination except for the impression of slightly short limbs in relation to the body, forehead prominent (frontal boosing), enlarged liver and spleen. On auscultation lungs were clean, regular heart sounds no murmur checked. Cardiac echo was normal. Due to thrombocytopenia, a sepsis examination was performed which was negative and antibiotic treatment discontinued after receiving negative blood cultures, Urine examination was also sent to detect CMV which was negative in addition kidney and urological system without any anomalies or pathology.
Metabolic clarification was done due to episodes of hypoglycemia and was normal. In light of cholestatic jaundice with high levels of direct bilirubin, Ursolit treatment was applied, abdominal ultrasound showed evidence of normal anatomy of liver, bile ducts, gallbladder, and pancreas, portosystemic hepatic shunt was detected, and a communication was demonstrated with curling and dilation of the hepatic vein and its small branches with mixed flow of the two veins attachment at two points. Normal ammonia and normal coagulation functions were detected (Figure 1).
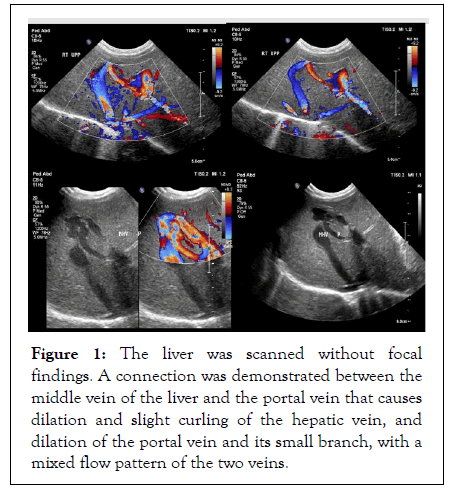
Figure 1: The liver was scanned without focal findings. A connection was demonstrated between the middle vein of the liver and the portal vein that causes dilation and slight curling of the hepatic vein, and dilation of the portal vein and its small branch, with a mixed flow pattern of the two veins.
Vein and the branch of portal vein brain ultrasound were done and it showed normal results. At the age of six months the child was asymptomatic and stable, a repeat ultrasound and significant improvement was seen minimal shunt between the portal vein on the left and the hepatic vein, and it was in the closing process. Last laboratory showed normal ammonia levels, Gases PH7.36, Hepatic function SGOT18 units/L SGPT35 units/L, hemoglobin was stable 13, normal platelets 250,000, 10000 normal leukocytes.
The patient continued to undergo Pediatric Gastroenterology, and Pediatric surgery follow-up at Schneider Children's Medical Center in Israel.
Radiological finding: Postpartum ultrasound of the liver and bile ducts of upper abdomen showed evidence of liver and gallbladder with normal dimensions and ecogyny and normal bile ducts [4]. A shunt has been demonstrated that shows a connection in the middle vein of the hepatic vein and the portal vein, which causes dilation and slight curling of the hepatic vein.
Laboratory findings: glucose was 50 mg/dL at first and later ranged from 75 to 100 mg%, Blood gases were normal pH 7.3-7.4, Normal Bicarbonate 22-24, O2 saturation 96%, normal electrolytes including normal calcium potassium and sodium normal thyroid function, normal Blood Proteins Albumin 4.2 mg/dL, CPK was 200 (mcg/L), Liver function was disturbed SGOT 180 units/L, dropped to 35, SGPT 60 units/L Which dropped to 30 later [5]. Normal ammonia 38 μmol/L. follow up one month after discharge from our hospital, Radiological finding showed The Porto-systemic shunt was detected by fetal ultrasound and verified after birth Intra-hepatic portosystemic shunt is still observed between the middle hepatic [6].
The Portosystemic shunt could be a clinical reality of undetermined being the foremost frequent reason for viscous. The absence of partial reabsorption of the viscous membrane throughout the portosystemic shunt development and failure of it venous blood vessel within the perinatal amount, the maturity being periodically. Once family cases area unit reported, however, they occurs to be in isolation, no mutations or genetic markers were known within the majority of cases, a liver shunt is caused by a congenital abnormality known as a non-inheritable portosystemic shunt. In some cases, multiple tiny shunts type owing to severe disease like cirrhosis of the liver. These area unit said as noninheritable portosystemic shunts. Non-inheritable portosystemic shunts (CPSS) area unit rare noninheritable, abnormal blood vessel communications between the portal blood vessel system and therefore the circulation poignant associate calculable 1,40,000 to 1,50,000 newborn infants. The hymen ought to be evaluated at birth, at which period the newborn infant might have salient shunt membrane and the presence of hydrometrocolpos. The clinical manifestations of this anomaly are often serious, together with Hepatopulmonary Syndrome (HPS), which might result in important hypoxemia and symptom.
This case illustrates some of the presentations of CPSS in newborn infant: liver nodules, neurocognitive difficulties, and PAH and possibly tall stature. Liver Doppler US is the key todiagnosis. Considering CPSS in the diagnostic work up of a patient with a complex clinical picture of unexplained endocrine, liver, gastro-intestinal, cardiovascular, hematological, renal or neurocognitive disorder is important, as prompt referral to a specialized center may significantly impact patient outcome. The diagnosis of portosystemic shunts is often challenging and requires a high degree of clinical suspicion. Spontaneous closure of CPSS can occur in some anatomic forms during the first year of life. However, in instances where spontaneous closure does not occur, radiologic or surgical closure is recommended to prevent, resolve and/or stabilize complications. Upon discovery of a CPSS in a child, it is important to rule out portal hypertension or hepatic hemangioma as the cause of the shunt, either of which would require a specific treatment. Once the congenital, and isolated, nature of the shunt has been ascertained, closure by surgical intervention is usually recommended.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Nasser B, Jerdev M, Nasse H, Nasse W (2022) Congenital Portosystemic Shunts in Neonate: A Case Report. Pediatr Ther. 12:439.
Received: 07-Feb-2022, Manuscript No. PTCR-21-15249; Editor assigned: 10-Feb-2022, Pre QC No. PTCR-21-15249 (PQ); Reviewed: 21-Feb-2022, QC No. PTCR-21-15249; Revised: 28-Feb-2022, Manuscript No. PTCR-21-15249 (R); Published: 07-Mar-2022 , DOI: 10.35248/ 2161-0665.22.12.439
Copyright: © 2022 Nasser B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.