Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Case Report - (2022)Volume 15, Issue 9
Kawasaki disease is well known and widely prevalent acute febrile illness and systemic vasculitis of unknown aetiology that usually and predominantly afflicts children of younger age group usually below 5 years. Its coronary presentations are usually coronary artery aneurysms and can result in long-term cardiovascular sequelae. Kawasaki disease is the leading cause of acquired heart disease among children in the Pacific region. Sometimes coronary artery aneurysms developed in some untreated children with Kawasaki disease, might lead to ischaemic heart disease and myocardial infarction. Early treatment with Intravenous Immunoglobulin (IVIG) might reduce the risk of development of coronary artery aneurysms, several cases have been reported to have IVIG resistant Kawasaki disease and are at increased risk of developing coronary artery damage. Besides, lack of specific diagnostic tools and biomarkers for Kawasaki disease make early diagnosis and treatment challenging. Though Kawasaki Disease is prevalent in more than 60 countries, including Asia, the Middle East, Latin America, and Africa, as well as in North America and Europe it still found centered on Japan in Pacific region. Coronary involvement is a common and most serious complication that usually presents in later stage of disease progression. The purpose of this review is to report a case of Kawasaki Disease and describe the coronary presentation of Kawasaki Disease.
Kawasaki diseases; Aetiology; Aneursysm; Intavenous Immunoglobilin (IVIG)
Kawasaki Disease (KD), named also mucocutaneous lymph node syndrome, is an acute systemic febrile vasculitis. Several theories for the pathophysiology of the condition have been proposed, but the aetiology of KD remains unknown. It was first described in in 1967 by Tomisaku Kawasaki in Japanese children. Although it has highest incidence in Japan and Japanese American population, 134-135 per 1,00,000 children, it has universal distribution all over the world from different races and ethnicities. It is a kind of necrotising vasculitis of medium sized arteries and with predilection for the coronary arteries. The diagnosis of the disease relies on clinical signs and symptoms. Because of these signs overlap with many common paediatrics febrile illnesses, it can be challenging to identify KD. Criteria of KD diagnosis are ≥ 5 days of fever and adding; least four of the five following bilateral non-purulent conjunctivitis, rash, extremity changes, cervical lymphadenopathy, and mucocutaneous changes. In atypical cases, patients with fewer and fewer principal symptoms can be called KD when coronary artery disease is detected. Kawasaki disease can result in a variety of cardiac and noncardiac complications. Kawasaki disease is the leading cause of acquired heart disease in children and can effect children at any age, but 85% of cases occur under the age of 5 years. The commonest and most life threatening complication of KD is the development of coronary artery aneurysm. In untreated KD, up to 25% of patients have coronary artery aneurysm and most of them develop within 6-8 weeks from the onset of the illness. A small number of coronary artery aneurysm result in coronary thrombosis and lead to risk for future ischemic heart disease, myocardial infarction, and sudden death. A life threating malign KD sequelae is Kawasaki shock syndrome, which KD with associated systolic hypotension, or other signs of poor perfusion.Less common KD cardiac complications include myocarditis, pericarditis, congestive cardiac failure, pericardial effusion, aortic of mitral regurgitations due to myocardial involvement and arrhythmias. Children with incomplete KD are more likely to experience treatment delays and the development of coronary artery disease.Treatment within 10 days of illness onset with intravenous immunoglobulin and aspirin has proven effective in dramatically reducing the risk of cardiac complications; but, approximately 20% of patients with KD might not adequately respond to this treatment and may require a second dose of IVIG or alternative medications, such as steroids.
Coronary artery aneurysm and most of them develop within 6-8 weeks from the onset of the illness. A small number of coronary artery aneurysm result in coronary thrombosis and lead to risk for future ischemic heart disease, myocardial infarction, and sudden death. A life threating malign KD sequelae is Kawasaki shock syndrome, which KD with associated systolic hypotension, or other signs of poor perfusion. Less common KD cardiac complications include myocarditis, pericarditis, congestive cardiac failure, pericardial effusion, aortic of mitral regurgitations due to myocardial involvement and arrhythmias. Children with incomplete KD are more likely to experience treatment delays and the development of coronary artery disease. Treatment within 10 days of illness onset with intravenous immunoglobulin and aspirin has proven effective in dramatically reducing the risk of cardiac complications; but, approximately 20% of patients with KD might not adequately respond to this treatment and may require a second dose of IVIG or alternative medications, such as steroids
We describe here a 23 years-old IT professional of Japanese Nationality with no cardiovascular risk factor and history of hospitalisation 2 years back for fever of 6 weeks duration, accompanied by generalised erythema and musculoskeletal pain. Following various examinations and blood tests that revealed thrombocytosis, hypoalbuminemia, an abnormal liver profile, and elevated erythrocyte sedimentation rate and C-reactive protein, the patient was diagnosed as Kawasaki Disease and discharged after recovery. Two years later he was readmitted for exertional angina.Subsequent Coronary angiography showed severe diffuse disease of the entire coronary vasculature with multiple aneurysm (Figures 1-4).
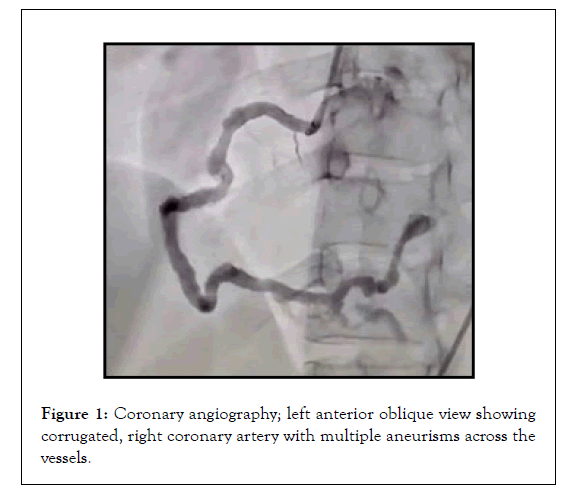
Figure 1: Coronary angiography; left anterior oblique view showing corrugated, right coronary artery with multiple aneurisms across the vessels.
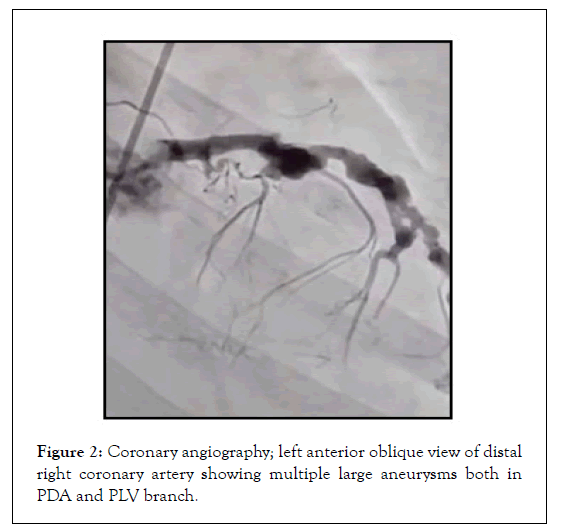
Figure 2: Coronary angiography; left anterior oblique view of distal right coronary artery showing multiple large aneurysms both in PDA and PLV branch.
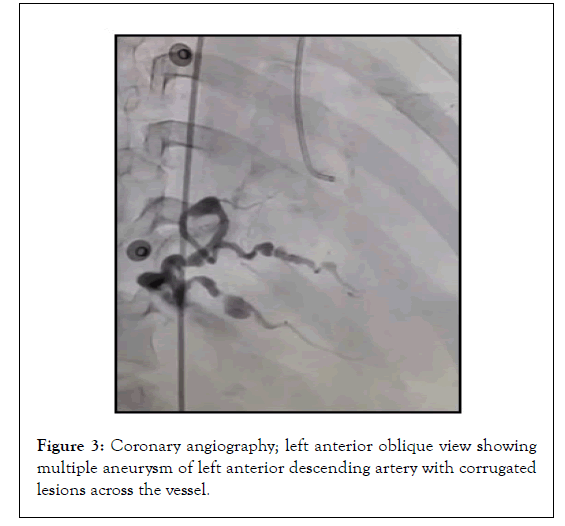
Figure 3: Coronary angiography; left anterior oblique view showing multiple aneurysm of left anterior descending artery with corrugated lesions across the vessel.
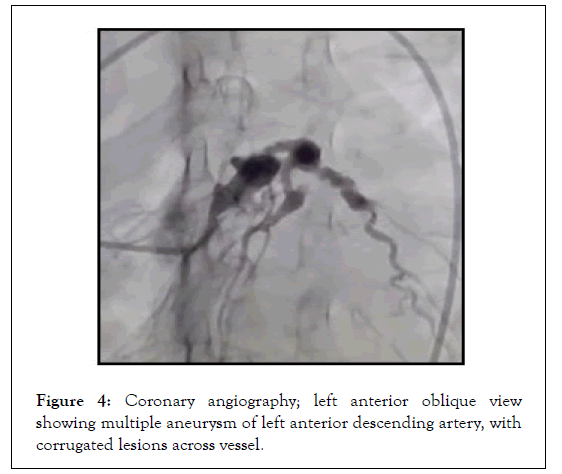
Figure 4: Coronary angiography; left anterior oblique view showing multiple aneurysm of left anterior descending artery, with corrugated lesions across vessel.
The clinical symptoms and findings led to confirmation of diagnosis of Kawasaki Disease that had was made in the acute phase 2 back. Treatment with aspirin, acenocoumarol, and an antianginal drug was started. The patient was discharged after showing improvement on medical management (Figures 5 and 6).
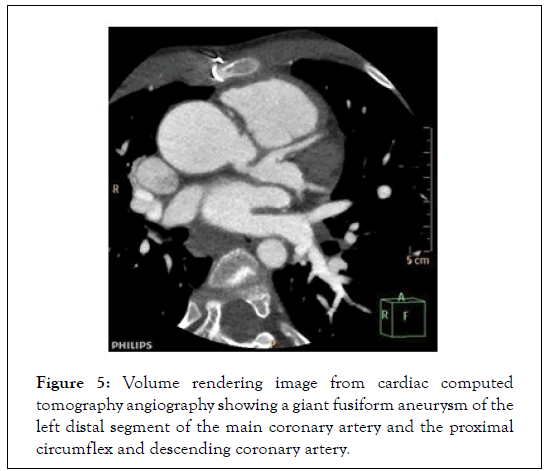
Figure 5: Volume rendering image from cardiac computed tomography angiography showing a giant fusiform aneurysm of the left distal segment of the main coronary artery and the proximal circumflex and descending coronary artery.
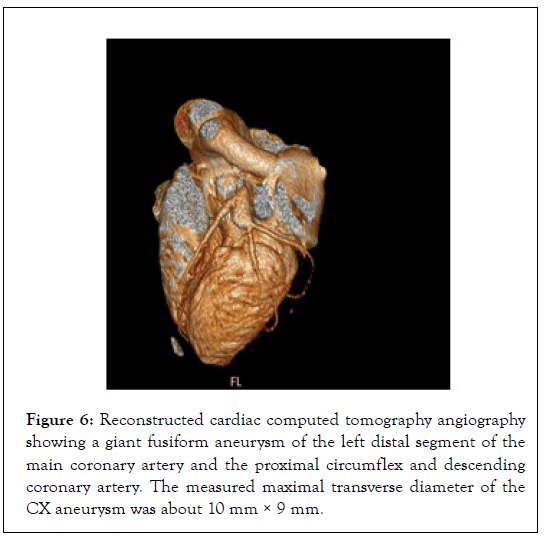
Figure 6: Reconstructed cardiac computed tomography angiography showing a giant fusiform aneurysm of the left distal segment of the main coronary artery and the proximal circumflex and descending coronary artery. The measured maximal transverse diameter of the CX aneurysm was about 10 mm × 9 mm.
Aetiology
Since Dr. Kawasaki’s initial description of the illness in Japan in the 1960s, many different theories about the triggering factors of Kawasaki Disease (KD) have been proposed, however the etiology remains unknown. The most widely accepted theories have been built on infectious diseases, environmental toxin exposure, and autoimmunologic response. The primarily winter-spring KD seasonality, characterization of the disease by a febrile exanthem with lymphadenitis and mucositis features like contagious diseases, such as adenovirus infection, measles, and scarlet fever and well-documented Japanese epidemics with wave-like spread support an infectious trigger. Also, immunologic response consists of CD8 T cells, oligoclonal IgA, cytotoxic T cells and interferon pathways in the coronaries in fatal form of KD support a viral etiology. On the other side even a wide variety of different bacterial and viral infections such as parvovirus B19, Propionibacterium, human bocavirus, and numerous others were identified, none has been consistently associated with the illness. Besides, the possibility of a unique KD infection with negative serologic, genetic, and immunologic study or case series create the major debate about explaining KD aetiology by the cause of a single agent. Environmental factors also have been proposed as the triggers of KD. Manifestations of mercury toxicity has some common features between the cutaneous and acral manifestations of KD to those of acrodynia, so mercury exposure proposed as a causative role in KD but there were no aetiological relation between all KD cases and history of mercury exposure. Similarly, the frequent association between KD and atopy, particularly atopic dermatitis, has inspired a search for an autoimmune response as playing a trigger role for KD, but we depart from the triggering role of it cause of non-recurring nature of KD and the lack of indication for corticosteroids in primary therapy of KD.
Genetic background of coronary artery lesion
Kawasaki disease is a disease of genetic susceptibility. There is a correlation between coronary artery lesions and genetic polymorphism. Based on several Genome-Wide Association Studies (GWAS) and other gene polymorphism studies, the data suggest that Coronary Artery Lesion formation in Kawasaki Disease is related to various genetic factors, such as HLA-E, HLA-B, CD40, FCGR2A, HMGB1, MICB, PELI1, ITPKC, CASP3, MMP (MMP- 3, MMP-13), IL-10, and ITPR3.
Onouchi, et al. [1] identify a functional SNP (rs28493229) in the ITPKC gene on chromosome 19q13.2 that may be significantly correlated with the progression of Coronary Artery Lesion through the Ca2 ± NFAT signalling pathway as a negative regulator of T-cell activation but only in Japanese and Caucasian populations. CD40 can activate both humoral and cellular immunity by stimulating antigen-presenting cells and vascular endothelial cells. Kuo, et al. [2-5] indicated that the genetic polymorphisms of CD40 (rs4810485) are involved in Coronary Artery Lesion of Kawasaki Disease in a Taiwanese population. A Korean GWAS study showed that the functional SNP (rs17136627) of a KCNN2 gene that plays a role in potassium mediators/small conductance calcium activation channels in Kawasaki Disease patients without Coronary Artery Lesion and in patients with medium or giant aneurysms is closely related to the development of severe Coronary Artery Lesion. Kuo, et al. [2-5] found that gene combinations (LOC100133214 (rs2517892) and IL2RA (rs3118470)) influence Coronary Artery Lesion in 384 SNPs. The TGF-βsignalling pathway may play an important role in EMT and pro-inflammatory cell infiltration in Coronary Artery Lesion formation. Shimizu, et al. [6-8] using a candidate gene approach, found variants in genes in the transforming growth factor (TGF)-β signalling pathway (TGFβ2, TGFβR2, and SMAD3) are associated with the Z scores of Coronary Artery Lesions in patients of Euro-Americans and Koreans.
Pathophysiology
Kawasaki disease is a systemic vascular disease of medium-sized arteries preferentially occurring in infants and children (usually age <5 years). It occurs most commonly in patients of Asian ethnicity. The diagnosis of Kawasaki disease is based on a fever for >5 days plus 4 of the following findings: bilateral non-exudative conjunctival injection (erythema), cervical lymphadenopathy, changes in the peripheral extremities (edema, erythema, desquamation) polymorphous truncal exanthem, and changes in the lips, tongue, or oral mucosa (injection, drying, fissuring, red strawberry tongue). A serious complication of Kawasaki disease is coronary artery inflammation leading to the development of coronary artery aneurysms, acute myocarditis, cardiac tamponade, and sudden cardiac death. The exact etiology of this disease is currently unknown but recent studies have shown the role of genetic susceptibility of Kawasaki disease in children of Japanese ethnicity regardless of their country of residence along with an elevated expression and activity Matrix Metalloproteinases (MMPs), and suggest that imbalances in MMPs or MMP/tissue inhibitor of MMP (TIMP) play important pathophysiological roles in the development of coronary artery lesions in this disease.
Immune mechanisms of coronary artery lesion
Kawasaki disease is an inflammation of blood vessels throughout the body and abnormal activation of the immune system is an important link in the development of coronary artery lesions. The innate immune system (cellular and humoral) is involved in the disease in an early stage characterised by the production of neutrophils, majority γδT cells, pathogen-associated molecular patterns (PAMPs), the elevated levels of damage-associated molecular patterns (DAMPs), and circulating inflammatory cytokines, such as Interleukin (IL) 1, IL-6, and Tumour Necrosis Factor-α (TNF-α) in the acute stage. Meanwhile, the intestinal mucosal permeability and sIgA are closely related to vasculitis in a Kawasaki Disease animal model. A CAWS-induced model indicates that NLRP3 in BMDCs are important for vasculitis formation. The markers associated with antigen presentation (CD74, CD1c, CD20 and TLR7) and activated myeloid dendritic cells are significantly elevated in coronary tissue. The activation of the adaptive immune system appears in the later stage of the disease, mainly as the increase of regulatory T-cells, and memory T and memory B-cells. The self-limited nature of the disease coupled with a low rate of recurrence and the presence of oligo-clonal IgA implies that Kawasaki disease is associated with a super- antigen rather than with a conventional antigen. In the animal model of Kawasaki disease, vasculitis induced by LCWE, CD8+ T-cells, rather than CD4+ T-cells, NK T-cells, or T Reg cells, is an important factor in the production of CAL. Interestingly, in patients with Coronary Artery Lesion, CD40L was highly expressed in CD4+ T-cells and platelets although there was no significant difference between CD8+ T-cells and serum. As a distinct subset of CD4+ T-cells, Tfh 1 (follicular T helper) cells are significantly lower. In contrast, cTfh2 cells are significantly increased. The immunological responses vary with different pathological conditions. It is understandable that the different studies produced different results, which are probably due to the different animal models used and the different disease stages applied in the studies.
Clinical presentation
The cardiac manifestations of Kawasaki Disease (KD) can be categorised as either coronary or non-coronary sequelae. Coronary artery manifestations mainly revolve around the degree of involvement of coronary arteries in the inflammatory process during the acute and sub-acute phase of the disease. Whereas non-coronary manifestations are related to inflammation of the endocardium, myocardium and pericardial tissue. Inflammation of the endocardium ultimately results in this inflammatory process subsequently leads to variable manifestations of coronary artery ectasia and aneurysmal formation. After KD illness, patients can develop persistent aneurysmal formation, transient mild dilatation or no dilatation at all [9]. Mild dilatation typically resolves, while aneurysmal formation can persist and thus result in clinical signs and symptoms of ischemic heart disease [9]. The mechanism of clinical symptoms occurs via thrombus formation within the aneurysmal segment, a layered thrombus that results in fibrotic stenosis or myofibroblast proliferation that also results in coronary artery stenosis [9]. It is important to highlight that it remains unclear whether or not KD in the absence of coronary artery ectasia results in accelerated coronary artery atherosclerosis later in life. While some small studies have investigated surrogate markers of atherosclerosis such as carotid intima-media thickness, large contemporaneous studies with long term follow-up are lacking [10]. Furthermore, much of the current understanding of the pathophysiology of KD is adopted from autopsy studies and thus skew the data towards severe disease [9]. Historically, the imaging modality of choice for the evaluation of coronary artery involvement during the acute phase of the illness is echocardiography [9]. The Japanese Health Ministry arbitrarily defined the degree of coronary ectasia by quantifying the aneurysmal segments as either small, medium or giant on the basis of the absolute measurement of the ectatic segment being <4 mm, 4 to 8 mm or >8 mm respectively [11]. This classification was demonstrated to be useful in predicting late outcomes of KD cardiac manifestation. For example, in a retrospective review of 1073 patients who met the diagnostic criteria for KD, 82% of patients had no coronary artery ectasia, whereas 12%, 4% and 2% had small, medium and giant coronary aneurysms respectively. Amongst the patient’s without coronary artery aneurysmal formation during the acute phase, none experienced ischemic symptoms later in life or developed occurrence of coronary artery ectasia during a follow-up of 6994 patientyears. Whereas some patients with small to medium aneurysms developed chest pain but without any deaths. However, patients with giant aneurysms developed myocardial infarction or death at an incidence of 26%. Owing to the fact that KD mainly occurs in growing children with a very wide spectrum of normal coronary artery size, the Japanese health ministry schema had limitations in its ability to standardise the severity of aneurysmal disease across age groups, different ethnicities and most importantly body size. Hence, authors proposed a more contemporary schema based on the Z score [12].The non-coronary cardiac manifestations of acute phase KD include myocarditis, pericarditis, myopericarditis and endocarditis. The American Heart Association includes these manifestations as part of the diagnostic clinical criteria for the diagnosis of KD [13]. These clinical syndromes occur due to the inflammatory milieu that ensues during the acute inflammatory phase. The clinical spectrum of presentations can vary from mild symptoms to cardiogenic shock. Cardiogenic shock can occur through various mechanisms, which include biventricular failure secondary to myocarditis, arrhythmias cardiac tamponade, severe valvulitis with valve insufficiency and constrictive pericarditis [14- 17]. Myocarditis is thought to be very prevalent in the acute phase of KD, with some studies demonstrating up to 70% of patients had findings consistent with myocarditis by non-invasive imaging [13]. The progression of myocarditis to fibrosis is difficult to study, as coronary complications can also lead to fibrosis via ischemic mechanism rather than an inflammatory mechanism. While histological studies have been able to demonstrate fibrosis well after the acute phase of KD, it remains unclear if these are sequelae of myocardial inflammation during the acute phase or secondary to ischemia and microvascular dysfunction secondary to coronary aneurysm formation and thrombosis [18,19]. Recent advances in myocardial imaging with cardiac magnetic resonance imaging have allowed better evaluation for fibrosis non-invasively. To that end, one small study was unable to demonstrate an association between late gadolinium enhancement in the absence of coronary aneurysm formation [20].
Diagnosis
Complete KD is a clinical diagnosis; no laboratory or imaging evaluations are required aside from echocardiography once the diagnosis is made. If KD is suspected but the diagnosis cannot be confirmed, the patient should be referred in a timely manner to a center that has experience with this illness. It is important to diagnose KD promptly, because a delay can result in Coronary Artery Aneurysms (CAAs) and other serious cardiac complications. Patients who are not treated with intravenous immune globulin (IVIG) by day 10 illness are at increased risk of cardiac sequelae and sudden death.
Diagnosis of KD according to the criteria established by Tomisaku Kawasaki in 1967 [9], requires the presence of fever lasting ≥ 5 days, combined with at least four of the five following physical findings, without an alternative explanation [2]
• Bilateral bulbar conjunctival injection
• Oral mucous membrane changes, including injected or fissured lips, injected pharynx, or strawberry tongue
• Peripheral extremity changes, including erythema of palms or soles, oedema of hands or feet (acute phase) or periungual desquamation (convalescent phase)
• Polymorphous rash
• Cervical lymphadenopathy (at least one lymph node>1.5 cm in diameter)
A concomitant infection affects about 40% of children with KD. Clinical judgment is required to attribute the fever to such an illness or to KD.
Rash and conjunctival injection are common symptoms of many illnesses, but other KD characteristics, such as red, cracked lips and redness and swelling of the hands and feet, are uncommon in the disorders in the differential diagnosis and should raise the suspicion for KD.
Incomplete KD-As with all clinical criteria, these are imperfect guidelines with less than 100% sensitivity and specificity. In addition, Dr. Kawasaki published his guidelines before cardiac involvement was recognised in this disease, so they were never intended to identify children at risk for developing CAAs. Thus, it is not unexpected that at least 10% of children who develop CAAs never meet criteria for KD [11]. Incomplete KD should be suspected in patients less than six months of age with unexplained fever ≥ 7 days, even if they have no clinical findings of KD, and in patients of any age with unexplained fever ≥ 5 days and only two or three clinical criteria. No laboratory values are included in the classical diagnostic criteria, but elevated WBC and platelet counts, transaminases, and acute-phase reactants, as well as anemia and pyuria, are suggestive of KD.
Echocardiography should be performed on all suspected KD patients as soon as possible to establish a baseline for longitudinal follow-up and therapy effectiveness. Furthermore, initial coronary artery diameter is used to identify individuals who are at high risk of developing a coronary aneurysm and therefore require enhancement of initial IVIG therapy. Finally, the measurements are useful for identifying patients who should be treated with IVIG despite failing to meet classical diagnostic criteria for KD. Coronary artery imaging in children is particularly challenging due to small vessel size, high heart rates and their inability to cooperate. The detection of CAA (Coronary artery aneurysm) by two-dimensional echocardiography in the acute phase is the initial imaging modality since it is noninvasive, repeatable at the bedside and due to the absence of radiation. However, the echocardiogram has certain limitations, including inadequate visualization of the coronary arteries (distal segments, circumflex coronary artery, luminal stenosis or presence of thrombosis) and may result in underestimation of the CAA burden and may increase the risk for secondary complications. Moreover, patients with persisting CAA after the acute phase need prolonged follow-up and additional noninvasive imaging modalities are required, such as Cardiac Magnetic Resonance imaging (CMR), coronary Computed Tomography (CT), exercise echocardiography or nuclear imaging techniques. Although invasive coronary angiography remains the imaging gold standard [1].Over the last few years, with the advent of higher detectors (256,320) and dual-source CT scanners is increasingly available, having improved the temporal resolution allowing a better accuracy of coronary artery evaluation by identifying stenotic lesions, presence of aneurysms, coronary artery ectasias, calcification or thrombosis with acceptable radiation exposure. CT calcium score is a low-dose radiation technique without intravenous contrast that measures calcification in the coronary arteries, which has been shown to be a strong predictor of coronary events. It can be used to detect coronary calcifications that may have been missed by echocardiography. However, there is a risk of radiation exposure and need for heart rate control and sedation in children under 5 years [10].CMR does not expose patients to radiation and remains the most suitable and best imaging modality for the assessment of cardiac function and for the detection of ischemia and infarction. In contrast, MRI has a lower spatial and temporal resolution for the detection of small aneurysms and requires heart rate control and has long imaging and sedation times in young children. In addition, in selected patients, coronary angiography could be considered when a catheter-based intervention is contemplated. The frequency of additional imaging will be guided by the symptoms [13].
Biomarkers for diagnosis of coronary artery lesion
Clinicians proposed different scoring systems to evaluate coronary artery lesions in patients with Kawasaki disease according to their characteristics, blood test results, and clinical course. Asai and Kusakawa's scoring system was widely used in the 1970s and 1980s, followed by Harada's in the 1990s. However, the sensitivity and specificity of this score vary from region to region. Currently, the evaluation of coronary artery lesions in Kawasaki disease mainly relies on color Doppler Echocardiography but ultrasound cannot accurately reflect the specific situation of coronary artery damage. It is reported that patients with normal ultrasound can still have coronary artery endothelial dysfunction, intima, and media change. Biomarkers are necessary to assist in the determination of coronary artery lesions. There are some potential biomarkers of Coronary Artery Lesion formation. Plasma clusterin level, NTproBNP, CRP, and IL-6 are highly suggestive of coronary artery lesions. Increased expression of Nitric Oxide Synthase (iNOS) in neutrophils suggests the occurrence of coronary artery lesions in KD patients. The study reported higher serum sLR11 level may be the biomarker of Coronary Artery Lesion at the convalescent phase. Li, et al. [21,22] found that 11-DH-TXB2, sP-selectin, IPF, and sCD40L levels are related to the degree of Coronary Artery Lesions. MicroRNA (miRNA) is considered to be one of the most promising biomarker resources in various types of nucleic acid research, including Kawasaki Disease. Li, et al. [21,22] showed that high levels of mir-92a-3p and miR-182-5p are a high risk factor for the occurrence of coronary artery lesion.
Treatment
The primary aim of treatment in the acute phase of Kawasaki Disease (KD) is minimising the incidence of coronary artery lesions as, if left untreated, KD can result in coronary artery aneurysms (CAA) in ~25% of cases. Treatment has shown to be most effective if administered as early as possible after onset of fever (preferably within 10 days).The main treatment strategy in the acute phase consists of a single 2g/kg dose of Intravenous Immunoglobulins (IVIG) in conjunction with four times daily medium- (30-50 mg/kg/day) to high (80-100 mg/kg/day) dose aspirin (ASA) until the patient is afebrile (usually 48-72 hours) followed by low-dose (3-5 mg/kg/day) ASA for a duration of 14 days. Large randomised trials have shown that the combined strategy of IVIG and ASA reduces risk of CAA to ~5%.Interestingly, a significant group of patients is IVIG resistant and suffers recurrent of persistent fevers requiring a second dose of IVIG or steroids (e.g. 30 mg/kg intravenous methylprednisolone for 2-3 hours once daily for 2-3 days or dexamethasone 0.3mg/kg/day for 3 days).Other upcoming and promising management strategies for KD include TNF-α inhibitors (e.g. Infliximab, Abciximab or Etanercept), plasma exchange, cyclosporine, cyclophosphamide and methotrexate [23-27]. There is currently no drug available to reverse the already occurred damage. Patients with small CAA are typically continued on low-dose ASA mono therapy after acute phase treatment while patients with moderate-sized aneurysms can be managed with ASA and a P2Y12 inhibitor and patients with large aneurysms may be treated with an antiplatelet agent in conjunction with anticoagulant therapy. For patients presenting with an angina or acute coronary syndrome as result of a CAA culprit, both percutaneous and surgical revascularisation are treatment options. The appropriate revascularisation strategy differs according to the shape and extent of the aneurysm [28-30]. Treatment options include covered stents, Amplatzer occluder, (balloon or stent-assisted) coil embolization or surgical exclusion followed by coronary artery bypass surgery. Nevertheless, the level of evidence for treatment of developed CAA is low due to lack of randomised trials and large-scale data. The treatment strategy for CAAs after KD should therefore be tailored to the individual patient [30-36].
Long-term coronary outcomes
Most of the patients with small or medium-sized coronary artery aneurysms usually return to normal luminal dimension within 2-3 years, though few patients might developed stenosis and MI. Those without Coronary lesion doesn’t show any abnormality in the Echocardiographic follow-up. Chronic inflammation can be found in coronary artery pathological lesions and long-term isotope nuclear imaging may show high metabolism in the coronary site. On longterm follow up by Non-invasive assessment of arterial structure and function, patients with or without Coronary Artery Lesion. May present a high risk of cardiovascular disease, including increased aortic IMT and carotid distensibility [37-48]. Others may present with segmental thickening of the intima in the degraded coronary aneurysm that can be present in even those with no coronary lesions in the acute phase [49-52]. Some studies have reported new aneurysm onset or further expansion in the late period. Prognosis of Coronary Artery Lesion mainly depends on the degree of stenosis of the lumen [53-61]. In Kawasaki Disease patients, intimal thickening with calcification in coronary aneurysm segment are similar to adult coronary atherosclerosis change [62-68]. Coronary artery lesions are a chronic process, and it is necessary to have a careful follow-up study to observe patients because some vascular dysfunction can occur later even when coronary aneurysm disappears [69-74].
Coronary Artery Lesion is a common complication of Kawasaki Disease. The incidence ranges between 30% and 50% in the 9 to 10 days of illness. The risk of development of coronary lesions has been attributed to many factors including male, delay in the initiation of intravenous immunoglobulin, high level of circulating inflammatory biomarkers (C-reactive protein >200 mg/l) and <1 year of age or more than 8 years of age and recurrent Kawasaki Disease. IVIG and high- dose aspirin are the mainstays of treatment. Intravenous immunoglobulin 2 g/kg is given as a single infusion over 12 h and may be repeated once in recalcitrant cases. Moderate (30 to 50 mg/kg/day) to high (80 to 100 mg/kg/day) dose of aspirin should be continued until the patient is apyrexial. Kawasaki Disease is the only disease for which it is allowed to use aspirin as a treatment line in the children age group; however, it should be combined with the influenza vaccine to guard against Rye syndrome. Early initiation of intravenous immunoglobulin is found to be protective against the development of Coronary Artery Aneurysm. Some patients were found to have treatment resistance, and one study suggested a scoring system to predict response to treatment based on the level of circulating inflammatory biomarkers, duration of illness, and age of presentation. The use of corticosteroids did not show marked beneficial effects in comparison with placebo in the context of cardiovascular complications. In most cases, the Coronary Artery Lesion usually starts regression after 10 days of therapy, however, about 20% cases progress and subsequent develop complications including aneurysm thrombosis, myocardial infarction, and deterioration of the left ventricular systolic function. Cardiovascular complications are the first cause of death among Kawasaki patients. These devastating sequelae can be prevented by establishing a proper diagnosis based on given clinical criteria and early initiation of the optimal dose of intravenous immunoglobulin. The Kawasaki Disease patient cohort is currently growing and represents a challenge in terms of increased cardiovascular disease risk stratification. The worst prognosis is among patients with giant aneurysms (>8 mm); however, the risk of subsequent myocardial infarction in patients with small aneurysms is uncertain. The state of vascular inflammation and endothelial injury impacts coronary flow reserve and makes those patients more vulnerable to accelerated atherosclerosis. Ongoing registry studies and prospective data are aiming to provide optimal management of Kawasaki patients with Coronary Artery Aneurysm with regard to the thrombotic regimen (anti platelets vs. anticoagulation or combined regimen). These conundrums in clinical management are of paramount importance and warrant future prospective studies for a better understanding of disease progression.
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
[Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [Pubmed].
[CrossRef] [ Google Scholar] [ Pubmed].
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] (all versions) [Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [ Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [ Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[Cross Ref][Google Scholar][All Versions][Pubmed]
[Cross Ref][Google Scholar][All Versions][Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
Citation: Camm NJ, Tenekecioglu E, Kamel A, Somoza-Cano FJ, Maksud D, GarcÃ?Âa JR (2022) Coronary Artery Lesions in a Young Patient with Kawasaki Disease from Pacific Region. J Clin Exp Cardiolog. 13:712.
Received: 14-Mar-2022, Manuscript No. JCEC-22-15381; Editor assigned: 17-Mar-2022, Pre QC No. JCEC-22-15381 (PQ); Reviewed: 31-Mar-2022, QC No. JCEC-22-15381; Revised: 05-Apr-2022, Manuscript No. JCEC-22-15381 (R); Published: 12-Apr-2022 , DOI: 10.35248/2155-9880.22.13.720
Copyright: © 2022 Camm NJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.