Journal of Osteoporosis and Physical Activity
Open Access
ISSN: 2329-9509
ISSN: 2329-9509
Research Article - (2021)Volume 9, Issue 4
Purpose: Osteoporosis consists an increasing economic burden for healthcare systems worldwide. In addition to prevention strategies, pharmaceutical treatment to reduce the risk for osteoporotic fractures is gaining focus. Data about the cost effectiveness of anti- osteoportic treatments in Greece is missing. We performed a cost- effectiveness analysis of the two golden standard treatment strategies, bisphosphonates and monoclonal antibodies, such as denosumab.
Methods: Clinical data and data of bone absorptiometry of 128 post-menopausal women, who received antiosteoporotic treatment, were retrospectively collected. Based on this data a cost- effectiveness analysis was performed. As an indicator of effectiveness, we defined the patients’ transition, under anti- osteoporotic medication, into a condition in which all the criteria underlined by the Hellenic Osteoporosis Foundation as necessary to stop antiosteoporotic treatment are met. The costs included in the analysis involve the pharmaceutical costs, cost of the diagnostic procedure and cost of treatment of incident osteoporotic fractures. The two treatment regimens were compared by the incremental cost- effectiveness ratio (ICER).
Results and conclusions: Treatment with denosumab is found to have statistical significantly higher efficiency (ΟR 2.58; 95%CIs 1.21-5.50; p=0.016) but also significantly higher treatment costs (2412.00 € ± 123.50 and 1760.00 € ± 141.3; p=0.0007) compared to treatment with bisphosphonates. Treatment with denosumab, is not cost-effective compared to bisphosphonate treatment (ICER 3105 €) for accomplishing the treatment objectives. In order to achieve cost effectiveness, the cost per unit of denosumab should be discounted by 30% or the adherence to treatment should significantly be increased.
Osteoporosis; Cost-effectiveness analysis; Bisphosphonates; Denosumab
Osteoporosis is a chronic disease that is characterized by loss of bone mass. It progresses most often subclinically, until its characteristic clinical manifestation, which is pain due to an osteoporotic fracture. The incidence of osteoporotic fractures is significantly increased due to the aging of the world's population. Osteoporotic fractures, mainly hip fractures, are the main factor associated with the increasing economic burden of osteoporosis. Based on the latest existing data from 2010, the direct cost of treating osteoporotic fractures in Greece amounted to 680 million euros, while the indirect cost, including the loss of well-being, amounted to 1.9 billion euros [1]. The corresponding cost in EUcountries was 37 billion euros and is estimated to reach 76.7 billion euros in 2050 [2]. In Europe, the cost of treating cardiovascular disease for the year 2015 amounted to 210 billion euros, while the cost for the treatment of malignancies for the year 2009 amounted to 126 billion [3,4]. Therefore, prevention of fractures due to osteoporosis through appropriate anti-osteoporotic therapy should be considered of major importance.
Osteoporosis prevention is based on trying to maximize bone mass in childhood and adolescence through dietary measures and exercise. The prevention of osteoporotic fractures is based on measures to prevent falls and other accidents and on medication aiming at reducing the risk of fractures. Monoclonal antibodies, such as denosumab act by inhibition of the receptor activator of nuclear factor kappa-B ligand (RANK-L), which leads to inhibition of osteoclast differentiation and promotion of osteoclast apoptosis [5]. Oral bisphosphonates, such as alendronate, risedronate and ibandronate act by inhibiting the activation and bone resorptive action of osteoclasts [6]. These are the two most commonly used strategies for modulation of osteoporosis in Greece [7].
A retrospective study of in 113 postmenopausal women showed that both treatments significantly increased bone density over a 12-month follow-up period. With denosumab being superior in increasing BMD of the femoral neck area [8]. In a randomized clinical trial both interventions led to an increase in BMD as well as a decrease in specific parameters related to bone resorption, with the reduction of bone resorption being greater in the denosumab group [9].
The limited financial resources mandate economic evaluation of potential interventions for osteoporosis [10,11]. This is even more important in countries struck by the financial crisis such as Greece.
The lack of adequate clinical data about the efficacy and the cost of anti- osteoporotic medication in the Greek population renders such analyses extremely difficult. Therefore, most analyses are based on theoretical models, using data from other European countries [12,13]. The aim of this study was to collect data from postmenopausal women from Greece with diagnosed osteoporosis and their retrospective evaluation in order to compare the cost- effectiveness of denosumab and oral bisphosphonates.
Due to the paucity of burden of illness studies of osteoporosis in the Asian region, particularly the Philippines, it is difficult to allocate healthcare resources appropriately for fracture prevention. The availability of information on the financial burden of osteoporosisrelated fractures, particularly in the local region, will create awareness on the size of the problem as well as assist healthcare authorities to initiate appropriate programs and strategies.
Patient selection and data acquisition
Patient data were collected from June to December 2019 from the Department of Nuclear Medicine, 417 Army Share Fund Hospital (NIMTS), and Athens, Greece and from a primary healthcare facility (private orthopedic practice, Anavyssos, Greece). The protocol is approved by the Ethic Committee of the 417 Army Share Fund Hospital (NIMTS), Athens, Greece (protocol number 1/2/29.1.2020).
Patients who met all the criteria for admission to the study and none of the exclusion criteria were enrolled only after written consent. Inclusion criteria were a) female gender; b) age >53 years; c) established menopause (1 year without menstruation) and d) anti-osteoporotic therapy with bisphosphonates (group A) or denosumab (group B). Exclusion criteria were a) history of malignancy and b) treatment with high-dose corticosteroids (>7.5 mg/day)
From every patient enrolled in the study. following data was collected: a) Demographics, such as gender, age, height (cm), weight (kg); b) Clinical data such as smoking, history of fracture, history of parental hip fracture, history of rheumatoid arthritis, treatment with cortisone; c) Data on the treatment of osteoporosis such as type, dosage and duration of anti-osteoporotic therapy, type, dosage and duration of calcium and vitamin D replacement therapy. Also the adherence to the anti-osteoporotic therapy was documented. Non- adherence was defined as a gap in treatment of more than 60 days for oral bisphosphonates and one year or more for denosumab treatment.
Data of an examination of Bone Mineral Density (BMD) by DUAL X-RAY ABSORPTIOMETRY (DXA) from the same site (hip or spine) were collected for each patient before the begin of antiosteoporotic treatment and then yearly for five consequtive years were collected. The time frame between the first and the last DXA was selected, which is the median time period required for both bisphosphonates and denosumab to be effective [14].
Assessment of effectiveness
The collected data was used to perform a cost- effectiveness analysis comparing treatment with denosumab to treatment with oral bisphosphonates.
The assessment of the effectiveness of each treatment was based on the Fracture risk assessment tool for the Greek population (FRAX® http://www.shef.ac.uk/FRAX/) and the criteria, set by the Greek Osteoporosis Foundation and related studies.7,15 which are mandatory in order to consider stopping anti- osteoporotic treatment. These are:
a) Absence of an incident fracture of the hip or spine or >1 incident fractures of other parts of the skeleton and
b) T score of the femoral neck or of the spine in the lumbar (L) vertebrae 2- 4>-2.5 and
c) 10-year risk (FRAX) of major osteoporotic fracture <10% and of hip fracture <2.5% for people aged 50 to 75 years or
d) 10-year risk (FRAX) of major osteoporotic fracture <15% and of hip fracture <5% for people over 75 years of age
When a patient met all the above-mentioned criteria after at 5 years, then the treatment was considered to be effective.
Assessment of cost
The assessment of cost of treatment per patient was performed from the point of view of the NHS and included following costs:
A) The cost of the pharmaceutical (K) per patient results from the sum of the cost of the pharmaceutical preparations for each year among the selected DXA. The calculation is based on the following equation16
K = 0.75 * (Nf * pricef + Nf-1 * pricef-1 + Nf-2 * pricef-2 + ……… + Nb * priceb)
Nf: Number of drug units used during the year of the last DXA (year f); pricef: Retail price of the pharmaceutical product for the year f; Nb: Number of drug units used during the year of the first last selected DXA (year b); Priceb: Retail price of the medicinal product for the year b.
The rate of 0.75 refers to the percentage of coverage of the medication by the NHS in Greece.
The price of the pharmaceutical product for each year was calculated on the basis of an annual discount rate of 2% starting from the year 2019 [17]. The retail price of the pharmaceutical product for the year 2019 came from the last bulletin of prices of medicines for human use of the Ministry of Health of Greece (protocol number Δ3(α)/87611.13/12/2019) (Table S1).
B) The cost of the diagnostic procedure, which includes the cost of the DXA and salary of the staff. The cost of the DXA was calculated based on the electronic prescription (www.e-perscription.gr) at € 52.82. Since for the monitoring of osteoporosis it is recommended to perform a DXA per year, the diagnostic cost per patient was calculated by multiplying the price of € 52.82 with the years of treatment. In addition, the cost of the medical visit was added to monitor the course of each patient (€ 10) during the years of treatment. The operating costs of each unit were not taken into account, as this differs significantly between health care units and could lead to incorrect cost estimation.
C) Cost of treating new osteoporotic fractures. In the case of patients with an incident fracture during the study period, the corresponding cost of fracture treatment treating was added, as determined based on the published diagnosis related groups (DRGs) of the Ministry of Health (27/03/2012) (Table S2).
Cost- effectiveness analysis
The treatments were compared based on the incremental costeffectiveness ratio (ICER), which was calculated based on the equation:
Where, C is the total average cost and E is the effectiveness of each treatment.
Statistical analysis
Categorical data were presented as frequencies and quantitative characteristics were expressed as mean values ± Standard Deviation (SD). Univariate analysis between treatment groups was performed with the Fisher's exact test for qualitative variables and the Mann- Whitney U test for quantitative variables. Odds Ratios (OR) and 95% Confidence Intervals (CIs) for were calculated by the Mantel and Haenszel’s statistics. Demographic variables associated with the effectiveness of treatment were transformed into dichotomous variables after ROC curve analysis. For each parameter the coordinate point with the maximum value of the Youden index was used as a cut- off. Step- wise Logistic regression analysis with Odds Ratios (ORs) and Confidence Intervals (CIs) was used to investigate if the type of treatment is an independent variable for treatment effectiveness. Any p value below 0.05 was considered statistically significant.
Clinical data
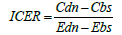
The patient selection process is shown in Figure 1. Between October 2019 and February 2020, data was collected from 300 postmenopausal women, aged 53 to 96 years, with osteopenia or osteoporosis. 150 patients received anti- osteoporotic therapy. 6 individuals were excluded due to a history of malignancy and 4 individuals due to high-dose corticosteroid therapy. 10 individuals were excluded as they did not initially meet the criteria for initiating anti-osteoporotic therapy according to the FRAX fracture risk assessment tool. Two individuals were excluded because they were treated with teriparatide, which was not included in the evaluated treatments. 128 people were eventually included in the analysis. Of these, 95 came from the 417 Army Share Fund Hospital (NIMTS) and 33 from the private orthopedic practice.
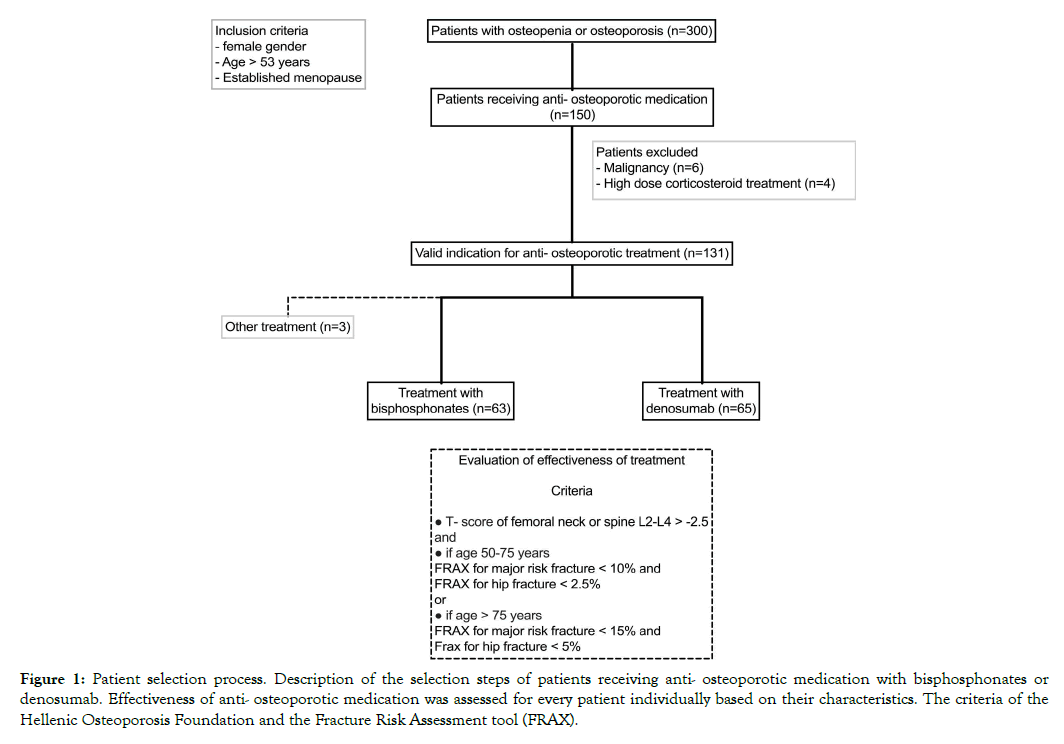
Figure xxxx: Patient selection process. Description of the selection steps of patients receiving anti- osteoporotic medication with bisphosphonates or denosumab. Effectiveness of anti- osteoporotic medication was assessed for every patient individually based on their characteristics. The criteria of the Hellenic Osteoporosis Foundation and the Fracture Risk Assessment tool (FRAX).
63 individuals (49.2%) were treated with bisphosphonates (group A) and 65 individuals (50.8%) were treated with denosumab (group B). The demographic characteristics of the populations of the two groups are shown in Table S3. The populations of the two groups differed significantly in weight and height, but not in body mass index. The number of patients with low dose cortisone treatment in their history was greater in the bisphosphonate group. No significant differences were found concerning age, smoking and pre-existing fractures. Finally, major comorbidities such as rheumatoid arthritis, high blood pressure, hypothyroidism, hyperthyroidism and diabetes occurred with similar frequency in both treatment groups.
Adherence to anti- osteoporotic treatment was 47.6% and 47.7% in the group of oral bisphosphonates and denosumab respectively. The number of patients receiving calcium and / or vitamin D replacement therapy did not differ between treatment groups. In the bisphosphonate treatment group, 63% of patients received alendronate, 8% received risedronate, 24% received ibandronate, and 5% received zoledronic acid.
Effectiveness of treatment regimens
Of the 128 patients, almost 1/3 (n=41) developed a fracture during the study period, most often distal radius fractures (11.7%). followed by fractures of the ankle (n=6.3%) and vertebral fractures (4.6%) (Table 1). Comparing the two treatment groups, no statistically significant difference was found in the incidence of different types of fractures during the treatment period.
Table 1: Incident fracture per type of anti- osteoporotic medication.
| Bisphosphonates (n=63) | Denosumab (n=65) | Total | |
|---|---|---|---|
| Hip fracture | 1 | 0 | 1 |
| Vertebral fracture | 3 | 3 | 6 |
| Distal radius fracture | 9 | 6 | 15 |
| Other fracture | 9 | 10 | 19 |
| 22 | 19 | 41 |
Treatment with denosumab led to a statistically significant increase in BMD in the hip (25.07%. p=0.001) and T-score in the spine (4.72%. p=0.001). In contrast, patients treated with bisphosphonates did not show statistically significant changes in DXA parameters in the hip or in the spine. Comparing changes in the DXA parameters, the change in T-score (p=0.017) and BMD (p=0.001) of the spine and the change in BMD in the hip (p 0.030) under treatment with denosumab were compared to respective changes under treatment with bisphosphonates (Figure 2A-D).
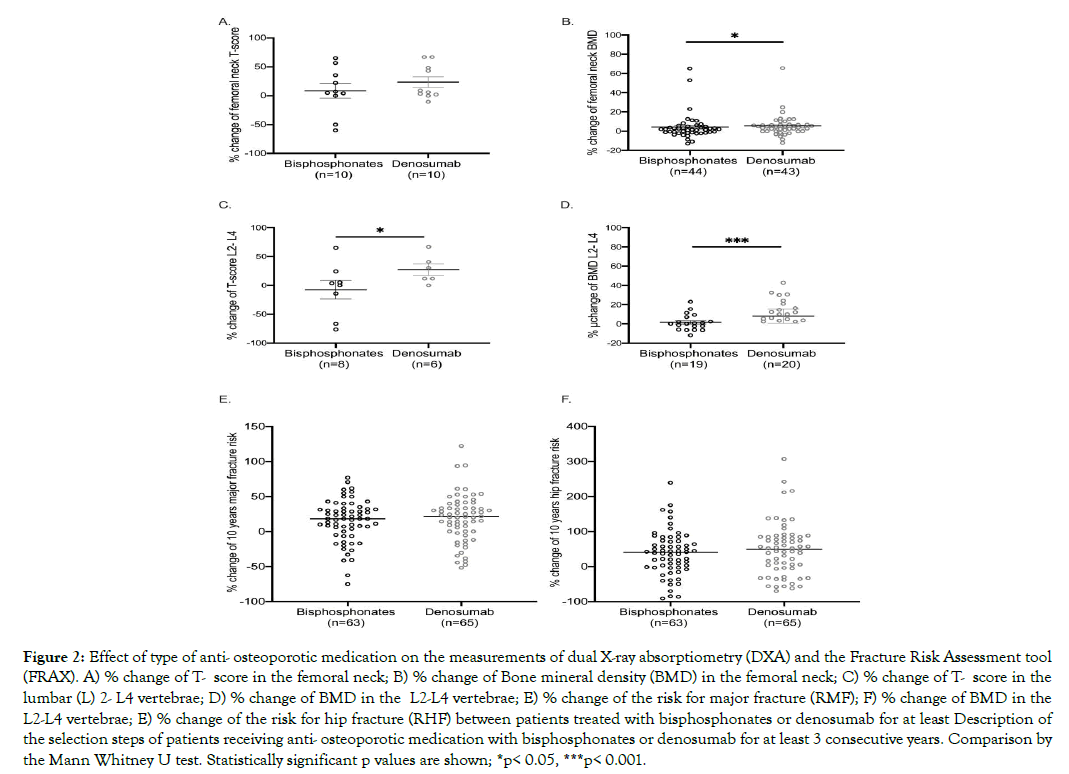
Figure 2: Effect of type of anti- osteoporotic medication on the measurements of dual X-ray absorptiometry (DXA) and the Fracture Risk Assessment tool (FRAX). A) % change of T- score in the femoral neck; B) % change of Bone mineral density (BMD) in the femoral neck; C) % change of T- score in the lumbar (L) 2- L4 vertebrae; D) % change of BMD in the L2-L4 vertebrae; E) % change of the risk for major fracture (RMF); F) % change of BMD in the L2-L4 vertebrae; E) % change of the risk for hip fracture (RHF) between patients treated with bisphosphonates or denosumab for at least Description of the selection steps of patients receiving anti- osteoporotic medication with bisphosphonates or denosumab for at least 3 consecutive years. Comparison by the Mann Whitney U test. Statistically significant p values are shown; *p< 0.05, ***p< 0.001.
As for the 10-year risk of major osteoporotic fracture and hip fracture, both bisphosphonate therapy and denosumab treatment did not prevent a statistically significant increase. Thus, in the bisphosphonate treatment group, the 10-year risk of major osteoporotic fracture increased by 15.8% (p=0.021) and of hip fracture by 9% (p=0.038). Respectively in the denosumab treatment group, the 10-year risk of major osteoporotic fracture increased by 12.7% (p=0.006) and of hip fracture by 28.6% (p=0.012). Comparing the two treatment groups, the difference in the change in both the 10-year risk of major osteoporotic fracture and the corresponding risk of hip fracture was not statistically significant (Figure 2E,F).
From the above it is clear that, by evaluating individual parameters related to osteoporosis, such as T-score, BMD or the risk of fracture itself, it is not possible to draw a safe conclusion about the effectiveness of each treatment, as while a treatment can to improve one parameter, at the same time it may be related to the deterioration of another parameter. This proves again the need for an efficient indicator, which will take into account all the above parameters. Using as an effectiveness indicator, the achievement of all treatment goals set by the Greek osteoporosis Foundation, bisphosphonate therapy was effective in 15 patients (23.8%), while denosumab was effective in 29 patients (44.6%). Therefore, denosumab treatment was 2.6 times more likely to be effective than bisphosphonate therapy (OR 2.58, 95% CIs 1.21-5.50. p=0.016) (Figure 3A).
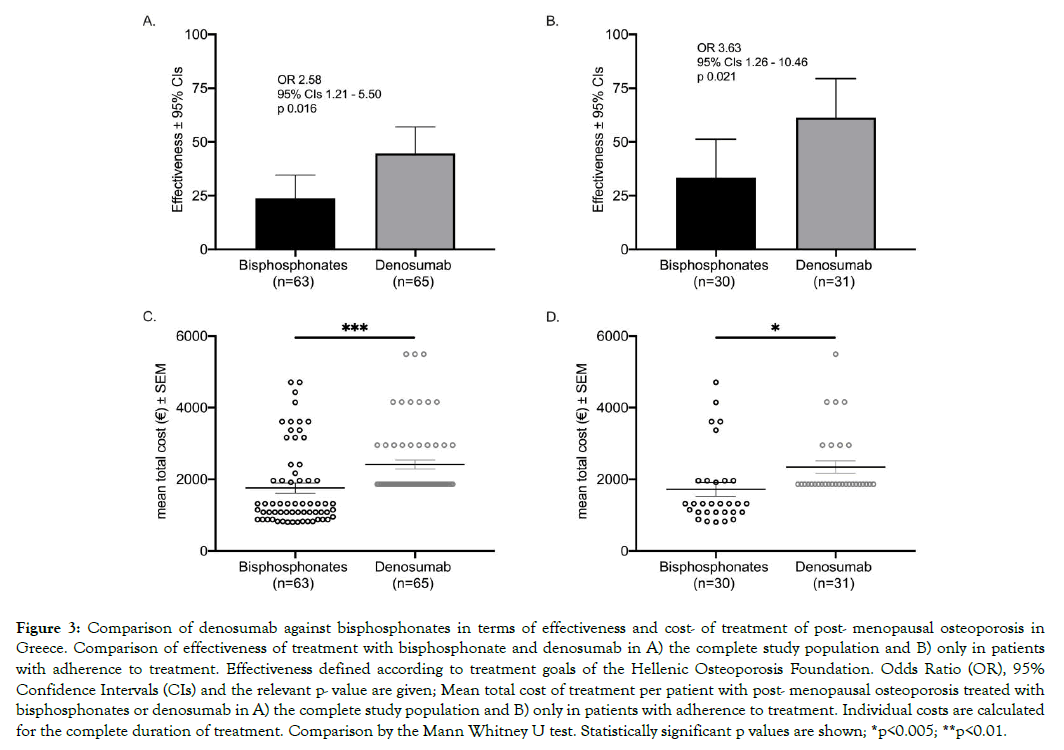
Figure 3: Comparison of denosumab against bisphosphonates in terms of effectiveness and cost- of treatment of post- menopausal osteoporosis in Greece. Comparison of effectiveness of treatment with bisphosphonate and denosumab in A) the complete study population and B) only in patients with adherence to treatment. Effectiveness defined according to treatment goals of the Hellenic Osteoporosis Foundation. Odds Ratio (OR), 95% Confidence Intervals (CIs) and the relevant p- value are given; Mean total cost of treatment per patient with post- menopausal osteoporosis treated with bisphosphonates or denosumab in A) the complete study population and B) only in patients with adherence to treatment. Individual costs are calculated for the complete duration of treatment. Comparison by the Mann Whitney U test. Statistically significant p values are shown; *p<0.005; **p<0.01.
ROC curve analysis revealed the following baseline values to be associated with the effectiveness of the treatment: age >75 years and BMI >25 and adherence to treatment. All above variables entered into stepwise forward logistic regression analysis (Table 2). Analysis showed that treatment with denosumab instead of bisphosphonates was an independent protective factor for effectiveness of anti- osteoporotic therapy. Age >75 years, BMI>25 and adherence to treatment also were shown to be independent protective factors for effectiveness.
Table 2: Baseline and clinical characteristics of patients with osteoporosis. Univariate and step- wise logistic regression analysis of parameters associated with the effectiveness of anti- osteoporotic medication.
| Effectiveness of treatment | ||||||
|---|---|---|---|---|---|---|
| No | Yes | Univariate analysis | Step-wise forward logistic regression | |||
| Demographics (n, %) | (n=84) | (n=44) | OR (95% Cis) | p | OR (95% Cis) | p |
| Age > 75 years # | 27 (32.1%) | 25 (56.8%) | 2.78 (1.31 – 5.89) | 0.008 | 2.79 (1.18 – 6.60) | 0.019 |
| Weight > 61 kg # | 45 (53.6%) | 32 (72.7%) | 2.31 (1.05 – 5.09) | 0.039 | ||
| Height > 163 cm # | 34 (40.5%) | 15 (34.1%) | 0.76 (0.36 – 1.63) | 0.567 | ||
| ΒΜΙ > 25 # | 40 (47.6%) | 33 (75%) | 3.30 (1.48 – 7.39) | 0.005 | 3.75 (1.52 – 9.28) | 0.004 |
| Smoking | 14 (16.7%) | 2 (4.5%) | 0.24 (0.05 – 1.10) | 0.040 | ||
| Previous fracture | 30 (35.7%) | 11 (25.0%) | 0.60 (0.27 – 1.36) | 0.238 | ||
| Parental hip fracture | 20 (23.8%) | 5 (11.4%) | 0.41 (0.14 – 1.18) | 0.105 | ||
| Intake of cortisone | 11 (13.1%) | 0 (0%) | 0.62 (0.54 – 0.72) | 0.016 | ||
| Comorbidities (n, %): | ||||||
|
1 (1.2%) | 0 (0%) | 0.66 (0.58 – 0.74) | 0.656 | ||
|
19 (26.0%) | 10 (27.8%) | 1.09 (0.45 – 2.68) | 0.509 | ||
|
18 (24.7%) | 9 (25.0%) | 1.02 (0.41 – 2.56) | 0.573 | ||
|
5 (6.8%) | 1 (2.8%) | 0.39 (0.04 – 3.46) | 0.661 | ||
|
4 (5.5%) | 3 (8.3%) | 1.57 (0.33 – 7.41) | 0.682 | ||
| Characteristics of anti- osteoporotic treatment (n, %) | ||||||
| Denosumab vs bisphosphonates | 36 (42.9%) | 29 (65.9%) | 2.58 (1.21 – 5.50) | 0.016 | 3.32 (1.38 – 7.99) | 0.007 |
| Adherence | 31 (36.9%) | 30 (68.2% | 3.66 (1.69 – 7.94) | 0.062 | 4.74 (1.52 – 9.28) | 0.001 |
| Calcium substitution | 75 (89.3%) | 41 (93.2%) | 1.64 (0.42 – 6.40) | 0.543 | ||
| Vitamin D substitution | 74 (88.1%) | 41 (93.2%) | 1.85 (0.48 – 7.09) | 0.540 | ||
A. Abbreviations ΒΜΙ: Body mass Index; OR: Odds ratio; CΙs: Confidence intervals; B. OR and p value of the parameter intake of cortisone is not shown in the multivariate analysis due to lack of patients with cortisone intake in the arm of effective treatment; C. # Cut- off point of each variable was determined based on the coordinate point with the maximum value of the Youden index; D. Univariate analysis by the Fisher’s exact test
Further analyzing the efficacy of bisphosphonates, it was shown that alendronate was effective in 10 patients (25%), risedronate in 1 patient (20%), ibandronate in 4 patients (26.7%), and zoledronic acid in 0 patients. At this point it should be emphasized that the zero efficacy of zoledronic acid is associated with the small number of patients who received this treatment and were included in the study.
In a sub- analysis of patients who met the criteria for adherence to anti-osteoporotic treatment, bisphosphonate therapy was effective in 10 patients (33.3%), while denosumab was effective in 20 patients (66.7%). Therefore, denosumab treatment was 3.6 times more likely to be effective than bisphosphonate therapy (OR 3.63, 95% CIs 1.26-10.46 p=0.021) (Figure 3B). Adherence to treatment seems to be more important for patients receiving denosumab, where adherence increased the probability of an efficient treatment more than 5 times (OR 5.05, 95% CIs 1.75-14.57 p=0.003).
Cost of osteoporosis treatment
The average pharmaceutical cost per patient for the 5 year follow up was significantly greater in the denosumab treatment group (€ 1551.61 € ± 0) compared to bisphosphonate therapy (€ 742.8 € ± 24.26) (p < 0.0001). The average total cost of treatment per patient, which includes both the diagnostic procedure and the treatment of complications such as osteoporotic fractures, was significantly higher in the denosumab treatment group compared to the corresponding cost of bisphosphonate therapy (2412.00€ ± 123.50 and 1760.00€ ± 141.3; p=0.0007) (Figure 3C). Separately for each sub-category of bisphosphonates the average total cost per patient was 1778.79 € ± 177.87 for alendronate, 1559.77 € ± 718.75 for risedronate, 1698.88 € ± 234.59 for ibandronate and 2149.27 € ± 1000.00 for zoledronic acid.
When the costs were calculated only for patients adhering to treatment, the mean total cost of treatment in the denosumab treatment group was significantly higher than the corresponding cost of bisphosphonate therapy (2344.83€ ± 168.88 and 1721.80€ ± 194.5; p=0.018) (Figure 3D).
Cost- effectiveness analysis
Based on these data, the effectiveness of treatment with denosumab (EDn) is 0.45 and with bisphosphonates (EBs) 0.24. Thus, the incremental cost effectiveness ratio (ICER) between of treatment with denosumab and treatment with bisphosphonates is 3105 €. Therefore, treatment with denosumab is not cost-effective in relation to bisphosphonate therapy in terms of achieving treatment goals. In order to achieve cost- effectiveness a discount of the cost per unit of denosumab by 30% is necessary. Comparing denosumab with each type of bisphosphonates separately, denosumab was not cost- effective compared to alendronate (ICER 3165 €), risedronate (ICER 3408 €) and ibandronate (3961 €). Concerning, bisphosphonates ibandronate had the best cost-effectiveness ratio.
Analysis of the cost-effectiveness of the two treatments in patients with adherence to treatment showed that denosumab was costeffective compared to oral bisphosphonates with an ICER of 1832.47 €, suggesting that increasing adherence is also a valuable approach for achieving cost- effectiveness of treatment with denosumab.
This study evaluated the effectiveness and cost- effectiveness of denosumab compared to standard bisphosphonate therapy for the treatment of postmenopausal osteoporosis in Greece.
Both bisphosphonate therapy and therapy with RANK-L inhibitors are worldwide first-line therapies for modifying the risk of osteoporotic fractures and especially hip fractures. The metaanalysis of Lyu et al. of 2019 evaluated data of 10 RCTs, with a total of 5361 patients, in which the efficacy of bisphosphonate or denosumab treatment was compared [18]. Denosumab significantly improved BMD of the femoral neck and of the spine compared to bisphosphonates 12 and 24 months after starting treatment. However, only one out of ten studies showed that denosumab treatment significantly reduced the risk of osteoporotic fracture. The meta-analysis of Wu et al of 2018 included 11 RCTs with a total of 5446 patients [19]. Although the relative risk of developing osteoporotic fracture did not differ between treatment with denosumab or bisphosphonates, only treatment with denosumab led to a significant increase in BMD in the hip, femoral neck, spine and radius.
The lack of data from patients in Greece renders the assessment of the efficacy of these therapies in the Greek population as well as the economic evaluation of these strategies very difficult, as the analysis must be based on data from other countries or on approximate data. For this reason, this study was based on the retrospective collection and analysis of real clinical data from postmenopausal Greek women who received anti- osteoporotic treatment. The purpose was to collect primary data with the aim of documenting the effectiveness of the above treatments in Greek patients as well as comparing these methods in terms of their economic efficiency.
In this study we chose to perform a cost- effectiveness analysis against cost-utility or cost-benefit analysis, as these are interventions with similar results. In addition, this indicator can be used more easily than QALYs in clinical practice [20]. Moreover, we chose to retrospectively analyse clinical data collected from Greek women instead of the common use that is the Markov model. While economic modelling offers useful data for determining health policies, it is essential that these data are supplemented by data from randomized or retrospective studies [11,21,22]. Without clinical data, there is a risk of miscalculating both the cost and effectiveness of the treatment method. Also, due to the lack of data in the Greek population, the creation of a Markov model for the study of osteoporosis in Greece requires the use of data from other populations.
A review of the literature shows that many of the existing economic analyses are based on individual performance indicators that are related either to individual parameters of bone density measurement (T-score, BMD) or exclusively on the theoretical risk of fracture [8,15,23,24]. A major finding of this study is the inefficiency of such individual parameters as indicators of treatment efficacy. Based on the findings in the study population it turns out that two treatments, such as bisphosphonates and denosumab, which are generally considered to be effective, could not significantly improve each of the bone density measurement parameters. Even more important is the finding that both the risk of major osteoporotic fracture and the risk of hip fracture increased despite ongoing treatment. A hasty interpretation of the above findings could lead to the erroneous conclusion that both treatments are ineffective. However, the fracture risk is individualized and adapted to the characteristics of each patient. Each indicator used to assess the effectiveness of anti-osteoporotic therapy should have similar characteristics. The efficiency index used in this study, which incorporates the FRAX® algorithm and the treatment goals of the Greek Osteoporosis Foundation, estimates the change in both the individual parameters of the DXA (T-score, BMD), as well as the demographic characteristics of the individual and the risk factors that are associated with increased risk of incident fractures. Based on the above index, it appears that denosumab has a significantly higher probability than bisphosphonates of achieving the therapeutic goals set by the Hellenic Osteoporosis Foundation for the treatment of postmenopausal osteoporosis. This benefit is however accompanied by a significant increase in treatment costs, which is owed to the significantly higher price of denosumab compared to oral bisphosphonates. Herein relies the importance of the cost analysis, on which the decision making of NHS should be based.
According to the results of the analysis, denosumab is not costeffective compared to alendronate, risedronate and ibandronate for treating post- menopausal osteoporosis in Greek women. Looking back at the literature, there are contradicting results concerning costeffectiveness of denosumab compared to oral bisphosphonates. A cost-benefit analysis, which compared denosumab with zoledronic acid for post- menopausal osteoporosis in Greece, showed that denosumab is cost effective compared to non-treatment and equivalent to zoledronic acid in terms of efficacy and relative cost per QALY gained [12]. Another cost- benefit analysis compared using a Markov showed that denosumab is economically costeffective against non-treatment or treatment with bisphosphonates, with an ICER ranging from € 10829-€ 24927 [13]. In a study from Sweden, denosumab is cost- effective against alendronate (27000 €) and risedronate (12000 €) [24]. On the contrary, a study from Australia concluded that a price reduction of 50% is necessary in order for denosumab to be cost- effective compared to alendronate [25]. Similar to this study, we concluded that a discount in the price of denosumab of 30% is needed for denosumab to be costeffective against oral bisphosphonates.
An important finding of this study was the importance of adherence to treatment for the achievement of cost- effectiveness. In this study population adherence of 48% was documented which is consisted with average adherence documented in previous studies [26]. In our study adherence was independently associated with the treatment effectiveness. Moreover, denosumab proved to be cost- effective against treatment with oral bisphosphonates in the subgroup of patients adhering to treatment. Therefore, increasing patient’s adherence, through improved patient education and health care provider-patient interaction, may improve adherence and increase cost- effectiveness of anti- osteoporotic treatment.
This analysis is a different approach to the economic evaluation of osteoporosis treatments, as it is based on factual clinical data rather than a theoretical model. However, the collection of clinical data is accompanied by some key limitations. First, the representativeness of the sample, as data was collected only from structures within the prefecture of Attica. The confirmation of the finding in a nationwide sample, although being a very demanding process, is of particular importance, so that it is possible to draw safe conclusions for the Greek population. Second, the time horizon of the analysis. The limited time horizon may underestimate the incidence of osteoporotic fractures, which clearly affect the efficacy and cost of treatment. Finally, the cost sources used do not include the outpatient cost of an osteoporotic fracture, such as costs for rehabilitation or disability related costs. This form of cost was not evaluated, as it was not possible to collect the necessary data from all patients and unavoidably leads to an underestimation of treatment costs. However, as the analysis is done from the point of view of the health system and most of this cost, especially in Greece, falls on the family budget and not the NHS, and since the observed osteoporotic fractures did not differ significantly between the two treatment groups, it was considered that the importance of this cost for the comparison between groups.
Denosumab is characterized by significantly greater effectiveness in treating post- meaopausal osteoporosis in Greek women compared to oral bisphosphnate treatment. However, its systematical use is limited due to the high costs of the pharmaceutical product. From the point of view of the NHS, ways to reduce the price of denosumab treatment or increase patient’s adherence to treatment should be evaluated in order to render treatment with denosumab cost- effective.
Authors' contributions
GR and AZ designed the study. GR, EG, NR and AG collected and analyzed the patient data. GR wrote the manuscript under the supervision of AZ with all authors contributing to writing and providing feedback. AZ oversaw the research program.
Disclosures
Georgios Renieris, Eleni Georgaki, Natalia Renieri, Athanasios Georgokostas and Athanasios Zafeirakis declare that they have no conflict of interest.
Citation: Renieris G, Georgaki E, Renieri N, Georgokostas A, Zafeirakis A (2020) Cost-Effectiveness Analysis of Denosumab Compared to Bisphosphonates for Treating Post- Menopausal Osteoporosis in Greece. J Osteopor Phys Act. 9:245. doi: 10.35248/2329-9509.21.9.245
Received: 14-Mar-2021 Accepted: 01-Apr-2021 Published: 08-Apr-2021 , DOI: 10.35248/2329-9509.21.9.245
Copyright: © 2021 Renieris G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.