Research - (2022)Volume 7, Issue 4
Background: Radiotherapy is an effective curative treatment option for intermediate-to-high-risk localized prostate cancer. Given that no significant difference was observed in survival and toxicities, we evaluated the cost-effectiveness of ultra-hypo fractionated radiotherapy and conventionally fractionated radiotherapy for intermediate-to-high-risk localized prostate cancer from the Chinese payer perspective.
Methods: We developed a Markov model with a 15-year time horizon to compare the cost and effectiveness of ultra- hypo fractionated radiotherapy with those of conventionally fractionated radiotherapy for localized intermediate- to-high-risk prostate cancer. Outcomes were measured in Quality-Adjusted Life-Years (QALYs), Incremental Cost- Effectiveness Ratio (ICER), and Willingness-To-Pay (WTP). Univariable and probability sensitivity analyses were performed to evaluate the robustness of the Markov model.
Results: Based on the results of our Markov model, the conventionally fractionated radiotherapy yielded 2.32 QALYs compared with 2.14 QALYs in the ultra-hypo fractionated radiotherapy in China. The cost of ultra-hypo fractionated radiotherapy was found to be decreased by about 14% folds ($4251.04) in comparison to that of conventionally fractionated radiotherapy. The ICER of conventionally fractionated radiotherapy vs the ultra-hypo fractionated radiotherapy was $23,616.89 per QALY in China. The most sensitive parameters were the ultra-hypo fractionated radiotherapy utility of Failure-Free Survival (FFS) with grade two or worse urinary toxicity and discount rate per annum. The cost effectiveness acceptability curve showed that conventionally fractionated radiotherapy had a 57.7% probability of being cost-effective at the Chinese WTP threshold.
Conclusion: The ultra-hypo fractionated radiotherapy was not a cost-effective strategy compared with conventionally fractionated radiotherapy in patients with localized intermediate-to-high-risk prostate cancer from the perspective of the Chinese payers. However, steep reductions in the grade two or worse urinary toxicity of the ultra-hypo fractionated radiotherapy could alter the results.
Prostate cancer; Ultra-hypo fractionated radiotherapy; Conventionally-fractionated radiotherapy; Markov model
Globally, prostate cancer is the second most common malignant tumor affecting millions of middle-aged and elderly men. According to the latest report in 2018 its morbidity ranked second (13.5%) and its mortality ranked fifth (6.7%). [1] In China, the incidence of prostate cancer has increased by more than twofold from 1992 to 2017 [2]. Approximately 80% of patients were localized at diagnosis, and about 30%-40% of patients developed distant metastasis and ultimately succumbed to the disease within five years after the initial diagnosis.
Radiotherapy in combination with androgen-deprivation therapy is well established as treatment for intermediate to high risk localized prostate cancer [3]. One particular area of interest is which radiotherapy approach is more suitable for intermediate to high-risk cases. Given the alpha/beta ratio for prostate cancer is less than 3 Gy, hypo fractionated radiotherapy a higher dose per fraction with a fewer fractions of radiation--has been intensively studied in prospective clinical trials in localized prostate cancer [4,5]. The hypo fractionated radiotherapy ranged from 2.4 Gy to 3 Gy per fraction with 4-6 weeks, resulting in a total dose of 60-70 Gy, while the ultra-hypo fractionated radiotherapy included 35 Gy in 5 fractions or 36.25 Gy in 5 fractions with 1-2 weeks. A recent metaanalysis confirmed the results in overall survival (HR=1.12, 95% CI: 0.93-1.35, p=0.219) and prostate cancer-specific survival (HR=1.29, 95% CI: 0.42-3.95, p=0.661) for hypo fractionated radiotherapy were comparable to conventionally fractionated radiotherapy [6-9]. Similarly, ultra-hypo fractionated radiotherapy as compared with conventionally fractionated radiotherapy did not improve 5-year disease-free survival without decrease and late gastrointestinal and genitourinary toxicities in intermediate and high risk patients with prostate cancer. The cost-effectiveness between ultra-hypo fractionated radiotherapy and conventionally fractionated radiotherapy is of utmost importance when determining the best treatment scheme for patients with intermediate and high risk localized disease [10-12].
Recent advances in imaging and treatment planning have made it possible to provide shorter and more convenient schedules at higher doses [13]. Although several economic analyses of Intensity Modulated Radiotherapy (IMRT) existed and resulted in greater output of health gains at a lower cost compared to threedimensional radiation therapy [14-16]. Radiotherapy access was often in short supply worldwide and virtually not extensively used in the developing countries [17]. The use of ultra-hypo fractionated radiotherapy with shorter treatment courses can reduce travel expenses and increase patient convenience, especially now during the COVID-19 pandemic [18].
Given that ultra-hypo fractionated radiotherapy provides additional biological benefit, increases patient convenience and is associated with expensive equipment, the relative economic value of this treatment has received little attention. To address this issue, we developed a Markov simulation model to evaluate the cost-effectiveness of ultra-hypofractionated radiotherapy compared with conventionally fractionated radiotherapy in patients with intermediate-to-high-risk localized prostate cancer from the perspective of the Chinese payer.
Study design of the HYPO-RT-PC trial
HYPO-RT-PC was a multi-national, randomized, open-label, phase III clinical trial with a non-inferiority design (Table 1). Patients with intermediate-to-high-risk localized prostate cancer received either 42.7 Gy in seven fractions for 2.5 weeks with an interval of one day in the ultra-hypo fractionated radiotherapy group or 78 Gy, 2 Gy/fraction, 5 days per week over an 8-week period in the conventional fractionated radiotherapy group. No patients received androgen deprivation therapy in two groups. 120 (20%) patients and 118 (20%) patients received volumetric-modulated arc therapy or intensity-modulated radiotherapy with ultra-hypo fractionated radiotherapy group and conventional fractionated radiotherapy group respectively. All patients in two groups received image-guided radiotherapy technique (IGRT). The proportion and duration of treatment regimens used in second and third-line metastatic prostate cancer treatment were not applied in HYPO-RT-PC trial [19].
| Characteristics | CRT(n=591) | UHRT(n=589) | P-value |
|---|---|---|---|
| Age (years, range) | 69(65-72) | 68(64-72) | |
| Intermediate risk (n, %) | 527(89%) | 527(89%) | |
| High risk (n, %) | 64(11%) | 62(11%) | |
| 3DCRT (n, %) | 471(79.7%) | 471(80%) | |
| VMAT/IMRT (n, %) | 120(20.3%) | 118(20%) | |
| BED (Gy) | 130 | 129.52 | |
| Total radiotherapy dose (Gy) | 78 | 42.7 | |
| Frequency of radiotherapy (f) | 39 | 7 | |
| Single dose of radiation (Gy) | 2 | 6.1 | |
| Total time of radiotherapy (days, range) | 57(55-59) | 16(15-17) | |
| The 5-year failure-free survival rate | 84% | 84% | 0.99 |
| The 5-year overall survival rate | 96% | 94% | 0.62 |
| Urinary toxicity (≥grade 2) | 2% | 6% | 0.0037 |
Table 1: Baseline demographics, clinical characteristics, and radiotherapy details were recorded between CRT and UHRT in HYPO-RT-PC trial.
Markov model
According to HYPO-RT-PC trial (ISRCTN45905321) protocol, a Markov model programmed in Tree Age Pro software 2011 (Tree Age Software LLC, Williamstown, Massachusetts) was used for comparing the economic consequences and therapeutic efficacy of ultra-hypo fractionated radiotherapy from the Chinese payer perspective.[11] Three states were included: failure-free survival (FFS), progressive survival (PS) and death (Figure 1). Moreover, a 15-year time horizon with one-month cycles has been used, that is, almost all patients were assumed to live for less than 15 years in the model. The average healthy life expectancy reached 83 years with a 15-year time horizon in our study, which was more than estimated life expectancy at age 60 years in men in China according to the World Health Organization (WHO) reports [20]. All patients started in the FFS state and then they could either enter progressed to the PS or death state based on transition probabilities. The PS state could not progress to the FFS state, and death was an absorbing state (Figure 2). Because there was only FFS and overall survival at 5 years after diagnosis in HYPO-RT-PC trial, the survival data between 5 and 15 years was obtained from previously published paper. Kaplan-Meier survival data presented graphically were extracted from survival curves using Web Plot- Digitizer (Https://apps.automeris.io/wpd/index.zh_CN.html). Furthermore, these survival data were used to fit parametric survival models [21,22]. The survival models of two groups were fitted with Weibull distribution function. Transition probabilities between health states in the model were derived from published literature, whenever possible, preferentially using utility measurements acquired prospectively. The transition probability from FFS to death was 0.0003 of Sweden's all-cause death probability [23]. The transition probability from FFS to PS and PS to death in each cycle was estimated by the formula: P(t→t+1)=-exp[λ(t)^γ-λ(t+1) ^γ )], which t stood for the current cycle number in the Markov mode [24].

Figure 1: A network of three health states.

Figure 2: Abbreviated decision tree and Markov model used to compare CRT and UHRT for intermediate-to-high-risk localized prostate cancer.
Utility and cost
The quality-adjusted life year (QALY) was a measure which constituted a combination of length and quality of life, calculated as the product of a utility value, from 0 for death to 1 for perfect health. The Quality of Life 5D-5L (EQ-5D-5L) instrument was used measurement of Health‐related quality of life [25,26]. The utilities of different health states in patients with prostate cancer were collected from previously published the literature (Table 2). From the perspective of Chinese society, our study took into account direct medical costs, including radiotherapy, urinary toxicity, digital rectal examination, blood test, imaging examination, hospitalization, androgen deprivation therapy, chemotherapy and supportive treatment costs (Table 3). We assumed that all patients received a total of 24 months of adjuvant androgen deprivation therapy based on the National Comprehensive Cancer Network (NCCN) practice guideline for prostate cancer [27]. Those treatment costs were obtained from national price announcement in the third-grade first-class hospitals in Chengdu, China. Direct non-medical costs only took into account transportation costs. We did not consider indirect labor costs because of the average age of two groups being more than 60 years, which was the official age of retirement in China [28].
| Parameter | Health utility value mean (Range) | References | Distribution |
|---|---|---|---|
| The utility of biochemical recurrence | 0.74(0.592-0.888) | [37, 38] | β |
| The utility of clinical metastasis | 0.25(0.2-0.3) | [37, 38] | β |
| U_CRT_UT | 0.91(0.7274-1) | [37, 38] | β |
| U_UHRT_UT | 0.85(0.7265-1) | [38] | β |
| U_PS | 0.61(0.49-0.73) | [10, 37, 38] | β |
| Discount rate (%) | 3(0-8) | [25] | β |
Table 2: Model parameters and assumptions were summarized.
| Unit cost ($) | CRT | UHRT | References | Distribution |
|---|---|---|---|---|
| Radiation oncologist | 2.17(1.74-2.61) | 2.17(1.74-2.61) | [41] | γ |
| Pelvic enhanced CT | 83.94(67.16-100.73) | 83.94(67.16-100.73) | [41] | γ |
| Mask design and production | 13.92(11.13-16.70) | 13.92(11.13-16.70) | [41] | γ |
| Body membrane | 78.29(62.63-93.95) | 78.29(62.63-93.95) | [41] | γ |
| Body frame | 5.22(4.18-6.26) | 5.22(4.18-6.26) | [41] | γ |
| Real-time radiotherapy monitoring | 7.25(5.80-8.70) | 7.25(5.80-8.70) | [41] | γ |
| Complex analog positioning of special X-ray machine | 135.70(108.56-162.84) | 135.70(108.56-162.84) | [41] | γ |
| Specific computer treatment planning system (TPS) | 316.06(252.85-379.27) | 316.06(252.85-379.27) | [41] | γ |
| Intensity modulated radiation therapy (IMRT) | 173.98(139.18-208.77) | 173.98(139.18-208.77) | [41] | γ |
| X knife therapy (first time) | 724.91(579.93-869.89) | [41] | γ | |
| X knife therapy | 362.46(289.96-434.95) | [41] | γ | |
| Image guided radiotherapy (IGRT)(first time) | 195.15(156.12-234.18) | [41] | γ | |
| Image guided radiotherapy (IGRT) | 160.64(128.51-192.77) | [41] | γ | |
| Routine blood test | 2.75(2.20-3.31) | 2.75(2.20-3.31) | [41] | γ |
| Biochemistry blood test | 14.50(11.60-17.40) | 14.50(11.60-17.40) | [41] | γ |
| Electrocardiogram | 4.93(3.94-5.92) | 4.93(3.94-5.92) | [41] | γ |
| Transportation cost | 1.45(1.16-1.74) | 1.45(1.16-1.74) | Local estimate | γ |
| Hospitalization fees/day | 10.87(8.70-13.05) | 10.87(8.70-13.05) | [41] | |
| Upper abdominal plain+pelvic enhanced MRI | 310.99(248.79-373.18) | 310.99(248.79-373.18) | [41] | γ |
| Head plain CT | 72.49(58.00-86.99) | 72.49(58.00-86.99) | [41] | γ |
| Bone scan | 145(116-174) | 145(116-174) | ||
| Digital rectal examination | 2.17(1.74-2.61) | 2.17(1.74-2.61) | [41] | γ |
| PSA | 14.21(11.37-17.05) | 14.21(11.37-17.05) | [41] | γ |
| Goserelin (month) | 396.67(317.33-476.01) | 396.67(317.34-476.01) | [41] | γ |
| Bicalutamide (month) | 72.49(57.99-86.99) | 72.49(57.99-86.99) | [41] | γ |
| Docetaxel (month) | 644.94(515.95-773.93) | 644.94(515.95-773.93) | [41, 42] | γ |
| Abitrone (month) | 579.61(463.69-695.53) | 579.61(463.69-695.53) | [41, 42] | γ |
| Kabatasai (month) | 5617.80(4494.23-6741.35) | 5617.79(4494.23-6741.35) | [41, 42] | |
| Supportive treatment (month) | 543.70(434.96-652.45) | 543.70(434.96-652.45) | [43] | γ |
| Urinary toxicity | 960(768-1152) | 960(768-1152) | [37] | γ |
Table 3: Key cost parameters and related assumptions.
Cost-effectiveness analysis
All costs were presented in 2020 US dollar and future costs and health outcomes were discounted to the current year with annual rate of 3%, reflecting an average annual inflation rate in China [29]. Clinical effectiveness was expressed in QALYs, which was calculated as the sum of the product of health utilities weight in a given state and the number of life years gained, [30] cost-effectiveness analysis was evaluated using incremental cost-effectiveness ratios (ICERs) between ultra-hypo fractionated radiotherapy and conventionally fractionated radiotherapy. The willingness-to-pay (WTP) threshold value for cost-effective analysis was 3 times Gross Domestic Product (GDP) per Capita of China in 2020, which was set at $31,510 per QALY according to WHO guidelines [30-32].
Sensitivity analysis
The robustness of our model parameters was estimated by one- way sensitivity analysis and probability sensitivity analysis. A series of deterministic sensitivity analyses were performed to test the robustness of base case results. The parameters were obtained by varying the base case by 20% in the deterministic sensitivity analysis [33]. We assumed a beta probability distribution for the health utility values, and a gamma distribution for cost parameters (Tables 2 and 3). Moreover, the discount rate considered as β distribution was varied (0%-8%) within the sensitivity analysis (Table 2). The one-way sensitivity analysis results were demonstrated as a tornado diagram with the most influential model parameters. We performed probabilistic sensitivity analyses with 1000 Monte Carlo simulations with all of the input variables varied simultaneously with a specific pattern of distribution. Last, a second-order Monte Carlo simulation was developed to estimate the expected values of costs and effectiveness in the base case [34].
Base case results
Based on the results of our Markov model, the conventionally fractionated radiotherapy yielded 2.32 QALYs compared with 2.14 QALYs in the ultra-hypo fractionated radiotherapy in China (Figure 3). Treatment with the conventionally fractionated radiotherapy cost $34,411.85 compared with $30,160.81 for the ultra-hypo fractionated radiotherapy. The cost of ultra-hypo fractionated radiotherapy was found to be decreased by about 14% folds ($4251.04) in comparison to that of conventionally fractionated radiotherapy. The ICER of conventionally fractionated radiotherapy vs the ultra-hypo fractionated radiotherapy was $23,616.89 per QALY in China. The details were listed in Table 4.
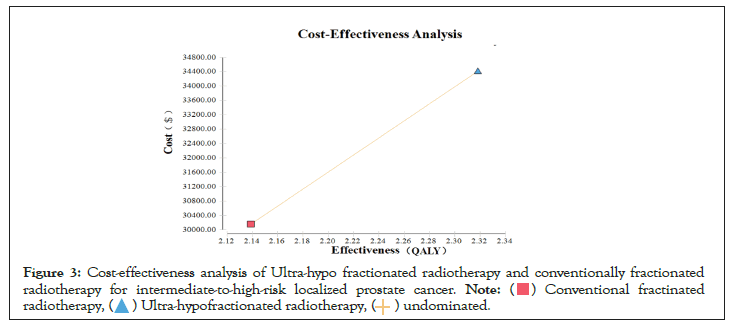
Figure 3: Cost-effectiveness analysis of Ultra-hypo fractionated radiotherapy and conventionally fractionated
radiotherapy for intermediate-to-high-risk localized prostate cancer.

| CRT | UHRT | |
|---|---|---|
| Effectiveness (QALYs) | 2.32 | 2.14 |
| Cost ($) | 34411.85 | 30160.8 |
| Incremental Effectiveness (QALYs) | 0.18 | / |
| Incremental Cost ($) | 4251.04 | / |
| Incremental Cost/ Effectiveness ($ /QALY) | 23616.89 | / |
| Average Cost/Effectiveness ($/QALY) | 14843.97 | 14102.6 |
Table 4: Cost-effectiveness analysis of CRT and UHRT.
Sensitivity analysis
The results of one-way sensitivity analysis of our Markov model were presented in Figure 4. The most sensitive parameters were the ultra-hypo fractionated radiotherapy utility of FFS with grade two or worse urinary toxicity and discount rate per annum. When the utility of FFS with grade two or worse urinary toxicity of ultra- hypo fractionated radiotherapy varied from 0.72 to 0.77, the ICER of conventionally fractionated radiotherapy vs the ultra-hypo fractionated radiotherapy ranged from $32,615.86 per QALY to $5,850,488.91 per QALY, which exceeded the WTP threshold of $31,510 per QALY. In addition, conventionally fractionated radiotherapy was no longer cost-effectiveness when the discount rate per annum was 3.68% or more.

Figure 4: One-way sensitivity analysis. This diagram shows the incremental cost effectiveness ratio (ICER) of CRT
for different model input parameters from the perspective of Chinese society.

Figure 5 illustrated the cost effectiveness acceptability curve associated with the proportion of the intervention at any threshold value of WTP. The cost effectiveness acceptability curve showed that conventionally fractionated radiotherapy had a 57.7% probability of being cost-effective at the Chinese WTP threshold. When the hypothetical WTP threshold increased to $141,795, the probability for conventionally fractionated radiotherapy to be cost-effective was 69.3%.
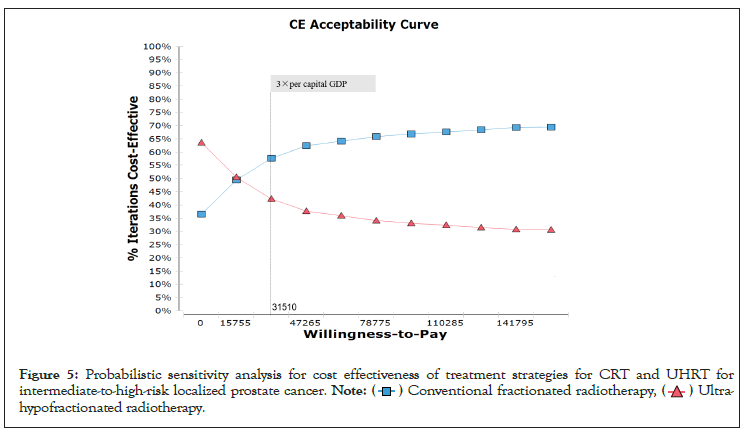
Figure 5: Probabilistic sensitivity analysis for cost effectiveness of treatment strategies for CRT and UHRT for
intermediate-to-high-risk localized prostate cancer.

Our study demonstrated that treatment with conventionally fractionated radiotherapy yielded an additional 0.18 QALYs than treatment with ultra-hypo fractionated radiotherapy, leading to an ICER of $23,616.89 per QALY in China. Although the unit cost of ultra-hypo fractionated radiotherapy was found to be decreased by about 14% folds ($4251.04) in comparison to that of conventionally fractionated radiotherapy, the ultra-hypo fractionated radiotherapy was not a cost-effective strategy in patients with localized intermediate-to-high-risk prostate cancer from the perspective of the Chinese payers.
In recent years, costs were derived from the continuous advancement of technology and the upgrading of radiotherapy relevant devices. Compared with tridimensional radiotherapy (3D-RT), the incremental cost of IMRT for prostate cancer was $5,553.78 in the Brazilian health system [35]. Given no differences in radiotherapy relevant devices in HYPO-RT-PC trial, the cost of the ultra-hypo fractionated radiotherapy was less than that of conventionally fractionated radiotherapy in our study. In the previous published cost-effectiveness analysis, stereotactic body radiotherapy (SBRT) consisted a total dose of 37 Gy over 5 fractions was the most cost-effective radiation treatment modality in patients with intermediate-risk prostate cancer [36]. However, SBRT with better long term outcomes was a prerequisite for a highly accessible and more cost-effective intervention. In fact, a phase III HYPO-RT- PC trial, the first randomized controlled trial comparing ultra-hypo fractionated to conventional fractionation, confirmed that ultra- hypo fractionated radiotherapy resulted in higher grade two or worse genitourinary toxicity, but did not improve FFS in patients with localized intermediate-to-high-risk prostate cancer.
The optimal utility of FFS for ultra-hypo fractionated radiotherapy remained to be determined and the cost-effectiveness had a strong relationship with the cost of grade two or worse urinary toxicity. The utility of prostate cancer and treatment-related health states was rarely reported in patients with ultra-hypo fractionated radiotherapy in China, we obtained the utility values from previous published studies [37-39]. The most sensitive parameters were the ultra-hypo fractionated radiotherapy utility of FFS with grade two or worse urinary toxicity in the tornado diagrams. The results of one-way sensitivity analysis revealed that conventionally fractionated radiotherapy was not a cost-effective strategy in
patients with localized intermediate-to-high-risk prostate cancer when utility of FFS with grade two or worse urinary toxicity of ultra-hypo fractionated radiotherapy varied from 0.72 to 0.77. However, the utility of FFS for symptoms occurring with treatment varied from 0.71 to 0.89 in previous published cost-effectiveness analyses, and it was likely to have substantially altered the results of ICER. Most patients did not receive the combination of IMRT with IGRT in HYPO-RT-PC trial, which was widely used for ultrahypo fractionated radiotherapy in China. Therefore, the utility of prostate cancer and treatment-related health states in China was more urgently needed in order to cost-effectiveness analysis in the future [40].
Some limitations of the present study have to be discussed. Firstly, limitations in our study were raised primarily from the quality of inputs used to inform the Markov model. We did not have access to utility and transition probability from the real world study in China. We acquired transition probability by simulating the survival curve, which was a method adopted by other similar cost-effectiveness studies [41,42]. In addition, due to the lack of long-term outcomes in China, we obtained the main data on main outcomes of interest from patients in Sweden and Denmark. Third, differences of late toxicities between ultra-hypo fractionated radiotherapy and conventionally fractionated radiotherapy were not considered in the presented study. Lastly, some other factors, such as the time away from home, education and religion, would influence the choice of treatment protocol for the patients with localized intermediate-to-high-risk prostate cancer [43].
In conclusion, compared to conventionally fractionated radiotherapy, the ultra-hypo fractionated radiotherapy was not a cost-effective strategy in patients with localized intermediateto- high-risk prostate cancer from the perspective of the Chinese payers. However, steep reductions in the grade two or worse urinary toxicity of the ultra-hypo fractionated radiotherapy could alter the results.
Not applicable
Conceptualization, JxH and ClL. Methodology, JxH and QfW. Writing original draft, JxH, QcH and ClL. All authors contributed to reviewing the manuscript and approved the submitted version.
No fundings are involved in this study.
All data analyzed during this study are included in the main article. Any other questions should be directed to the corresponding author.
Not applicable.
All co-authors have agreed and approved the final manuscript.
The authors declare that they have no other financial or nonfinancial competing interests.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: He J, Wang Q, Hu Q, Li C (2022) Cost-Effectiveness Analysis of Ultra Hypo fractionated Radiotherapy and Conventionally Fractionated Radiotherapy for Intermediate to High Risk Localized Prostate Cancer. Immunogenet Open Access. 7:172.
Received: 06-Jun-2022, Manuscript No. IGOA-22-18335; Editor assigned: 10-Jun-2022, Pre QC No. IGOA-22-18335 (PQ); Reviewed: 24-Jun-2022, QC No. IGOA-22-18335; Revised: 01-Jul-2022, Manuscript No. IGOA-22-18335 (R); Published: 08-Jul-2022 , DOI: 10.35248/IGOA.22.7.172
Copyright: © 2022 He J, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.