Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2022)Volume 10, Issue 4
Background: COVID-19 has afflicted the health of children all age groups. Perinatal transmission of SARS-CoV-2 is mainly horizontal; the vertical transmission of COVID-19 is a debate subject.
Methods: We conducted a retrospective study in the neonatal ICU of Harouchi Mother and Child Hospital in Casablanca, Hassan II University Casablanca, Morocco from March 15, 2020 to December 31, 2021. Our purpose is to describe the epidemiological, clinical, therapeutic, and outcome profile of newborns infected by Sars-cov2 and to discuss the possibility of maternal-fetal transmission.
Results: Eighty-eight newborns were hospitalized in the COVID isolation unit, Eighteen newborns got infected; eight of them by probable maternal-fetal transmission and ten post-natal infection. The diagnosis was confirmed by PCR; the main symptom was respiratory distress, followed by fever; all symptomatic newborns received supportive treatments.
Conclusion: Infection of the newborn by SARS-CoV-2 is a little studied subject. Data collection is necessary in order to establish guidelines adapted to this population.
COVID-19; Newborns vertical transmission; Maternal-fetal transmission
The "Corona Virus Disease 2019" (COVID-19) pandemic linked to "SARS-CoV-2 was declared a global health crisis by the World Health Organization (WHO) at the end of January 2020.So far as we know, people of all ages are susceptible to SARS-CoV-2. Few cases of neonatal COVID-19 have been reported to date, and little is known regarding route of infection, clinical presentation, management, and outcome. As a precautionary principle, newborns represent a group of vulnerable patients considered potentially at risk, but who ultimately prove to be asymptomatic and paucisymptomatic, as indicated by low incidences and severity of the published pediatric cases
The data about maternal-fetal transmission is controversial; it is the subject of numerous studies; several cases of perinatal transmission have been reported based on positive tests of newborns at day 1 of life. However, the long and short-term effects of COVID-19 infection are still blurred and must be more studied [1].The purpose of this study is to describe the epidemiological, clinical, therapeutic, and outcome profile of newborns infected by Sars- cov2 and to discuss the possibility of maternal-fetal transmission.
We conducted a retrospective study in the neonatal Intensive Care Unit (ICU) of Harouchi Mother and Child Hospital in Casablanca, Hassan II University (Casablanca, Morocco from March 15, 2020 to December 31, 2021. Data collection was done using patient medical records. In this unit were admitted newborns having postnatal symptoms suspects of COVID-19 and those born by positives mothers at the time of childbirth. The newborns from COVID-positive mothers were immediately transferred for isolation and observation, separating from their mothers, contact and breastfeeding where not allowed before Polymerase Chain Reaction (PCR) COVID who was systematically performed between 24 and 48 hours.
A positive PCR nasopharyngeal swab retained the infection with SARS-CoV-2. Newborns who died before performing PCR were excluded from this study and those whose didn’t benefit from PCR.
The Protéine C-Reactive (CRP) was considered negative when the rate was <20 mg/l. Neutropenia has consider when neutrophil count was ≤ 1500 cells/L. Lymphopenia has consider when Lymphocyte count was ≤ 2000 cells/L. Thrombocytopenia has considered when the Platelets was ≤ 150 × 10/L.
During this period, eighty-eight newborns with suspected SARS- COV-2; were hospitalized in the COVID isolation unit, sixty-two newborns were born by positive mothers at the time of childbirth, and twenty six of them were admitted with a postnatal infection symptom. Eighteen newborns had a positive PCR; eight of them got infected by probable maternal-fetal transmission and ten post-natal infections. The Figure 1 summarizes the distribution of patients.
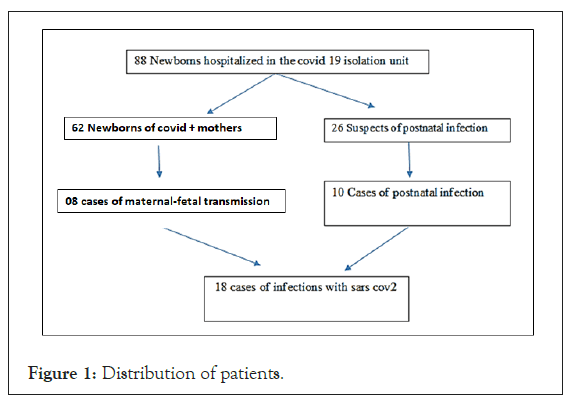
Figure 1: Distribution of patients.
Epidemiological characteristics
Concerning the newborns from COVID-positive mothers: All mothers had symptoms of COVID-19 infection at the time of delivery, 60 of them were diagnosed before delivery, 78% of parturient suffered from severe respiratory distress requiring intensive care. In 60% of cases, the delivery was done by cesarean section because of profound maternal desaturations. All newborns of COVID mothers were admitted to Hour (H1) of life except two newborn, their mothers have been diagnose only benefited from PCR after childbirth, the first newborn was in respiratory distress, taken care of from birth without any contact with his mother. The second had contact with his mother but clinical signs were observed at H70 of life. 12% of newborns to mothers infected with COVID-19 at the time of delivery had a positive PCR at birth. Six newborns out of eight with probable maternal-fetal transmission were born by caesarean section, in five cases the caesarean section was indicated for maternal rescue with severe respiratory distress; the APGAR at 5 minute was more than 7 in 87% of cases. A median gestational age was 38SA (week of amenorrhea) (32SA- 40SA), 03 premature newborns and 05 born at term.
Regarding newborns admitted for postnatal infection: The newborns had a median age of 20 days with extremes (D14 of life and D26 of life). The sex ratio was 1:6. All the newborns were at term. The notion of SARS-CoV-2 contact was noted in seven patients. In three cases, the contaminant was undetermined.
Clinical features
Five cases of eight probable maternofoetal infections had symptoms from birth, 02 cases were initially asymptomatic and presented signs between H30 and H48 of life. One newborn had no symptoms diagnosed by the systematic screening of infants of a positive COVID mothers. The main symptom was respiratory distress observed in 06 cases, followed by fever in 05 cases (isolated in one case and associated with respiratory distress in 4 cases). Concerning postnatal infection, clinical symptoms simulated viral bronchiolitis in five newborns, febrile respiratory distress in four case, in one baby the SARS-CoV-2 infection was revealed by an isolated fever.
One patient had Down syndrome with CIV-type congenital heart disease admitted with severe respiratory distress.
Paraclinical characteristics
The COVID-19 PCR on a nasopharyngeal swab was carried out in eighty-eight patients on admission and was positive in 18 cases. Among the eight cases of probable maternofetal transmission, 2 newborns tested negative at 24 hours of life, were diagnosed after repetition of the PCR test on D5 of life in front of the worsening of their clinical conditions. The first case was a newborn of a 32 weeks COVID-positive mother. He was admitted for early neonatal respiratory distress treated initially by the non-invasive method who tested negative at birth but worsened their respiratory distress for which a repeat PCR came back positive on Day 5 of life, this newborn had radiological lesions in frosted glass at chest scanner.
The second case was a term newborn with moderate respiratory distress, PCR test at H27 of life was negative, infectious assessment was negative. Faced with worsening respiratory signs and the onset of fever, a second test was performed at day 5 of life if is found to be positive. The chest CT scan was performed in six patients; it was normal in three cases and showed frosted glass opacity in 3 cases. Among the ten cases of postnatal infection, the Chest radiography showed abnormalities in seven neonates the assessment was supplemented by a chest computed tomography CT which demonstrated the pulmonary damage of COVID-19 in 4 patients: Ground-glass opacity appearance in 3 cases, and pulmonary condensation in 01 case.
Biologically, the C reactive protein and the blood count were normal in all cases
Treatment: All symptomatic newborns received supportive treatments, azithromycin was administered to eight patients after diagnosis, and no patient was treated with hydroxychloroquine. Nine patients received antipyretic treatment (paracetamol). Continuous Positive Airway Pressure CPAP has only been used in one patient and six newborns (4 admission for postnatal infection and 2 cases of vertical transmission) required assisted ventilation intubation.
Evolution
The evolution of the eight cases of probable maternofetal infection was favorable in seven newborn. A length of stay was 14,5 days (7D-22D). One death that was a newborn of 32 weeks, admitted for early neonatal respiratory distress treated initially by the non- invasive method that tested negative at birth but worsened their respiratory distress he was intubated, the evolution was marked by deep refractory desaturations, bradycardia, complicated by death.
The epidemiological, clinical, therapeutic characteristics and evolutionary of the patients admitted for probable vertical transmission are summarized in Table 1. In the postnatal infections, the evolution was good in 08 cases, two newborns died: a newborn admitted with severe febrile respiratory distress and a newborn with Down's syndrome who had congenital heart disease (interventricular communication) admitted to D26 Severe respiratory distress with fever died the day after admission. Table 2 summarizes the characteristics of newborns admitted for postnatal SARS-cov2 infection.
| Characteristics | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Mother’s disease | ||||||||
| Symptoms | Fever/ dry cough | Dry cough / dyspnea/ desaturation | Severe respiratory distress/ desaturations | Fever | dyspnea/ Desaturation | Fever/ respiratory distress | Dyspnea, desaturation | Anosmia, Desaturation fever |
| onset of symptoms | Before delivery | Before delivery | Before delivery | Before delivery | Before delivery | Before delivery | Before delivery | Before delivery |
| Mother’s disease Nucleic acid detection | Before delivery | After delivery | Before delivery | Before delivery | After delivery | Before delivery | Before delivery | Before delivery |
| Delivery | ||||||||
| Method of delivery | Vaginal delivery | Cesarean | Cesarean | Vaginal delivery | Cesarean | Cesarean | Cesarean | Cesarean |
| Demographic | ||||||||
| Sex | Male | Male | Male | Female | Female | male | Female | Male |
| Gestational age | 38W+4D | 41W | 32W | 33W | 40W | 38W | 37W | 34W |
| Newborn disease | ||||||||
| Onset of symptoms | H1 | D2 of live | H1 | H1 | H1 | D2 of live | Asymptomatic | H1 |
| Symptoms | Fever/ Respiratory distress | fever | Respiratory distress | Fever, Respiratory distress | Fever, Respiratory distress | Respiratory distress | Asymptomatic, Respiratory distress | Fever, Respiratory distress |
| Age of diagnosis | H36 | H28 | D3 (Mother diagnosed with COVID19 positive after delivery, no contact between mother and newborn) | D5 (PCR at H 24 negative, redone on D5 due to worsening respiratory distress) | H70 | D5 PCR at H24 negative, redone on D5 due to respiratory distress | H24 | H24 |
| The chest scanner | Normal | unrealized | Ground glass surfaces+ atelectasis | Multiple Ground glass surfaces | Normal | Normal | unrealized | Ground glass surfaces |
| WBC/mm3 | 7240 | 5780 | 9220 | 8040 | 7520 | 5670 | 8556 | 9854 |
| Neutrophils/mm3 | 4800 | 3200 | 6430 | 4750 | 5240 | 2560 | 4368 | 4670 |
| Platelets /mm3 | 301000 | 189000 | 198000 | 234500 | 197000 | 205000 | 199400 | 240000 |
| CRP (mg/l) | 4,9 | 1,2 | 5,6 | 8,5 | 4,5 | 7 | 3 | 5 |
| Treatment | ||||||||
| Supportive Treatment | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Mechanical ventilation | No | No | Yes | Yes | No | No | No | No |
| Outcomes | ||||||||
| Hospital stays days | 07 days | 07 days | 10 days | 22 days | 11 days | 10 days | 07 days | 07 days |
| Evolution | Healing | Healing | Healing | Died | Healing | Healing | Healing | Healing |
Table 1: Characteristics of newborns admitted for probable vertical transmission.
| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Place of birth | At home | Out born | Out born | in born | Out born | Out born | Out born | Out born | Out born | Out born |
| Gender | Male | Female | Female | Male | Male | Female | Male | female | Male | Male |
| Admission age | D14 of life | D18 of life | D22 of life | D14 of life | D26 of life | D22 of life | D15 of life | D20 of life | D16 of life | D22 of life |
| Mother status | Negative | Negative | Negative | Positive | Negative | Negative | Negative | Positive | Negative | Negative |
| Breastfeeding mode | Breast milk | Breast milk | Breast milk | Formula | Breast milk | formula | Breast milk | Formula | Formula | Breast milk |
| viral contagious | Unknown | unknown | Sister | Mother | Sister | Mother | Father | Mother | Unknown | unknown |
| symptom onset age | D13 of life | D15 of life | D19 of life | D14 of life | D25 | D20 | D13 | D18 | D13 | D15 |
| Symptoms | simulated viral bronchiolitis | Respiratory distress+ fever | simulated viral bronchiolitis | Fever | Fever+ severe respiratory distress | simulated viral bronchiolitis | Severe respiratory Fever | simulated viral bronchiolitis | simulated viral bronchiolitis | Severe respiratory Fever |
| Thoracic CT | Normal | unrealized | Multiple Ground glass surfaces | Normal | Ground glass surfaces | Ground glass surfaces | pulmonary condensation | Normal | unrealized | unrealized |
| WBC/mm3 | 5780 | 17570 | 14220 | 13040 | 6280 | 15200 | 13450 | 7645 | 8756 | 6120 |
| Neutrophils/mm3 | 3200 | 13110 | 9730 | 6720 | 3240 | 4300 | 5600 | 5840 | 4356 | 3413 |
| Platelets/mm3 | 189000 | 247000 | 2543000 | 273000 | 245000 | 250000 | 237000 | 198000 | 190000 | 210000 |
| CRP (mg/l) | 1.2 | 3 | 2.5 | 2.8 | 5.5 | 4,3 | 9 | 6,5 | 7 | 3 |
| Treatment | ||||||||||
| Supportive Treatment: | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mechanical ventilation | No | No | Yes | No | Yes | Yes | No | No | No | Yes |
| Hospital stays days | 7 | 10 | 15 | 8 | 1 | 19 | 12 | 7 | 10 | 10 |
| Evolution | Healing | Healing | Healing | Healing | Deceased | Healing | Healing | Healing | Healing | Deceased |
Table 2: Characteristics of newborns admitted for postnatal symptoms.
SARS-CoV-2 is a new strain of coronavirus responsible for high morbidity and mortality, making it an international public health problem affecting all populations.
Pregnant women and newborns are vulnerable to this infection. Data on the maternal and perinatal outcomes of pregnant women infected with the SARS-CoV-2 are limited to a handful of case reports and series. The sample sizes are small and the findings are diverse [1-3].
Usually the newborn can be contaminated postnatal but the problem arises concerning the possibility of materno-fetal transmission. The vertical transmission of COVID-19 is a debate subject and its clinical evidence is extremely scarce. A number of reports have suggested vertical transmission, and several studies have found SARS-CoV-2 in placental tissue, amniotic fluid and cord blood; however, vertical transmission seems to be a rare complication of COVID-19 in pregnancy [4]. Wang report the case of a newborn at 40 weeks gestational age born by C-section in whom a nasopharyngeal swab performed at 36 hours of life is positive for SARS-CoV-2 [5]. Another study by Zeng found three infants whose nasopharyngeal swab PCR were positive on day 2 and 4 of life then negative from day 6 or 7 of life to note that strict measures had been put in place to avoid horizontal transmission [6]. Zamora and Coll also reported a woman delivered via C-section and the newborn tested positive 16 hours after birth [7].
In a systematic review, the results of the nucleic acid test of SARS- CoV-2 in 128 newborns were reported, including 123 newborns negative throat swab tests and five positive tests. Five infants who tested positive for SARS-CoV-2 were delivered by cesarean section. Elevated concentration of IgM and IgG against SARS-CoV-2 were detected in eight newborns whose throat swab test were negative [8].
In our study sixty two newborns born from positive mothers were hospitalized in the COVID isolation unit, eight of them were positive (12%). Possible vertical transmission was suspected in 8 patients, 05 who tested positive within the first 36 hours of their lives, 2 newborns tested negative at 24 hours of life, were diagnosed after repetition of the PCR test on D5 of life, despite immediate isolation of the mother, respect for hygiene rules, non-breastfeeding, which means that mother-to-child transmission is possible. One newborn had contact with his mother but clinical signs were observed at H70 of life, duration is short for virus incubation and clinical transmission, which makes vertical transmission probable. Hence the need to increase studies in this subject and more investigations are necessary to confirm this probability.
Postnatal transmission of SARS-CoV-2 appears to account for the majority of infections reported in neonates [9]. In the postnatal period, infants may be exposed to SARS-CoV-2 from an infected mother, other caregivers and/or the neonate’s environment, making the source of postnatal infection, should it occur, difficult to determine [10]. In our study, 10 newborns had a postnatal infection; in four cases we have not determined the contaminator.
The clinical symptoms of newborns infected with COVID-19 is variable, but the main symptom is fever, which is found almost systematically in the cases described in the literature and generally manifests itself within five to fifteen days following birth. Unlike, the adults and children, the respiratory symptoms are inconsistent. Conversely, newborns are more likely to have neurological (hypotonia, drowsiness, moans, encephalitis) or digestive symptoms [11].
In a literature review of 25 newborns with COVID-19 from December 2019 to April 27, 2020, positive newborns developed fever (28%), vomiting (16%), and cough or shortness of breath (12%) initially, while only 16% of affected newborns were asymptomatic. The major complications were pneumonia (12%), respiratory distress (8%) and sepsis (4%). In a multicenter multinational cohort study carried out in Europe, newborns with COVID-19 exhibited fever (36.7%), pneumonia (46.9%), and gastrointestinal symptoms (10.2%) [12].
In our study, the main symptom was fever observed in 10 cases (five of eight cases of vertical infection and five of ten cases of postnatal infection); it was isolated in 2 cases and associated with respiratory distress in 08 patients. One newborn of a positive COVID mother remained asymptomatic, 5 of the 10 infants infected postnatal presentedsymptoms similar to viral bronchiolitis.
Detection of viral nucleic acid by Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) is the current gold standard and confirmatory test for COVID-19; serological tests are less likely to be reactive in the first several days of infection so are less useful in diagnosis of acute infection [13].
Concerning newborns of COVID-19-positive mothers, the moment of the diagnosis seems unstandardized. A negative PCR done early can be positive afterwards. In the other hand, early nasopharyngeal swabs might yield a false positive result detecting the virus in the amniotic fluid present in the infant’s nasopharynx, especially if swabs are taken immediately after birth [14].
In infected mothers, the infant should be tested first at about 24 hours of age. However, in rare cases, the infant may test negative in 24 hours but positive in 48-72 hours. According to several studies: Positive results in 1st RT-PCR were documented in 14 babies. The earliest were tested at birth the average time of the result was 22 hours. Three babies with negative 1st RT-PCR became positive in 2nd RT-PCR at D6, D7 and at 24 hours which continued to test positive at 1 week. One baby with an equivocal result with 1st RT-PCR became positive in subsequent testing on day 3 [15]; In our study, two patients had negative PCR initially but after redone it front of clinical complication turns out to be positive at D5 of life.
Zou et al. surveyed the relationship between viral loads of SARS- CoV-2 in RT-PCR test, and the timing of swab sampling after symptoms were also detected. It seems that sensitivity of RT-PCR test depends on the source of sampling (e.g. throat, nose, etc.), time of sampling and the health care provider’s skill for performing an accurate sampling [16].
The role of antibodies in diagnosis is uncertain, as most infections occur late in pregnancy with insufficient time for antibody production. Recently, a classification system has been proposed by Shah. Based on maternal tests, clinical status of the newborn, and neonatal tests. Whereas this requires detection of the virus in placental tissue, umbilical cord blood, and amniotic fluid outside of nasopharyngeal and rectal swabs [17]. A thing that was not tested in our study.
Regarding breastfeeding in COVID-19, Scientifics agree that it must be encouraged and supported more than ever [18]. In fact, the probable passage of specific antibodies in milk, demonstrated for other respiratory viral infections, as well as the multiple antiviral and anti-inflammatory properties of breast milk, are protective factors for the breast-fed newborn. This breastfeeding must comply with hygiene measures such as wearing a mask; frequent hand washing, disinfection of all touched surfaces, washing the breasts and distancing during the evening [19,20]. In our study, during follow-up, of the 54 newborns who had a negative PCR, 46 received breast milk according to hygiene advice and none of them showed signs of sarscov2 infections in post natal.
Since few newborns have been diagnosed with COVID-19 infection, treatment recommendations and guidelines based on clinical evidence remain to be discussed, most newborns were treated with routine care measures considering in some cases, antibiotic treatment of bacterial surinfection was necessary. In symptomatic COVID-19 positive neonate, management according to the unit practice guidelines, administering broad spectrum antibiotics, respiratory support, and keeping lower threshold for surfactant therapy might be enough since other neonatal morbidities might be the cause of the infant’s clinical condition [9]. In the case who the infant’s clinical condition is not responding to the conventional therapy, the treating neonatologist might consider adding azithromycin or anti-malaria drugs to the treatment [21]. In our study, the newborns received symptomatic treatment, 5 cases required ventilator-assisted intubation, and no patient was treated with hydroxychloroquine.
In general, the prognosis of SARS-CoV-2 positive newborns remains reassuring; their favorable evolution is linked to their benign clinical pictures [22]. Clinical complications or deaths were observed in newborn babies, compared to fatality rates in adults. In Europe, A total of 49 neonates with COVID-19 were included All of them survived without any sequelae, of note, neonates with pre-existing medical conditions and preterm infants appeared to be at a higher risk of severe illness from COVID-19 [23]. In our study, three cases of death occurred by refractory hypoxia which can be correlated with the underlying ground of trisomy 21 with congenital cardiopathy in 1 case and in the other case with the prematurity. Third case consulted 5 days after the onset of symptoms with severe respiratory distress and severe pneumopathy on pulmonary radiology.
Neonatal SARS-CoV2 infection exists, although its incidence is low compared to infants, children or adults. Vertical transmission is possible but infrequent; the overall prognosis is favorable. The questionable validity of serological analyzes and the lack of standardized definitions of congenital, perinatal, and postnatal transmission, more data is needed to confirm the route of transmission and to determine management guidelines, clinicians should watch frequently for updates as the state of knowledge evolves.
The authors confirm that they have no conflict of interest.
Citation: Badre A, Lehlimi M, Toumi H, Chemsi M, Habzi A, Benomar S (2022) COVID-19 and Newborn: Experience of a University Isolation Unit. J Infect Dis Preve Med. 10:268.
Received: 29-Jun-2022, Manuscript No. JADPR-22-18144; Editor assigned: 01-Jul-2022, Pre QC No. JADPR-22-18144 (PQ); Reviewed: 19-Jul-2022, QC No. JADPR-22-18144; Revised: 22-Jul-2022, Manuscript No. JADPR-22-18144 (R); Published: 29-Jul-2022 , DOI: 10.35841/2329-8731.22.10.268
Copyright: © 2022 Badre A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.