Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2022)Volume 11, Issue 8
At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. This results in an epidemic throughout China, followed by an increasing number of cases in other countries throughout the world. Currently, containment and mitigation measures have intensified and disease-modifying pharmacologic compounds and vaccines are being developed, COVID-19 continues to spread. The 2019 novel coronavirus (2019-nCoV/SARS-CoV-2) was shown to be a Beta coronavirus (lineage B) closely related to SARS-CoV and SARS-related bat coronaviruses, and it has been reported to share a common receptor with SARS-CoV (ACE-2). At the time of this writing, the full magnitude of the public health impact poses a great threat to all humankind. More than 12 million patients have been infected globally and 564, 623 have died as of 10thjuly 2020. In this review, we highlight epidemiology, transmission, impact on pregnancy and reproductive health and future directions to control the spread of this fatal disease.
COVID-19, Epidemiology, Global distribution, Transmission, Infertility, Prevention
Coronaviruses are members of the Coronaviridae family, which consists of subfamilies namely Orthocoronavirinae and Torovirinae. Orthocoronavirinae has four genera: Alpha coronavirus (average genome size 28 kb), Beta coronavirus (average genome size 30 kb), Gamma coronavirus (average genome size 28kb), and Delta coronavirus (average genome size 26 kb) [1]. Coronaviruses are predominantly common in mammals and birds. The Alpha coronavirus and Beta coronavirus infect mammals, and while Gamma coronavirus and Delta coronavirus infect avian species [2]. Coronaviruses are zoonotic pathogens that are well known to evolve environmentally and infect many mammalian and avian species [3]. Severe acute respiratory syndrome coronavirus (SARS-CoV) emerged in 2002 in Guangdong province, China, causing an outbreak that spread to 26 countries, with more than 8000 infections and 774 deaths and a case fatality rate of 9.5% [2]. The ongoing Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak that originated in 2012 in Saudi Arabia has spread to 27 countries with 2494 infections and 858deaths, with a case fatality rate of 34.4% [4]. The recent surfacing of the novel coronavirus SARS-CoV-2 (first identified on December 12th, 2019) was initially detected in Wuhan, Hubei Province, China, and has now spread globally via travelers and breached the boundaries of 213 countries/regions [5,6]. On March 11th, 2020, the World Health Organization officially declared a global pandemic. The rapid dissemination and sharing of information during the SARSCoV- 2 pandemic has surpassed that of both MERS-CoV and SARS-CoV, where the latter virus was only identified after several months and with a genome available a month later [7]. TheSARSCoV- 2 was identified and a genome sequence was available within a month from the initial surfacing of the agent in patients [8]. SARS-CoV-2 is presumed-but not confirmed-to have originated in bats given a remarkable (89-96%) genomic homology to bat coronaviruses [2].It appears that most of the early cases had some sort of contact history with the original seafood market [9-12].
Using online databases, we conducted a literature review of epidemiology of COVID-19. The key articles used were retrieved predominantly from NCBI, Google Scholar using the terms epidemiology of COVID-19. Global distribution of COVID-19, transmission, infertility and prevention as keywords for our search. We included scientific publications from March 17, 2020 to July 10, 2020 articles focusing on epidemiology of COVID-19.
The range of COVID-19 cases reported by the WHO has been increasing following the first report of COVID-19 in December 2019 from the WHO China administrative center [13]. The infection started from the local seafood market in Wuhan, China even as the specific infection route of the first case stays unclear. Soon, a secondary chain of infection found to be human-to-human transmission by way of close contact. There were a high number of infected humans with no history of exposure to flora and fauna or traveling Wuhan, and a couple of instances of infection have been detected amongst medical specialists [14-18]. Then, the number of confirmed instances in China grew till mid-February 2020. Up to march, COVID-19 instances proceed to be said globally from over a hundred and seventy international locations as 153,517 laboratories confirmed COVID-19 cases with 5,735 deaths have been referred to according to WHO [19,20]. Research indicated that the unfold of COVID-19 cases used to be quite rapid and pronounced to countless different global locations after its outbreak in china. The cases recognized outside of China had been in particular travelers who had been infected in China and then traveled to areas out of the doors of China. Travel-related COVID-19 cases had been pronounced in the following countries: Singapore, Japan, Republic of Korea, Malaysia, Vietnam, Australia, United States of America, Germany, etc. [21]. Unfortunately, COVID-19 has begun to spread domestically in South Korea, Italy, Iran, and Japan from mid- February 2020 [22]. Especially in the republic of Korea, the unfold of COVID-19 had been properly managed until mid-February. The wide variety of validated instances in South Korea was 31 on February 18 [23]. However, COVID-19 infections among a spiritual group in the Daegu metropolitan place and a close-by hospital caused a surprising spread to other predominant domestic cities in South Korea in mid-February.
It became clear that the COVID-19 infection takes vicinity via publicity to the virus and both the immunosuppressed and regular population appear susceptible. Some studies have reported the age distribution of character sufferers between 25 and 89 years old. Most character victims have been between 35 and 55 years old [24] and there have been fewer diagnosed instances among formative years and infants [24,25].
On 10 July 2020, WHO updated the total number of new cases in the last 24 hours (Table 1), (Figures 1 and 2).
| Globally | 10357662 cases(163939) | 508055 deaths (4188) |
| Africa | 306794 cases (9504) | 6192 deaths (182) |
| America | 5218590 cases (81885) | 249318 deaths (2189) |
| Eastern Mediterranean | 1077426 cases (19371) | 24970 deaths (547) |
| Europe | 2728059 cases (27624) | 197874 deaths (615) |
| South-East Asia | 808906 cases (23975) | 22235 deaths (642) |
| Western Pacific | 217146 cases (1580) | 7453 deaths (13) |
Table 1: Total new cases as on 10 July.
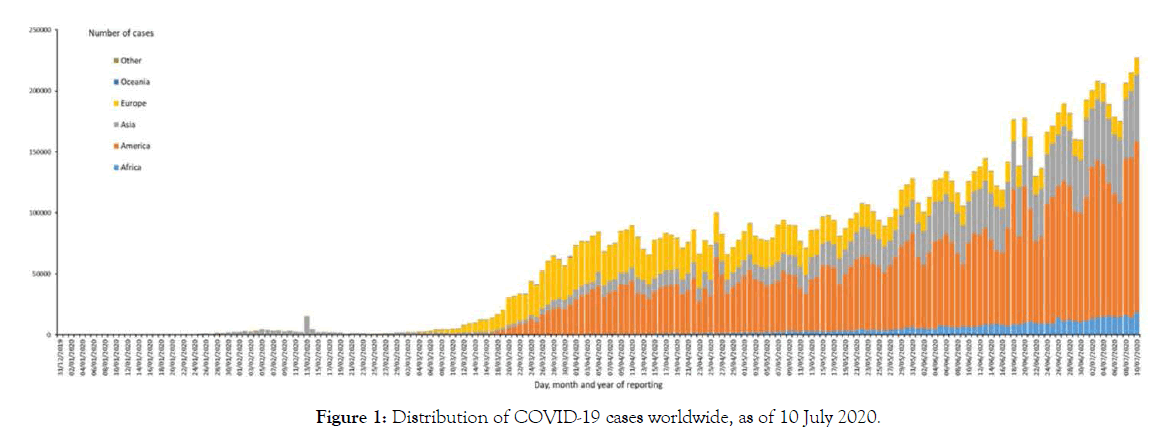
Figure 1. Distribution of COVID-19 cases worldwide, as of 10 July 2020.
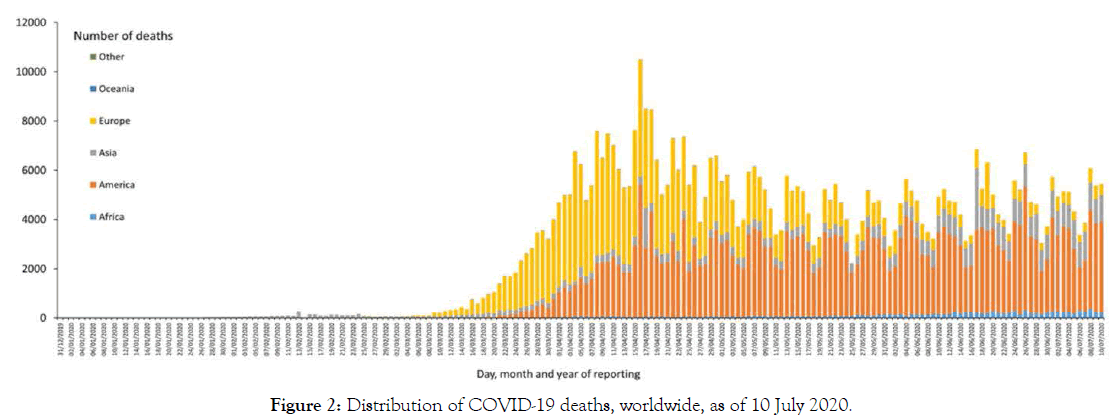
Figure 2. Distribution of COVID-19 deaths, worldwide, as of 10 July 2020.
Transmission
The novel corona virus originated from the Hunan seafood market at Wuhan, China, the place where animals are sold and hastily spread up to other countries worldwide. The virus that causes COVID-19 is a quite transmittable and pathogenic viral contamination and mainly transmitted through contact with respiratory droplets as an alternative than through the air [26,27]. The contamination to different nations spread mostly by means of ability of the friends to and from Wuhan metropolis at the time of peak infection. The South Korea, Italy and Iran has viewed most infected populace after the china [28]. The human to human unfold is now the essential way of transmission of the infection, the transmission may also be from symptomatic or asymptomatic person. The transmission happen from the symptomatic COVID-19 patient with the aid of the respiratory droplet when affected person coughs or sneezes. A single cough can flow up to 3 droplets. These droplets can land on other people, and overlaying surfaces around them, however, numerous smaller particles will remain inside the air. While in case of asymptomatic person [29] having the SARS-CoV-2 virus, the transmission from such patients appear with the aid of the handshake or illness of surfaces through fingers as such people do no longer exhibit signs COVID-19 [30]. The manual transmission may additionally spread in case of symptomatic patients. The virus is also shed for prolonged in faecal matter, accordingly every person who no longer washing their palms thoroughly after travelling the toilet could contaminate anything they contact like many respiratory viruses can be spread by way of shut contact with small droplets launched from contaminated individuals upper respiratory tract infections [31].
Impact of COVID-19 in pregnancy and on women’s reproductive health
Asymptomatic and mildly symptomatic pregnant ladies face two unique risks posed with the aid of SARS-CoV-2 contamination due to modifications in ACE2 expression to accommodate hemodynamic changes in pregnancy. The first risk entails the improved expression and exercise of ACE2 at some issue of being pregnant and conceivable secondary utero placental infection. According to the studies, ACE2 has been proven to metabolize Angiotensin-II to Angiotensin (1-7) [32]. Angiotensin–II constricts blood vessels while Angiotensin (1-7) dilates vessels. Relative expression of Ang II and Ang (1-7), closely influenced by ACE2 expression, was once proposed to maintain everyday blood pressure [33-36]. The uterus and the placenta, with their enhanced expression and exercise of ACE2 for the duration of pregnancy [37], may additionally put pregnant female at an expanded danger of organizing a utero placental SARS-CoV-2 infection. Recent researches have proven that no SARS-CoV-2 virus was detected in vaginal fluids or semen in infected persons [38,39]. COVID-19 infections may additionally have implications for infertility patients. The more desirable expression of ACE2 in the placenta and uterus in the course of early being pregnant after infertility remedy may make the organs more susceptible to viral entry in the course of mild or asymptomatic infections [40,41]. The local placenta-uterus contamination could result in inflammation and may compromise future fertility. ACE2 is also found in human ovarian follicles and the endometrium [42,43]. As a consequence, patients with moderate or asymptomatic SARS-CoV-2 infections can be additionally have hassle with their ovarian ovulation induction protocols or with implantation of embryos in the endometrium.
Maternal-fetal transmission of COVID-19
Maternal-fetal transmission of viral diseases (with the exception of herpes virus) is usually through the hematogenous route in which the virus circulating in the maternal blood stream enters the placenta, reaches the chorionic villous tree and fetal blood vessels, and is transmitted to the fetus. This mechanism of transmission has been shown not to occur with infection of pregnant women with two other pathogenic coronaviruses-SARS-CoV and MERS-CoValthough the clinical infections caused by these coronaviruses has resulted in severe maternal pneumonia, maternal deaths, and early pregnancy losses [44]. In recent studies among neonates delivered to these women who underwent testing, there were no cases of RT-PCR-confirmed SARS-CoV-2 infection, despite the existence of perinatal complications in some of the infants. An interesting observation is that in those cases where placentas were tested for SARS-CoV-2, the results were negative [45].
How can lactating mother avoid passing COVID-19 to the fetus?
While you are in the hospital or birth center and after you go home, Wash your hands before touching your baby. Wear a face mask or covering while breastfeeding or bottle feeding. Wash your hands before touching any breast pump or bottle parts and clean all pump and bottle parts after use [46,47].
Prevention of SARS-COV-2
In the absence of availability of entire remedy and emergency health care conditions, the prevention of SARS-CoV-2 is the prime consideration in controlling this ailment. Follow the directions of your regional fitness authority and stop secondary infections, interrupt human-to-human transmission to your shut contacts, fitness care personnel and forestall in a similar way worldwide spread. Also, people stay conscious of the trendy statistics on the COVID-19 outbreak provided through WHO. The preventive measures which must be taken are as follows-
• Wash your palms frequently and utterly with cleaning soap and water for at least 20 seconds or use alcohol based hand sanitizer that kills 99.9% of germs before and after caring for any sick person, after blowing one’s nose, or coughing or sneezing, after touching an animal, animal feed or animal waste and after touching garbage.
• Avoid touching the surfaces and contaminated hands as these may contain virus and avoid touching your nose, eyes or mouth without washing your hands otherwise viruses can be transferred to these organs.
• Maintain social (physical) distancing because when infected persons cough or sneezes, they spray small droplets from their nostrils or mouth which can also contain COVID-19 virus. The individual can breathe in these droplets [32,33]. By lowering the probability that a given uninfected individual will come into physical contact with an infected person, the disease transmission can be suppressed, ensuing in fewer deaths [34].
• A person who shows symptoms must keep him/herself in quarantine.
• Before scientific care is started, identify the plausible cases as quickly as feasible and isolate the suspected people separately from those who verified instances of the virus to prevent the workable transmission of infection to other sufferers and fitness care staff.
• If a person needs to consume meat or eggs, then thoroughly cooking meat, eggs and meals from animals would ruin the virus.
• Apply disinfectant daily on regularly touched surfaces such as keyboards, doorknobs, pens, tables, mild switches, handles etc. [33,35].
• The masks have been in massive demand in thinking closer to prevention of this viral infection transmission. The medical masks ought to be of assist in prevention of direct exposure to respiratory droplet from infected patients.
We are dwelling in times where a viral disease has added regular life in much of the world to a halt. The SARS-CoV-2 inflicting COVID-19 began in December 2019 in Wuhan, China. Recent research revealed that this disease is one of the most serious problem these days as the SARS-CoV-2 motives respiratory illness and it is spreading all across the world. There is an urgent need to understand the risks which might be and prepare families for current and future pregnancy challenges. Women are in fact advised to take the same precautions as the general public. Government agencies have quickly taken the initiatives to control this pandemic and also trying its best to diagnose and treat the COVID-19. We advise that the scholarly community conduct similarly look up to supply valid and reliable approaches to control this sort of disease.
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Citation: Wadood N, Toro AU, Madan A (2022) COVID-19 Impact on Pregnancy and Reproductive Health. J Women's Health Care. 11:599.
Received: 01-Aug-2022 Editor assigned: 04-Aug-2022 Reviewed: 18-Aug-2022 Revised: 25-Aug-2022 Published: 01-Sep-2022 , DOI: 10.35248/21670420.22.11.599
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.