Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Research Article - (2021)
Purpose: In the United States (US), after only one year, COVID-19 has already led to a reduction in life expectancy of about one year. In this study we review the mitigation and containment strategies of the epidemic in the US as a whole as well as in two of its largest states, namely New York (NY) and Florida (FL).
Methods: We utilized the Johns Hopkins University Coronavirus Resource Center to track the time courses of the epidemics in the US, NY, and FL.
Results: Today, the US represents about 5% of the world’s population but accounts for about 20% of deaths due to COVID-19. Initially, NY experienced the largest numbers of US deaths, but later enforced public health strategies of proven benefit and shutdown until deaths plummeted from the highest per capita to one of the lowest. FL issued no statewide mandates for social distancing, crowd avoidance, or masking. When cases plateaued, an initial shutdown was terminated prematurely, and restaurants and bars were mandated to reopen.
Conclusion: As competent and compassionate clinicians, teachers, and researchers in epidemiology and preventive medicine, we should encourage our patients and colleagues to practice the public health strategies of proven benefit. All US states, the nation as a whole, and all countries worldwide should employ coordinated public health strategies as an urgent and necessary adjunct to vaccinations.
Covid-19; Coronavirus; Food and Drug Administration (FDA)
CDC, US: Centers for Disease Control and Prevention; COVID-19: Coronavirus Disease 2019; EUA: Emergency Use Authorization; FDA, US: Food and Drug Administration; FL: Florida; NY: New York; US: United States.
In the United States (US) today, coronavirus disease 2019 (COVID-19) has surpassed cardiovascular disease and cancer as the single leading cause of death. In addition, after only one year, COVID-19 has already led to a reduction in overall life expectancy of about one year. In the US, the number of deaths from COVID-19 now exceeds 525 thousand and the number of cases now exceeds 29 million [1]. The deaths have already exceeded those from World Wars I (<120 thousand) and II (about 400 thousand) combined. In 2015, the US government had established a Global Health Security and Biodefense Unit. In early 2016, the World Health Organization surveyed the readiness of 195 countries. The world average was 40.2% and the US scored 83.5% thereby ranking number one in four of six categories including prevention, early detection and reporting, sufficient and robust health system, and compliance with international norms [2]. By 2018, the US government disbanded this unit [3]. At present, the country judged to have been best prepared for the existential threat turned out to be the least prepared for the actual threat [4-6]. Today, the US represents about 5% of the world’s population but accounts for about 20% of deaths due to COVID-19 [1,4-6]. As has been the case with most other major causes of death, racial inequalities are alarmingly large and are likely to only increase in the absence of an equitable distribution of vaccines [7]. Perhaps of even greater concern, the numbers of deaths that have occurred in the US are more than double that of any other country in the world [4]. In this study we review the mitigation and containment strategies of the epidemic in the US as a whole as well as in two of its largest states, namely New York (NY) and Florida (FL).
On January 19, 2020, the first case of coronavirus (COVID-19) was introduced into the US from Wuhan, China. The US government response was, “There will be no further cases,” and a month later after 15 cases had occurred, that “They will disappear.” Another month later, while COVID-19 was growing exponentially, the US government stated that “There would be no cases by April”. Initially, most cases were in major urban and metropolitan areas. Without mitigation or containment strategies of proven benefit, the exponential growth spread throughout the US. Even then, the US government response was delayed and fragmented with limited federal involvement. Each state had responsibility for its own containment and mitigation strategies despite the fact that the US was already experiencing the largest number of cases and deaths of any country in the world. Thus, the US government did not adopt the widely accepted public health strategies of proven benefit but, instead, adopted a strategy of “pandemic politics” [4-6].
Of greater concern, we believe the approach of the US government to COVID-19 included menacing assaults on science, the US Food and Drug Administration (FDA), as well as the US Centers for Disease Control and Prevention (CDC) [4]. For example, despite no reliable data from large scale randomized trials concerning COVID-19, the FDA issued an Emergency Use Authorization (EUA) for hydroxychloroquine. This EUA led to a nine-fold increase in US prescriptions. As a result, hydroxychloroquine was no longer available for many patients with autoimmune inflammatory diseases for which it had been approved about 46 years ago based primarily on a favorable benefit to risk ratio primarily among younger women [8,9]. Thus, it was unclear whether the stated “reassuring safety profile” for this drug based primarily on younger women would be generalizable to the elderly men at highest-risk developing and dying from COVID-19. Within several weeks, several largescale randomized trials were completed; all showed no benefit, and some demonstrated harm based on the previously well described prolongations of the QT interval [8]. Thus, the FDA withdrew the EUA but only after eroding their enormous and previously well-deserved public trust [10].
Before its politicization, the US CDC was a model for prevention and control efforts throughout the world [5,6]. During four US Presidencies, the CDC led and coordinated worldwide, national, and local efforts to eradicate smallpox, the, only human disease ever abolished from the face of the earth. The revival of the CDC is urgent [11,12]. For example, the CDC violated its own key principle to continue lockdowns until cases and deaths have almost disappeared [4-6]. On August 25, the CDC updated guidelines excluded exposed but asymptomatic individuals from testing. On September 17 it was revealed that White House officials had edited these guidelines without CDC approval. Further, a senior advisor to the Coronavirus Task Force, appointed by the previous US President, was a neuroradiologist. His credentials in epidemiology and preventive medicine were unclear but he, nonetheless, promulgated his theory widely, which was embraced by the former President, to rely on natural infection herd immunity alongside vaccine development to combat COVID-19. One logical consequence is that to achieve herd immunity, the US would have had to suffer between two and six million deaths depending on the timeline of the development and widespread distribution of effective and safe vaccines [4]. Further, after a September 26 White House super spreader event, 36 attendees tested positive, and the CDC was removed from its longstanding and experienced responsibilities for contact tracing [13]. In addition, until January 20, 2021 there was little evidence for any White House support for revised guidelines for masking that had been issued by CDC [14].
NY is the fourth most populous US state with 19.5 million residents, several major international airports, and a highly dense urban core. In the initial phase of the US epidemic, NY accounted for over 50% of all deaths (Figure 1). NY became the epicenter of the US and the US became and remains to this day the epicenter of the world. On March 2, 2020, the NY state government collaborated with local authorities to initiate and expand mitigation strategies. Specifically, mass gatherings were prohibited, schools were closed, and stay-at-home orders were enforced. In April, NY was the first state to issue and enforce a masking mandate and develop widespread testing and contact tracing programs. For three months, there were regular televised press briefings to provide informative and complete updates about cases, hospitalizations, and deaths. They emphasized urgency and necessity to practice mitigation strategies of proven benefit. These include masking, social distancing, crowd avoidance and frequent hand and face washing. NY followed guidelines first developed by the CDC. In NY, the lockdown continued until cases and deaths practically disappeared, which was long after the curve flattened. Deaths in NY plummeted from the highest rate per capita in the US to one of the lowest, where it has consistently remained (Figure 2) [1,4-6].
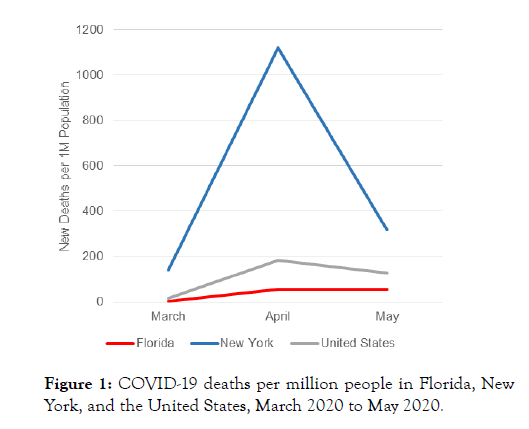
Figure 1: COVID-19 deaths per million people in Florida, New York, and the United States, March 2020 to May 2020.
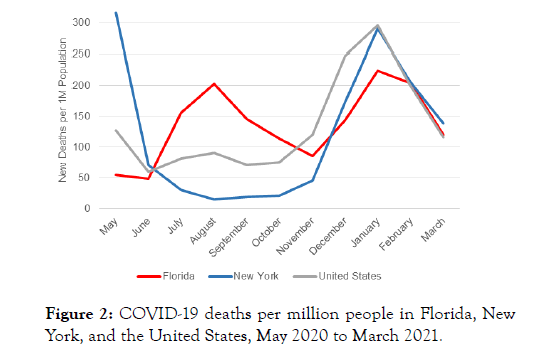
Figure 2: COVID-19 deaths per million people in Florida, New York, and the United States, May 2020 to March 2021.
FL is the third most populous state in the US with 21.5 million residents, several major international airports, and a lower population density than NY. Despite initial outbreaks in the southeast region of the state, the FL government issued no mandates. On March 16, 2020, a lockdown was mandated but then lifted prematurely on May 18 when the curve had only begun to flatten (Figure 1). On May 20, the FL governor proclaimed that “Florida had succeeded and was not the next New York”. When FL reopened, increases in new cases of COVID-19 were followed by more hospitalizations and then deaths. By August, deaths were rising in FL and falling in NY. On September 25, FL lifted all statewide restrictions, overruling local ordinances on masking, closures of bars, and limited opening of restaurants. Restaurants and bars were mandated to open immediately at >50% capacity and no fines or penalties would be collectable for pandemic-related mandates, including masking [4,15]. These strategies led to a several month-long spike in FL death rates which were higher than the US and NY averages (Figure 2).
“Death in old age is inevitable, but death before old age is not” [16]. Most deaths from COVID-19 are largely avoidable. Further, the hospitalizations that precede these premature deaths have threatened to paralyze the health care delivery system and the many premature deaths among many dedicated and conscientious healthcare workers trying to prevent them are particularly tragic [4].
Lessons can also be learned by comparing the mitigation and containment strategies of the US and South Korea. Both democratic republics with initial cases introduced on the same day. In contrast to the delayed and fragmented responses of the US, South Korea promptly and efficiently instituted nationally coordinated strategies of containment and mitigation [17]. By late February 2020, South Korea had the most cases of any country outside China, but today has 92 thousand total cases and 1600 deaths. Extrapolating these numbers with adjustment for the 6.5-fold difference in populations, the US would be expected to have about 598 thousand cases and 10,400 deaths. However, based on these considerations, the US has suffered almost 50 times the numbers of cases and deaths as South Korea. Such successes as seen in South Korea are widespread in Asia, and also include countries in Europe, South America, Australia, and Africa, all of which instituted prompt, coordinated, and effective containment and mitigation strategies. [1,4-6,17].
NY enacted late and initially fragmented responses but later employed effective public health strategies. The delayed but effective public health strategies of mitigation and containment reduced the death rate from COVID-19 in NY, but also caused large short-term economic consequences. FL enacted strategies more comparable to those of the US government. The FL approach assumed that deleterious economic consequences outweigh the increased risks of death, as also adopted by Brazil. Together, Brazil and the US account for >35% of deaths and <8% of the global population. Both countries’ Presidents contracted COVID-19. At present, both the US and Brazil have alarming increases in COVID-19 cases and deaths, far greater in the fall and early winter than they had last spring and summer [1].
Recently, the governors of Alabama, Iowa, Mississippi, Montana, and Texas have declared that state mandates would no longer be needed to prevent the spread of COVID-19 [18]. The situation in Texas is particularly alarming because, as of March 4, 2021, the rankings for total numbers of COVID-19 cases are California, followed by Texas and Florida, with NY falling to fourth. While herd immunity may occur within months, during that time it is most plausible that states rolling back masking mandates may have less of a decline or perhaps even increases as the seasonal fall in cases occurs. In addition, however, NY was not immune from “pandemic politics” either. The NY governor has been accused of obscuring a more accurate estimate of nursing home deaths, because the state’s count only included the number of deaths at the facilities, rather than accounting for the residents who died at a hospital after being transferred there. Thus, it appears that the total deaths from COVID-19 were accurate, but 3,800 had been attributable to hospital rather than nursing home deaths [19]. In FL, 9.5% of the population are >75 years, first in the US [20]. Among those >75 the COVID-19 death rate is 11.6% versus <1% among those <50 [21]. As of early March 2021, the rate of positive testing is about two-fold higher in FL (6.1%) than NY (3.1%) [1].
Each state in the US, the country as a whole, and all countries worldwide should continue to redouble efforts concerning coordinated clinical, medical and public health strategies while administering the vaccines as widely and efficiently as possible. We believe that all health professionals in the US and worldwide should unite concerning the urgency to practice as well as to preach these public health strategies.
Finally, any economic advantages of pandemic politics are shortlived and short-sighted in comparison to the public health strategies of proven benefit to avoid needless premature deaths from COVID-19. As competent and compassionate clinical and medical professionals, we should encourage our patients and colleagues to practice the public health strategies of proven benefit and promote evidence-based clinical and public health practices as well as discovery research, including basic, clinical and epidemiological.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Citation: Shih RD, Maki DG, Solano JJ, Levine RS, Alter SM (2021) Covid-19 in the United States: A Tale of One Country and Two Large States. Intern Med. S5:003.
Received: 02-Apr-2021 Accepted: 16-Apr-2021 Published: 23-Apr-2021 , DOI: 10.35248/2165-8048.21.s5.003
Copyright: © 2021 Maki DG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.