Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2019)Volume 9, Issue 1
Wells’ syndrome or eosinophilic cellulitis is a rare disease of which bullous form is uncommon, especially in children. We report a rare and original case of bullous Wells’ syndrome in a 10-year-old boy who was successfully treated with oral dapsone. It is therefore important to consider Wells’ syndrome in patients presenting recalcitrant bullous cutaneous eruption with eosinophilia.
Wells’ syndrome; Childhood; Bullous eruption; Eosinophilia; Dapsone
Wells’ Syndrome (WS) or Esinophilic Cellulitis (EC) is a rare disease histologically characterized by dermal eosinophilic infiltrate with flame figures. Bullous form of WS is uncommon and even more obscure in children. We report a rare and original case of bullous WS in a 10-yearold boy who was successfully treated with oral dapsone.
We report the case of a 10-year-old boy, with no history of recent vaccinations or insect bites or drug intake or atopic disease or any other personal or familial past medical history. He presented to our dermatology clinic with a recurrent pruritic and bullous cutaneous eruption, evolving for 4 years without fever and with good general statement. This skin condition was resistant to several topical and systemic treatments including antibiotics.
Clinical examination showed tense bullae of different size and a negative Nikolsky sign, based on well demarcated and slightly erythematous plaques, on both upper and lower legs and the trunk (Figure 1).
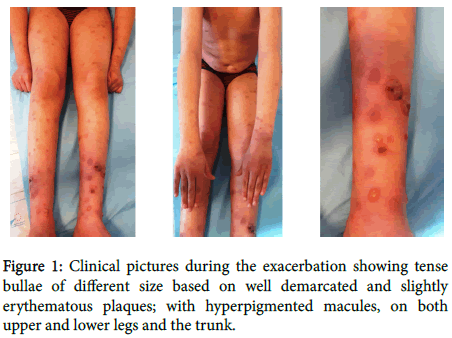
Figure 1. Clinical pictures during the exacerbation showing tense bullae of different size based on well demarcated and slightly erythematous plaques; with hyperpigmented macules, on both upper and lower legs and the trunk.
Mucous membranes were intact and the rest of general examination was normal. Laboratory tests objectived moderate leukocytosis (14000 cell/mm³) and marked eosinophilia (1300 cell/mm³) with elevated erythrocyte sedimentation rate (45 mm). Other biochemical and immunologic investigations were normal. Histological examination revealed acanthosis and dermal edema with diffuse infiltration made of eosinophils and some neutrophils. It also objectived flame figures made of eosinophilic debris deposited on collagen bundles, (Figure 2).
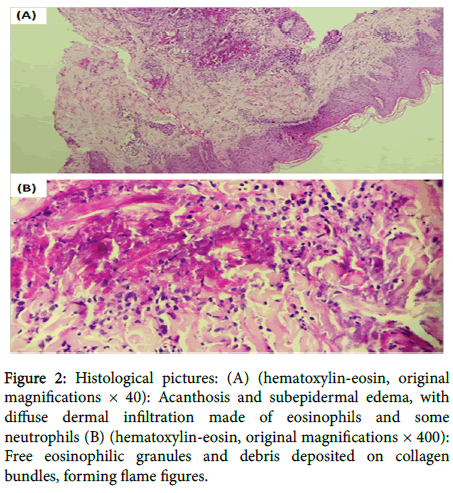
Figure 2. Histological pictures: (A) (hematoxylin-eosin, original magnifications × 40): Acanthosis and subepidermal edema, with diffuse dermal infiltration made of eosinophils and some neutrophils (B) (hematoxylin-eosin, original magnifications × 400): Free eosinophilic granules and debris deposited on collagen bundles, forming flame figures.
Perilesional direct immunofluorescence was negative. Based on clinical, biological and histopathological findings, a diagnosis of WS was made. Our patient was treated by oral dapsone (50 mg/day) for one month with rapid disappearance of the lesions and normalization of eosinophils rate (Figure 3).
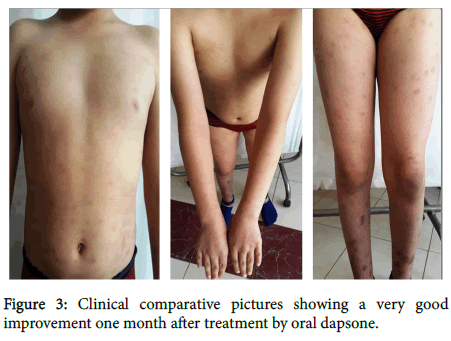
Figure 3. Clinical comparative pictures showing a very good improvement one month after treatment by oral dapsone.
George Wells described WS in 1971, the term ‘‘eosinophilic cellulitis’’ was then proposed in 1979 [1]. It is a rare recurrent inflammatory skin condition that more commonly occurs in adults. Pediatric cases are very rare with less than 30 pediatric cases in the literature [2]. The pathogenesis of this disease remains unclear. A local hypersensitivity reaction to different triggers like insect bites; drugs; vaccines; infections; hematologic disorders or solid tumors could be involved [3]. However, the inciting agent could be unknown in 50% of patients [4], as was the case in our patient.
WS may have different clinical presentations including plaque; urticaria; and annular, papulovesicular, bullous, and papulonodular lesions [2]. However, the bullous form of WS remains exceptional in children. Histopathological study shows dermal edema with an infiltrate of eosinophils without signs of vasculitis. Flame figures, which are not pathognomic for EC, represent the degranulation of eosinophils and deposition of their debris on collagen bundles. Otherwise, direct immunofluorescence is negative [4]. During exacerbation, laboratory tests may reveal peripheral eosinophila with elevated erythrocyte sedimentation rate and IgE level.
EC shouldn’t be confused with other bullous diseases including drug reaction, bacterial infection, idiopathic hypereosinophilic syndrome, bullous pemphigoid and others. Additional clinical, biological and histopathological data are important for differential diagnosis.
The affection can resolve spontaneously. For limited disease we can use topical corticosteroids. Systemic ones may be employed for extended forms. When the disease is recurrent and widespread, alternative treatments like dapsone; antimalarial agents; cyclosporine; azathioprine; interferon alpha; and photochemotherapy can be discussed [2,4,5].
Bullous WS is a rare condition even more obscure in children. It is therefore important to consider WS in patients presenting recalcitrant bullous cutaneous eruption with eosinophilia.
Citation: Salim S, Maouni S, El Meknassi I, Meziane M, Ismaili N, et al. (2019) Cutaneous Bullous Eruption Revealing Pediatr Ther 9: 355.
Received: 10-Mar-2019 Accepted: 11-Apr-2019 Published: 18-Apr-2019
Copyright: © 2019 Salim S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.