Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Short Communication - (2019)Volume 4, Issue 3
Introduction: Neonatal mortality is a public health problem in developing countries. Its reduction is an integral part of the goals for sustainable development.
Objectives: To determine the frequency of deaths during the first 48 hours at the Brazzaville University Hospital, to identify the causes of death and to determine the factors associated with early death.
Patients and methods: This was a descriptive and analytical study carried out in the neonatal department of the CHU Brazzaville from January 1 to June 30, 2018 (6 months). It concerned all neonates hospitalized during the study period and who died within 48 hours of hospitalization. The variables studied were epidemiological, clinical, paraclinical and progressive.
Results: 697 newborns were admitted to the service, 286 (41%) died, of which 133 (46.5%) in the first 48 hours of hospitalization. The average age at admission was 61.5 ± 132.5 hours. They were 64.4% male and 34.6% female. The causes of death were preterm birth in 52.6%, neonatal infection in 18.8%, perinatal asphyxia in 16.5% cases. Factors associated with death were male sex, baseline, vaginal delivery, respiratory distress, coma, prematurity, and low hemoglobin.
Conclusion: The early death of the newborn is common in Brazzaville. It is a reflection of the inadequacies of the health system. Its reduction requires an improvement of the technical platform of the services involved and the reinforcement of the capacities of the human resources.
Death; First 48 hours; Newborns
With 2.8 million deaths worldwide in 2016, neonatal mortality is a major public health problem [1]. Africa south of the Sahara and Southeast Asia are the most affected regions of the world [1]. The decline in neonatal mortality globally has been slower than that of under-five mortality [2]. Neonatal mortality accounts for 44% of deaths of children under 5 years of age [3]. In the Congo, the neonatal mortality rate is estimated at 21 per 1000 live births [1]. Most deaths occur in the first few hours after birth or hospitalization [4,5]. This early mortality is attributable to the conditions of care of newborns in the birth room, during a possible transfer and hospitalization. Reducing neonatal mortality to less than 12 per 1000 live births by 2030 is a target for sustainable development goals [3]. This requires that the causes and factors associated with the early death of the hospitalized newborn be mastered. The purpose of this study is to determine the frequency of deaths during the first 48 hours at the Brazzaville University Hospital, to identify the causes of death and to determine the factors associated with early deaths.
This was a descriptive and analytical study, which ran from January 1 to June 30, 2018 (6 months). It was conducted in the Neonatology Department of the University Hospital of Brazzaville. This service receives newborns in vital distress from the maternity hospital of the same hospital or other hospitals in the city. It has 20 incubators, 8 heating tables, a conventional phototherapy unit, a circuit of medical fluids, and ventilation assistance only by oxygen therapy to the telescope, electric vacuum cleaner slime.
The study involved neonates hospitalized in the department during the study period and who died within 48 hours of hospitalization. Newborns who died during transfer or admission were not included.
The variables studied were: the age, the sex, the socio-demographic characteristics of the mother, the monitoring of the pregnancy, the delivery way, the gestational age at delivery, the adaptation to birth, the anthropometric parameters at birth, the source, the transfer mode, the reason for admission, the clinical signs on admission, and the diagnosis.
The data capture and analysis were carried out successively by Excel and Epi Info 7 software. For the study of the factors associated with the occurrence of death, we compared the population of newborns who died in the first 48 hours. Hospitalization to other hospitalized newborns who died after the 48th hour or not. The ANOVA test, the chi-square test, and the Odds Ratio (OR) with a 95% confidence interval were used for univariate analysis to compare means and proportions. All variables that were found to be associated during the univariate analysis were selected for multivariate analysis. We performed a logistic regression to adjust the confounders. The materiality threshold is 5%.
During the study period, 697 newborns were admitted to the service, 286 (41%) died, of whom 133 (46.5%) were in the first 48 hours of hospitalization. The mean age at admission was 61.5 ± 132.5 hours (range: 1 hour and 28 days). They were 87 (64.4%) male and 46 (34.6%) female. The mean age of mothers was 26.1 ± 7 years (range: 15 and 42 years). Mothers were of low socioeconomic status in 79 (59.4%) cases. In 113 (85%) cases, the pregnancy was followed. The delivery was vaginal in 118 (88.7%) cases. Mean gestational age at birth was less than 31.8 weeks (range: 25 and 41 weeks). Premature babies accounted for 90 (67.7%). The mean birth weight was 2019 ± 950.3 g (range: 560 to 4050 g). Newborns with low birth weight accounted for 84 (63.2%). The mean birth size was 44.4 ± 5.2 cm (range: 32 and 53 cm). Mean cranial perimeter was 29.8 ± 3 cm (range: 22 and 35 cm). Newborns were admitted by reference from another health center in 82 (61.6%) cases, they came from the CHU maternity ward in 34 (25.6%) cases and from the home in 17 (12.8%). The transfer was unsafe in all cases (100%). The reason for admission was the prematurity in 56 (42.1%), the respiratory distress in 45 (33.8%), the apparent death status in 10 (7.5%), the jaundice in 7 (5.3%), the convulsion in 6 (4.5 %), and for another reason in 9 (6.8%). The clinical signs at admission are reported in Table 1. The C reactive protein was performed in 25 (18.8%) cases, it was high in 11 (44%). The hemogram performed in 47 (35.3%), anemia was noted in 26 (55.3%) cases. At admission, blood glucose was obtained in 36 (27.1%) of newborns, was normal in 18 (50%) cases, hyperglycemia in 10 (27.8%) and hypoglycemia in 8 (22.2%). The causes of death are reported in Figure 1. The mean time to death was 23.7 ± 14.9 hours (range 1 to 48 hours). Factors associated with the occurrence of newborn deaths are reported in Tables 2 and 3.
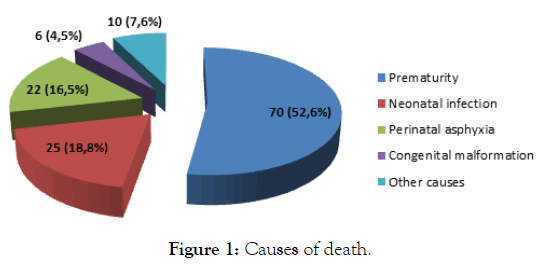
Figure 1: Causes of death.
| Parameters | N | % |
|---|---|---|
| Respiratory Distress | 127 | 96.2 |
| Hypotonia | 123 | 93.2 |
| Trouble of Conscience | 70 | 53 |
| Fever | 19 | 14.4 |
| Coma | 18 | 13.6 |
| Pale Skin | 18 | 13.6 |
| Jaundice | 17 | 12.8 |
| Convulsion | 14 | 10.6 |
Table 1: Cinical signs at admission.
| Parameters | Deces | 0R | IC (95%) | p | |
|---|---|---|---|---|---|
| Oui (%) | Non (%) | ||||
| Newborn Referred | 81 (69.8) | 234 (48.7) | 2.4 | 1.6 – 3.8 | 0.00006 |
| Male Sex | 87 (65.4) | 289 (51.4) | 1.8 | 1.2 – 2.6 | 0.005 |
| Low Socio-Economic Level | 79 (85) | 346 (78.1) | 1.6 | 0.9 – 2.9 | 0.2 |
| Multiple Pregnancy | 27 (20.5) | 105 (18.6) | 1.1 | 0.7 – 1.8 | 0.7 |
| Vaginal Delivery | 112 (88.7) | 423 (75) | 2.6 | 1.5 – 4.6 | 0.0009 |
| Resuscitation | 37 (27.8) | 138 (24.5) | 1.2 | 0.8 – 1.8 | 0.5 |
| Low Birth Weight | 84 (63.2) | 305 (54.1) | 1.4 | 0.9 – 2.1 | 0.07 |
| Respiratory Distress | 128 (96.2) | 344 (61) | 13.5 | 5.9 – 31.2 | 1E-07 |
| Pale Skin | 18 (13.5) | 29 (5.1) | 2.9 | 1.6 – 5.4 | 0.001 |
| Convulsion | 14 (10.5) | 59 (10.5) | 1 | 0.5 – 1.9 | 1 |
| Coma | 18 (13.5) | 13 (2.3) | 6.6 | 3.2 – 14 | 0.000001 |
| Jaundice | 17 (12.8) | 51 (9) | 1.5 | 0.8 – 2.6 | 0.3 |
| Prematurity | 90 (67.7) | 304 (53.9) | 1.8 | 1.2 – 2.7 | 0.005 |
| Hemoglobin | 13.7 ± 3.6 g/dl | 15.1 ± 3 g/dl | - | - | 0.005 |
| Blood Glucose | 1.2 ± 1.2 g/l | 1 ± 0.8 g/l | - | - | 0.2 |
Table 2: Univariate analysis.
| Parameters | ORa | IC (95%) | Coeff | S.E | Z-Statistic | p |
|---|---|---|---|---|---|---|
| Male Sex | 1.7 | 1.1 – 2.7 | 0.5 | 0.2 | 2.2 | 0.03 |
| Newborn Referred | 1.7 | 1 – 2.7 | 0.5 | 0.3 | 2 | 0.04 |
| Vaginal Delivery | 2 | 1 – 3.7 | 0.7 | 0.3 | 2 | 0.04 |
| Coma | 4.4 | 1.9 – 10.3 | 1.5 | 0.4 | 3.5 | 0.0005 |
| Respiratory Distress | 44.9 | 6.2 – 326.1 | 3.8 | 1 | 3.8 | 0.0002 |
| Prematurity | 2.3 | 1.4 – 3.8 | 0.8 | 0.3 | 3.2 | 0.002 |
Table 3: Multivariate Analysis.
The early death of the newborn is a reflection of the quality of the obstetric care, its care in the birth room, during a possible transfer and in the unit of hospitalization. We reported 46.5% of newborn deaths in the first 48 hours of hospitalization. Fla Koueta in Ouagadougou and Kedy Koum in Douala had a respective frequency of 58.8% and 7.7% of deaths during the first day of hospitalization [4,6]. With a population of low-birth-weight newborns, Ouedraogo report 50.8% of deaths occurring in the first 48 hours, a result similar to Yugbare [7].
Prematurity, neonatal infection and perinatal asphyxia were the main causes of early death at the Brazzaville University Hospital. These pathologies are the major causes of mortality in the neonatal period, they are observed in order of variable frequency by various authors at the world level and in the Neonatology units in Africa south of the Sahara [1, 4, 5, 8-10].
The reference of the newborn from a peripheral health center to the Brazzaville University Hospital is associated with the early death of the newborn. In developing countries and particularly those in sub-Saharan Africa, the transfer of newborns from a health center to the most equipped one is most often carried out in public transport vehicles, in the absence of medical personnel, without prevention of hypothermia and hypoglycemia [11,12]. We believe that the non-optimal conditions in our practice would favor early infant mortality. Fresson in France, a country better equipped than ours, report a significant mortality of newborns "outborn" in comparison with "inborn" [13].
The male sex in our study is significantly related to death. This observation is similar to the results of Katamea in the DRC and Hoan in Vietnam [12,14].
The vaginal delivery is also identified as a factor of death of the newborn. This same finding is observed by Ouedraogo [7]. This pathway poses a greater risk of dystocia, a source of intrauterine hypoxia and asphyxia at birth and therefore of death [6]. Other factors associated with death, severity of clinical condition at admission, including coma and respiratory distress, and prematurity. Mbarambara et al. [15] in the DRC and Kedy Koum et al. [9] in Cameroon also report the association of prematurity with neonatal mortality. The breeding of premature babies is difficult in our countries because of the under-equipment of our health structures and particularly of Neonatology services [12].
Early death is a major concern in the neonatology department of the Brazzaville University Hospital. The causes are dominated by perinatal pathology. The factors associated with death, which are essentially related to the quality of care, lead us to propose as measures to reduce it, the improvement of the care of the pregnant and the newborn, and the equipment of the unit of neonatology.
None.
Citation: Ekouya Bowassa G, Ngakengni NY, Moyen E, Okoko AR, Mbika Cardorelle A, Moyen G (2019) Death during first 48 hours in the Department of Neonatology of the University Hospital of Brazzaville. Clin Pediatr OA 4:157.
Received: 02-Aug-2019 Accepted: 22-Aug-2019 Published: 29-Aug-2019
Copyright: Copyright: © 2019 Ekouya Bowassa G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.