Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2022)Volume 7, Issue 3
Background: Delay in diagnosis of congenital heart disease (CHD) causes significant morbidity and mortality. However, screening of neonates at birth enables early identification of CHD and decreases complications related to delay diagnosis. Research that investigates the magnitude of delay diagnosis of congenital heart disease was enable stakeholders to plan a targeted awareness-creation on screening practices for early detection of congenital heart disease.
Objectives: To assess delay in diagnosis of congenital heart disease and associated factors among pediatrics patients who were registered in Cardiac Center Ethiopia from January 1, 2018, to December 30, 2020.
Methods: A retrospective institutional-based cross-sectional study design was used in the cardiac center in Addis Ababa, Ethiopia. A total of two hundred sixteen registered pediatrics congenital heart disease patients who fulfilled the inclusion criteria were included in this study. The data was entered into Epi-data version 7.2.2.6, cleaned, and exported to SPSS version 24 for analysis. Variable having a p-value<0.25 was a candidate for multivariable analysis. Then multivariable analysis was performed to determine the associated of independent factors of the dependent variable. Statistical significance was considered at p-values<0.05 and Adjusted Odds Ratio (AOR) at 95% confidence interval (95% CI).
Results: In this study 216 children were included, of total study subjects, 83 (38.4%) were male and 133(61.6%) were female, 85 (39.4%) of children were aged from 12 month to 5 year of age. Delayed diagnosis of CHD was noticed in 206 (95.4%) children. In multivariable logistic regression analysis, Maternal education those who had illiterate [AOR=0.135 (95% CI=(0.025-0.715)]. Place of child delivery, Hospital [AOR=0.057 (95% CI=(0.005-0.643)] and gestational age in weeks during delivery preterm baby [AOR=0.110 (95% CI (0.017-0.723)] are significant factors.
Conclusion: Maternal education, place of child delivery and gestational age were independently associated with the delay diagnosis of congenital heart disease. Repeated history of respiratory tract infection was also seen as complication. Improving the basic socioeconomic indicators and establishing a proper screening and referral healthcare delivery system are helpful.
Delay diagnosis; Congenital heart disease; Pediatrics
Congenital heart disease (CHD) is the most common congenital malformation worldwide. One in every 100 babies is born with CHD, with 1 in every 4 births having critical CHD. About 50,000 infants are born with it, and 12,500 are born with critical CHD. Although the fact that children with CHD have a better chance of survival congenital disorders remain a major health concern around the world [1].
In Indonesia, 5 million infants are born every year [2].The incidence of moderate and severe forms of congenital heart disease is approximately 6/1,000 live births or 19/1,000 live births if the possibly severe bicuspid aortic valve is included. A study that includes small muscular VSDs at birth and other small lesions in the western US indicates that the incidence of CHD reach 75/1,000 live births annually [3]. Another study in Ethiopia reported the diagnosis of CHD as 35.8% [4].
Congenital heart disease is the leading cause of birth defects and the second leading cause of death in the first year of life, after infectious diseases [5]. There are eight common CHDs, and these are VSD (Ventricular Septal Defect), Atrial Septal Defect (ASD), Patent Ductus Arteriosus (PDA), Coarctation of Aorta (CoA), Tetralogy of Fallot (TOF), Transposition of Great Arteries (TGA), Pulmonary Stenosis (PS), and Aortic Stenosis (AS) [6].
Delay in diagnosis of CHD causes significant morbidity and mortality [7]. It is associated with cardiovascular compromise and organ dysfunction, leading to prolonged ventilation and mortality among neonates undergoing cardiac surgery [8]. Delay in diagnosis of cyanotic CHD occurs when children with CHD are diagnosed after being sent home from the birth clinic or hospital [9,10]. Regarding a cyanotic CHD, delay diagnosis is when the children are diagnosed during cardiac surgery or intervention that should have already been performed.
Proper diagnosis of CHD is when the patient does not need emergency management at the onset of diagnosis, when treatment does not carry a high risk, when there is no need for different management, or when the patient has a good outcome if treated earlier [10]. On the other hand, advancing technology has improved the outcomes of children with these defects in developed countries. However, the financial impact of a child with CHD has exponentially increased over the last few decades. As such, in sub- Saharan Africa, the cost burden is significant and carries important implications for treating children with CHD [6].
Statement of the problem
Delay in diagnosis of congenital heart disease is prevalent globally in high, middle and low income countries. A study in high-income country shown that the proportion of delay diagnosis is 9% it including delay in diagnosis of cyanotic CHD of 10.4% and a cyanotic CHD of 8.7%.The critical CHD is also 29.5% of delayed in diagnosis of CHD [11].
Such delay in diagnosis causes major morbidity and mortality [7]. A recent study found that of the total pediatric hospitalizations in the US, only 3.6% accounted for treating children with CHD. However, it represented more than 15% of the annual costs for pediatric hospitalizations [12]. A Florida study showed that delayed detection of congenital heart disease increased hospitalization by 52% more admissions, hospitalized days 18%and infancy hospitalization costs by 35% [13]. Similarly, a study conducted in low- and middle-income countries showed a delay in diagnosis of congenital heart disease of 85.1% [14]. About 11.7% of the study cases died within 12 months of birth. Of these, 75.7% were diagnosed prenatally, 20.6% were diagnosed in the hospital, and 3.7% had delayed diagnosis [15].
Various factors contributing to the delay in the diagnosis of CHD reported in prior studies include inadequately trained health care providers in the health system and socioeconomic constraints in low and middle income country settings [14]. Congenital deficiencies associated with monogenic and chromosomal abnormalities, environmental teratogenicity substances, multifactorial inheritance, and micronutrient deficiency [16,17]. Additionally due to the high fertility rate and high neonatal mortality rate, the incidence of CHD in sub-Saharan Africa is greatly underestimated [18].
As far as I studied, there is no study conducted that aims to assess the magnitude of delay in diagnosis of congenital heart disease and associated factors among pediatric patients in the cardiac Centre in Ethiopia. Therefore, the aim of this study is to identify the magnitude of the delay in diagnosis of congenital heart defects and associated factors by doing a retrospective chart review on patients registered in the Cardiac Centre in Addis Ababa, Ethiopia by conducting a telephone interview with the caretaker of the patient.
Significance of the study
This study will add to existing research reports on CHD and fill a knowledge gap on delay in diagnosis and associated factors among pediatric cardiac patients in developing countries, specifically Ethiopia. Moreover, the findings of this study will be used as a reference for health care providers working on maternal and child health services, researchers, and policymakers to recognize the scope of the problem. Following that, assist policymakers in developing appropriate interventions and strategies for maximizing long-term benefits on quality of life.
In particular, the findings of this study help health care providers and managers target the development of appropriate strategies that are targeted to address the identified contributors to the delay in diagnosis of CHD and enhance health care professional knowledge and skills in the early identification of CHD. Subsequently, it may contribute to early diagnosis and ensure prompt medical response that can reduce complications, hospital stays, healthcare costs and lead to improved chances of survival by preventing death from these conditions. Furthermore, it serves as a reference for future clinical and public health research.
Delay in diagnosis of congenital heart disease
A delay in diagnosis of cyanotic CHD is defined as new-born with CHD at birth being discharged from health care facilities without a diagnosis of existing heart disease. For a cyanotic CHD, delay diagnosis is defined as first diagnosis of the defect at a time based on recommended standards [19]. A study in India showed that treatment should already have taken place or if at the time of diagnosis immediate therapeutic action was required. Study had shown in Eastern Europe 8.9% [10], southern Asia 85.1% and another study showed in Kenya were found by 60.6% of the children to have delay in diagnosis of CHD [20].
A study which was conducted in Pakistan showed that 58.9% of male and 40.1% of female patient have delay in diagnosis of CHD. Majority of the children, 69.4% were<2 years of age and 61.9% children their body weight was below the 3rdcentile. Regarding socio-demographic characteristic 63.4% children live in rural areas of residence and their Socio-economic status was low in 54.3%, middle in 37% and high in remaining 8.7%. A 43% of mother was illiterate among cases. Maternal fetal echocardiography was done in 4.9%. A cyanotic CHD was distinguished in 67.9% children while remaining had cyanotic CHD 32.1% [21].
In another study shown were male 63.3% and female 36.7%. Median age was 24 months. The patients had a median weight of 13 kg with majority of the patients weighing below the 3rdcentile for age 56.8%. Approximately 60% children came from rural areas. About 66% belonged to poor socio economic class with additional 30% from middle income group. Illiteracy rate in parents was mothers 54%.Only 2% of mothers had a fetal echocardiography performed. Most babies were delivered at home or local maternity centers 77%. Median distance the patient had to travel to reach the cardiac center was 32% traveling more than 100 km. About 65.3% children had a cyanotic CHD [14].Comorbid complications in delayed diagnosis of Congenital Heart Disease were prevalent [22].
Associated factors of delay in diagnosis of congenital heart disease
Findings that shown in Southern Asia reported most patients had delay in diagnosis of CHD due to the delayed diagnosis by health care providers 22.5%, delayed referral/follow-up 13.3%, social factors 13%, financial restrictions 12.3%, and religious beliefs 1.7% [14]. In other study shown in Southeast Asia diagnosis of CHD in most patients was delayed because of delayed diagnosis by doctor 57.5%, delays related to midwifery care 14.4%, financial factors 9.7%, delays in referral and follow-up 9.2%, and social factors 9.2% [22]. Most common factor contributing to found in delayed first consultation in 40.3% and by the doctor was the second most frequent to delayed diagnosis of CHD was 24.6% children [21].
Also in another study shared from Indonesia on delayed diagnosis of CHD by doctors was noted to be the associated factors for delayed diagnosis of CHD in children among 57.5% cases [22]. Inadequate trained health system, lack of awareness and financial issues contributing to delay in diagnosis of CHD. Its diagnosis among health care provider could be one important reason behind missed diagnosis of CHD [14].Studies have shown that delay in diagnosis of CHD is linked with severe complications and many times, complications have already occurred when the delay diagnosis is made [22,23].
The most common lesions found were PDA 29.2%, VSD 28%, ASD 17.7% and TOF 10.4%. Additionally, the most common clinical presentations being recurrent pneumonia 77.4%, murmur 76.6%, failure to thrive 24.1% and cyanosis 17% as study conducted in Kenya [20]. Advanced antenatal screening programs such as fetal echocardiography screening are well-established in high-income countries [24]. In Indonesia study shown primary healthcare settings, lack of awareness about CHD by general practitioners might explain these delays. The clinical features of children with CHD are various, thus the diagnosis is challenging. These clinical signs including cough, dyspnea, and failure to thrive, can be misinterpreted as symptoms of other diseases, and managed until the alternate diagnosis of CHD are established. Tuberculosis is one of the diseases reported in misdiagnoses of CHD in children due to their similar symptoms like failure to thrive, and their frequent incidence in Indonesia. These misdiagnoses lead to a lack of followup treatment since the physician’s advice to give more feeding will not resolve the main problem [22].
As Journal of the American Society of Echocardiography shown on Antenatal fetal echocardiography is considered to be a very supportive tool for the identification of CHD at earlier stages and can be useful in minimizing the morbidity and mortality related with CHD [25]. Antenatal diagnosis of CHD is quite common in developed country study conduct in London [7]. However recent data shown that Antenatal fetal echocardiography is not routinely use for early identification of CHD in south Asia [14].
Theoretically, clinical findings in cyanotic CHD should be more obvious than a cyanotic CHD because of the bluish discoloration of children with cyanotic CHD due to the right-to-left shunt, which results from deoxygenated blood entering the circulation [26].
Study shown in high-income countries reported the decline in delay referrals of cyanotic CHD patients is attributable to national neonatal Pulse Oximetry Screening (POS) recommendations [27]. Neonatal POS is a critical factor for screening of CHD in every newborn. Assessment timing ranges at less than 24 hours to 48 hours of age. Newborns should be referred for cardiology evaluation if oxygen saturation consistently falls below 95% [28]. Conceptual framework: (Figure 1).
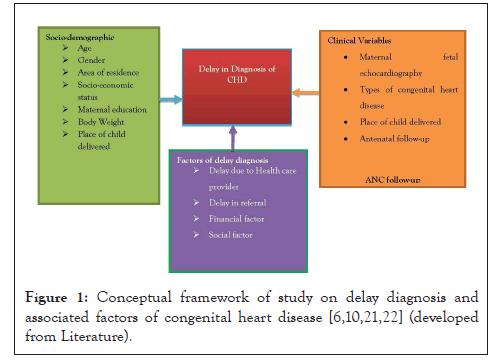
Figure 1: Conceptual framework of study on delay diagnosis and associated factors of congenital heart disease [6,10,21,22].
Objectives
General objective: To assess delay in diagnosis of congenital heart disease and associated factors among Pediatrics patients who were registered in Cardiac Center Ethiopia from January 1, 2018, to December 30, 2020.
Specific objective: It includes,
• To identify the delay in diagnosis of congenital heart disease among pediatric patients who were registered in Cardiac Center Ethiopia from January 1, 2018, to December 30, 2020.
• To determine associated factors for delay in diagnosis of congenital heart disease among pediatric patients who were registered in Cardiac Center Ethiopia from January 1, 2018, to December 30, 2020.
Study setting/area
The study was conducted at Cardiac Center, Ethiopia (Children’s Heart Fund of Ethiopia), located in Addis Ababa, which is the capital city of Ethiopia, established in 1992 inside Zewditu Memorial Hospital, Cardiac Center, Ethiopia, and is now located inside Black Lion specialized hospital in Addis Ababa. The idea of this cardiac center was conceived 30 years ago by Dr. Belay Abegaz but started functioning in 2009. It is a tertiary referral cardiac center for patients requiring cardiac intervention from all parts of the country. There are one hundred seventy-two (172) staffs including supportive staff. It has a total of 13 heart team members that include six cardiologists, two cardiac surgeons, two cardiac anesthesiologists, one cardiac intensivist, and two per fusionist and trained nurses. Since the first date of its operation, it has provided services for about 10,000 patients free of charge, of which 5600 of them are Pediatrics. Cardiac catheterization, implanting peacemaker, coronary bypass surgery, coronary angiography, Electrocardiography (ECG), and Echocardiograph are some of the services given by the center. It also has facilities such as Outpatient Department (OPD), Cardiac Care Unit (CCU), Odds Ratio (OR) and Cardiac Catheterizations Laboratory (Cath Lab) are the clinical departments. It has 30 beds and gives 24-hour services for both children and adults. It receives 150 new patients per month on average. These patients have follow-up depending on their condition at least once per month. Besides, patients can visit the clinic when he/she needs care [29].
Study period: Study was conducted from September 2021 to January 2022 G.C
Study design: Retrospective institutional based cross-sectional study design was used to assess delay in diagnosis and associated factors among pediatrics congenital heart disease patients at Cardiac Center Ethiopia.
Study population: All congenital heart disease who attends pediatrics cardiac clinic of cardiac center Ethiopia.
Source population: All registered of pediatrics with congenital heart disease patients in Cardiac Center Ethiopia during study period.
Eligibility criteria
Inclusion criteria: All children who diagnosis as confirmed CHD by Echocardiography in the study hospital.
Exclusion criteria: It includes,
• Those who diagnosis by Echocardiography has no congenital heart disease and age of >18 years old.
• Records with incomplete data
• Home delivery
Sample size: The sample sizes in this study were determined using a single population proportion formula.
Where n=the required sample size
Z=standard score corresponding to 95% confidence interval 1.96
P=the estimated proportion will take One study in a low- and middle-income country demonstrated in Pakistan found 85.1% or 0.85 of thecCHD [14].
d=the margin of error (precision) 5%
d-Is the desired degree of accuracy (taken as 0.05)
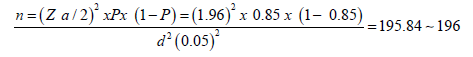
Therefore, n=196
Since the data collection will based on the medical record Number and interviewer administered method, 10% non- response rate sample size will increase to 216.
Sampling technique: Systematic random Sampling technique was used to select CHD pediatrics patient. Sampling interval (kth) will determine by dividing the total number of CHD patients that came within the study period (three Years) by the allocated sample size.
Total no of patients within 3 Years=1426 Sample size=216
K=1426/216=6.6 ⁓ 7
The first patient was select randomly then every 7th patient will select from the patient registration list until the required sample will be reached .Then, using the medical record number of select of the patients’ cards will be retrieved from the card room.
Measurement
Study variables
Dependent variable: Delay in diagnosis of CHD
Independent variables
Socio-demographic status: It includes,
• Age
• Gender
• Area of residence
• Socio-economic status
• Maternal education
• Body weight
Clinical variables: It includes,
• Maternal fetal echocardiography
• Types of congenital heart disease
• Place of child delivered
• Antenatal follow-up
Instruments: The data was collected by using clinical card review check list and telephone interview guide which is developed from different literature on related topic by adjusting the tools of previous studies and revising the literature of similar studies. The check list includes socio-demographic, types of congenital heart disease, Complications at the onset of diagnosis among pediatrics with CHD. And the telephone interview includes factors for delay in diagnosis of congenital heart disease.
Data collection and procedures
The data was collect by using patients’ card review checklist and through telephone interviewing of patient’s families retrospectively about associated factors related to delay in diagnosis of CHD. For this study three BSc nurses for data collection and one senior MSc nurse super visor were recruited during data collection. The data collectors and supervisors were trained for 3 days about objectives of the study and the data collection tools.
Operational definition and definition of terms
Congenital heart disease: a defect in the structure or function of the heart and great vessels which is present at birth diagnosed by echocardiography.
Delay in diagnosis: It is newborns discharged from their birth clinic or hospital without a CHD diagnosis with in timing ranges at less than 24-48 hours of age.
Delay diagnosis due to health care provider: Ever suspected of CHD by the health care providers after discharge a child from health facility.
Delay due to referral: Is the time from the doctor (general practitioner, pediatrician) to definite diagnosis, or suspected of CHD to refer be to tertiary health care.
Delay related to social factors: Any personal, cultural, and spiritual beliefs that influenced the delayed diagnosis.
Delay related to financial factor: Economic factors that influence delayed diagnosis or treatment of CHD after seeking medical attention [14].
Pediatrics: Age range is defined as ages 0-18 (birth to 18 years of age) [30].
Incomplete data: If there is not available echocardiography result and at least 2 phone numbers in patients’ card.
Data quality control and management: To assure the quality of data, the data collection instrument was developed in the English version by using from different literatures. The data collection format was pretest on 5% of the sample size to check for uniformity and understandability of the checklist in Black Lion Specialized Hospital before the actual data collection. During the data collection procedures, all the collected data was revised and checked daily for its completeness, accuracy and clarity by the supervisor and principal investigator.
Data analysis plan and procedure: The data was compiled, entered, into Epic-data version 7.2.2.6, and then cleaned, explored, standardized, and exported to SPSS windows version 24 for summarization and further analysis. Bi variable analysis was carried out to assess the association between the dependent and all the independent variables and to identify the candidate for multivariate analysis. Variable having a p-value<0.25 was a candidate for multivariable analysis. Then multivariable analysis was performed to determine the associated of independent factors of the dependent variable. Statistical significance was considered at p-values<0.05 and Adjusted Odds Ratio (AOR) at 95% confidence interval (95% CI). The result will present using OR and adjusted OR. Finally, the result was presented in tables, graphs, and statements.
Ethical consideration: Ethical approval letter was obtained from St. Paul’s Hospital Millennium Medical College Institution Review Board (IRB). Then official letter was written to Cardiac Center Ethiopia and Consent was obtained from all the study participants after they briefly informed about the objectives and the aim of the study before taken phone interview. Confidentiality was maintained at all levels of the study by not writing the respondent’s name on the checklist and the information which was gotten from the respondents were not be shared for other persons and was used only for the purpose of the study. Ethical issue dealing with respondents, techniques of supervision and how to handle data collection instrument were discussed.
Dissemination of the result: The result of the study will be submitted to St. Paul’s Hospital Millennium Medical College department of medical surgical nursing. If a need arises the result will presented for those who want the results of the study for intervention.
Demographic characteristics of patients
In this study, 216 children were included of total study subjects, 83 (38.4%) were male and 133(61.6%) were female, 85 (39.4%) of children were aged from 12 month to 5 year of age. There were 175 (81%) children who belonged to rural areas of residence. Maternal education status as illiterate was seen among 54 (25%) and literate were 162 (75.0%) cases. Socio-economic status was low (monthly family income below or<4000 ETB) in 144 (66.7%), middle (monthly family income between 4000 to 7000 ETB) in 60 (27.8%) and high (monthly family income above >7000 ETB) in remaining 12 (5.6%) [31] (Table 1).
| Characteristics | Frequency | (100)% | |
|---|---|---|---|
| Age | 0-1 month | 1 | 0.5% |
| 1-12 month | 43 | 19.9% | |
| 12month-5 year | 85 | 39.4% | |
| 5-10 year | 54 | 25.0% | |
| 10-18 year | 33 | 15.3% | |
| Gender | Male | 83 | 38.4% |
| Female | 133 | 61.6% | |
| Area of residence | Urban | 41 | 19.0% |
| Rural | 175 | 81.0% | |
| Maternal education | Illiterate | 54 | 25.0% |
| Literate | 162 | 75.0% | |
| Socio-economic status | Low<4000 | 144 | 66.7% |
| Middle 4001-7000 | 60 | 27.8% | |
| High>7000 | 12 | 5.6% | |
Table 1: Socio demographic characteristics of delay in diagnosis of Congenital heart disease patients attending at cardiac center Ethiopia, Addis Ababa, Ethiopia, January 1, 2018, to December 30, 2020 (n=216).
Clinical variables of patients
Maternal fetal echocardiography was done in 2 (0.9%). A cyanotic CHD was noted in 205 (94.9%) children while remaining had cyanotic CHD 11 (5.1%). Delayed diagnosis of CHD was noticed in 206 (95.4%) children. Body weight below 3rd centile was seen in 127/43 (33.8%) of under 5 years Children. During ANC follow-up maternal fetal echocardiography for about 2 (0.9%) were done for the mother of children (Table 2).
| Characteristics | Frequency | (100)% | |
|---|---|---|---|
| Place of child delivery | Hospital | 86 | 39.8% |
| Health center | 130 | 60.2% | |
| Body weight of child during diagnosis | <16 Kg | 123 | 56.9% |
| >/=16 Kg | 93 | 43.1% | |
| Maternal Fetal Echocardiography | Yes | 2 | 0.9% |
| No | 214 | 99.1% | |
| Delay in diagnosis | Yes | 206 | 95.4% |
| No | 10 | 4.6% | |
| Diabetes mellitus diagnosis before or during pregnancy | Yes | 4 | 1.9% |
| No | 212 | 98.1% | |
| History of maternal Hypertension | Yes | 34 | 15.7% |
| No | 182 | 84.3% | |
| First prenatal care visit | First trimester | 49 | 22.7% |
| Second trimester | 117 | 54.2% | |
| Third trimester | 41 | 19.0% | |
| Unknown | 9 | 4.2% | |
| Family history of Congenital Heart Disease | Yes | 20 | 9.3% |
| No | 196 | 90.7% | |
| Plurality | Singleton | 210 | 97.2% |
| Twins or Above | 6 | 2.8% | |
| Gestational age in weeks | 32-36 (Preterm) | 13 | 6.0% |
| 37-42 (Term) | 203 | 94.0% | |
| Types of Congenital Heart Disease | Acyanotic CHD | 205 | 94.9% |
| Cyanotic CHD | 11 | 5.1% | |
Table 2: Clinical variables related to delay in diagnosis of Congenital heart disease patients attending at cardiac center Ethiopia, Addis Ababa, Ethiopia, January 1, 2018, to December 30, 2020 (n=216).
Among 206 children with delayed diagnosis of CHD, possible factors for delayed diagnosis were recorded. Most common factor contributing to delayed diagnosis of CHD was found to be delayed due to Health care provider in 193(89.4%). Delayed in referral was the second most frequent factor contributing to delayed diagnosis of CHD about 13 (6%) children. Delayed in financial were observed in 5 (2.3%) children (Figure 2).
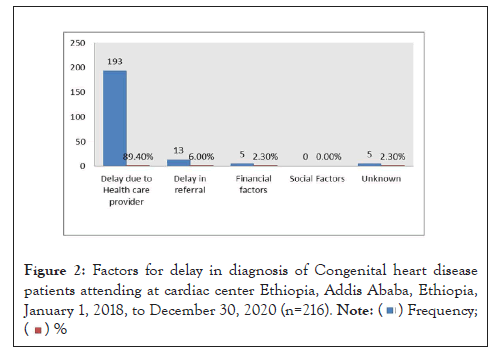
Figure 2: Factors for delay in diagnosis of Congenital heart disease
patients attending at cardiac center Ethiopia, Addis Ababa, Ethiopia,
January 1, 2018, to December 30, 2020 (n=216).
 .
.
The common complications at the onset of diagnosis among children with delay in diagnosis of congenital heart disease patients attending at cardiac center Ethiopia are congestive heart failure, pulmonary hypertension, heart rhythm problem, repeated attach of Respiratory Tract Infection (RTI) and failure to thrive. About 88(41%) of children were repeated attach of respiratory tract infection is a major complication during this study (Figure 3).
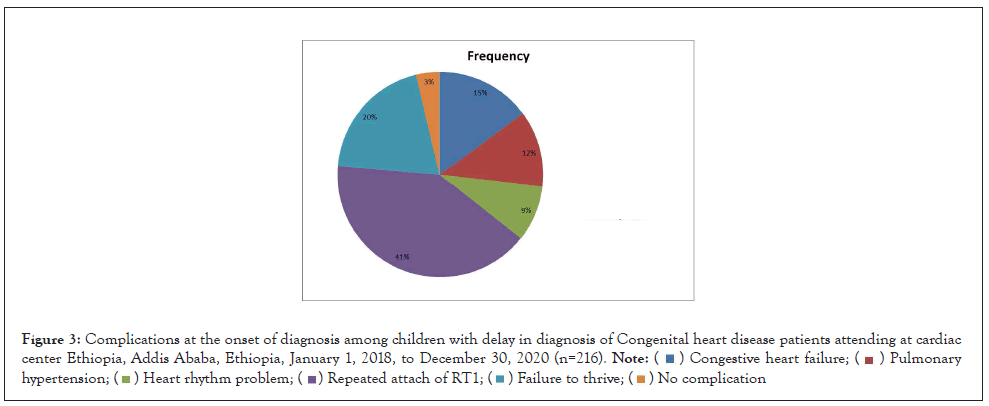
Figure 3: Complications at the onset of diagnosis among children with delay in diagnosis of Congenital heart disease patients attending at cardiac
center Ethiopia, Addis Ababa, Ethiopia, January 1, 2018, to December 30, 2020 (n=216).
 .
.
Factors associated with delay in diagnosis of congenital heart disease
In the bi variable logistic regression was conducted to identify associated variables with delay in diagnosis of congenital heart disease of the study participants. These are age, area of residence, maternal education, Socio-economic status, Place of child delivery, Family history of Congenital Heart Disease, and Gestational age in weeks and Types of Congenital Heart Disease. Accordingly, eight variables had a significance level of less than 0.25 with delay in diagnosis of congenital heart disease. All eight variables were entered into logistic regression for identifying significant variables of which three variables had an association with delay in diagnosis of CHD with a significance value of p- value less than 0.05 (Table 3).
| Characteristics | Delay in diagnosis | COR 95%CI | P-Value | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Area of residence | Urban | 36 (17.5%) | 5 (50.0%) | 0.212 (0.058-0.770) | 0.018 |
| Rural | 170 (82.5%) | 5 (50.0%) | 1 | ||
| Maternal education | Illiterate | 48 (23.3%) | 6 (60.0%) | 0.203 (0.055-0.747) | 0.017 |
| Literate | 158 (76.7%) | 4 (40.0%) | 1 | ||
| Place of child delivery | Hospital | 77 (37.4%0 | 9 (90.0%) | 0.066 (0.008-0.534) | 0.011 |
| Health Center | 129 (62.6%) | 1 (10.0%) | 1 | ||
| Body weight of child during diagnosis cat | <16 Kg | 110 (53.4%) | 9 (90.0%) | 0.127 (0.016-1.023) | 0.053 |
| >/=16 | 96 (46.6%) | 1 (10.0%) | 1 | ||
| Family history of CHD |
Yes | 16 (7.8%) | 4 (40.0%) | 0.126 (0.032-0.494) | 0.003 |
| No | 190 (92.2%) | 6 (60.0%) | 1 | ||
| Gestational age in weeks during delivery | 32-36 (Preterm) | 10 (4.9%) | 3 (30.0%) | 0.119 (0.027-0.531) | 0.005 |
| 37-42 (Term) | 196 (95.1%) | 7 (70.0%) | 1 | ||
Note: *Statistically significant predictors at P<0.25
Abbreviations: COR: Crude Odd Ratio; CI: Confidence Interval; CHD: Congenital Heart Disease
Table 3: Bivariable logistic regression conducted between delay in diagnosis and independent variables of delay in diagnosis of congenital heart disease patients attending at cardiac center Ethiopia, Addis Ababa, Ethiopia, January 1, 2018, to December 30, 2020.
Variables with a p-value<0.25 in bi variable were transferred to multivariable logistic regression. Age, maternal education, and types of congenital heart disease were found to be independent predictors of delay in diagnosis in multi variable regression analysis at p-value<0.05.
In multivariable logistic regression analysis, Maternal education those who had illiterate about 0.135 times more likely than delay in diagnosis of literate mother [AOR=0.135 (95% CI= (0.025-0.715))].
Place of child delivery in Hospital about 0.057 times less likely delay in diagnosis of CHD than delivery in Health center [AOR=0.057(95% CI=(0.005-0.643)]
Gestational age in weeks during delivery preterm baby 0.110 times more delay in diagnosis of CHD than term baby [AOR=0.110 (95% CI (0.017-0.723))] (Table 4).
| Characteristics | Delay in diagnosis | COR (CI 95%) | AOR (CI 95%) | P-value | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Maternal education | Illiterate | 48 (23.3%) | 6 (60.0%) | 0.203 (0.055-0.747) | 0.135 (0.025-0.715) | 0.019* |
| Literate | 158 (76.7%) | 4 (40.0%) | 1 | 1 | ||
| Place of child delivery | Hospital | 77 (37.4%) | 9 (90.0%) | 0.066 (0.008-0.534) | 0.057 (0.005-0.643) | 0.021* |
| Health Center | 129 (62.6%) | 1(10.0%) | 1 | 1 | ||
| Gestational age in weeks during delivery | 32-36(Preterm) | 10 (4.9%) | 3(30.0%) | 0.119 (0.027-0.531) | 0.110 (0.017-0.723) | 0.022* |
| 37-42 (Term) | 196 (95.1%) | 7 (70.0%) | 1 | 1 | ||
Note: *Statistically significant predictors at P<0.05
Abbreviations: COR: Crude Odd Ratio; AOR: Adjusted Odds Ratio; CI: Confidence Interval; CHD: Congenital Heart Disease
Table 4: Multivariable regression between delay in diagnosis and independent variablesof delay in diagnosis of congenital heart disease patients attending at cardiac center Ethiopia, Addis Ababa, Ethiopia January 1, 2018, to December 30, 2020.
Delay in diagnosis of CHD carries a serious risk of preventable mortality, morbidity, and permanent handicap [10]. Furthermore, failure to thrive, recurrent infections, and under nutrition adversely affects the long term health of the children. Limitations in daily activities also have a major impact on social development of these children.
In this study, it was shown that 95.4% children were having delayed diagnosis of congenital heart disease. In previous study showed about 85.1% were delayed diagnoses of CHD [14]. The finding is higher than the previous study. This might be due to no screening of CHD after delivery of the child in the health facilities. So, to decrease this delay give training for health professional who attend delivery for screening of children before discharge to home and on ANC follow-up screening of the mother to decrease delay in diagnosis of CHD and its complication.
In present study, about 38.4% were male and 61.6% were female. In similar study shown 58.9% of male and 40.1% of female patient have delay in diagnosis of CHD [21]. There is a difference on gender with CHDs. There might be due to study subjects that included during study period.
In present study 81% children who live to rural areas of residence. In other study about 63.4% children live in rural areas of residence. However, the finding was higher than previous study. It might be due to our country about 78.3% of population were lived in rural. So, the health facilities in rural areas they are no trained on screening of CHD.
In this study, maternal education as illiterate was seen among 25% of mother. In other study 43% of mother was illiterate [21]. The finding was lower than previous study maternal illiteracy is less awareness than literate mother. So, the maternal announces screening of fetal echocardiography during ANC.
In this study socio-economic status was low 66.7%, middle 27.8% and upper 5.6%. In previous study low in 54.3%, middle in 37% and high in remaining 8.7% monthly family income [21]. This might be due to economic status of the country.
The current study found that a cyanotic CHD was 94.9% and cyanotic CHD was 5.1% children. While in previous study a cyanotic CHD was 67.9% and cyanotic CHD was 32.1% children [21]. There is a difference; this might be due to difficult to differentiate their symptoms related to a cyanotic CHD immediately. In this study, maternal fetal echocardiography was 0.9% done. In another study shown maternal fetal echocardiography was 4.9% done [21]. However, this finding was lower than what was found in other study. This might be due to lack of trained health professional on maternal echocardiography during ANC follow-up. So, maternal fetal echocardiography must be functional by giving training for health professional.
In present study body weight below 3rdcentile was seen in 33.8% from 127 of less than 5 years Children. In previous study the patients weighing below the 3rdcentile for age 56.8% [14]. However, this finding was lower than what was found in previous study it might be due to only seen in less than 5 years of children was seen. In this study about 127 /43 (33.8%) children were having less than five years malnutrition as well. Regional data suggests that malnutrition is noted have prevalence around 26% among children, but in the present study it was seen in much higher proportion highlighting the fact that children with delayed diagnosis of CHD are much more exposed to malnutrition than other children [32]. Children with malnutrition are found to have increased rates of morbidity and mortality. Also, this is due to complications of delay in diagnosis of CHD. The solution is if early diagnosis of CHD complications does not occurred.
In this study the most common factor contributing to delayed diagnosis of CHD was found to be delayed due to health care provider in 89.4%. Delayed in referral was the second most frequent factor contributing to delayed diagnosis of CHD about 6% children. Delayed in financial were observed in 2.3% children. In another study, the most common delay in diagnosis of CHD was due to the delayed diagnosis by health care providers 22.5%, delayed referral/follow-up 13.3% [14]. This might be due to primary healthcare settings; lack of awareness about CHD by health care provider might explain these delays. The clinical features of children with CHD are various, thus the diagnosis is challenging. These clinical signs including cough, dyspnea, and failure to thrive, can be misinterpreted as symptoms of other diseases and managed until the alternate diagnosis of CHD are established. Some patients in our study were diagnosed with Respiratory tract infection and received treatment but they did not get better. Respiratory tract infection is one of the diseases reported in misdiagnoses of CHD in children due to their similar symptoms namely failure to thrive, and their frequent incidence in health facility.
Delay in diagnosis of children with CHD significantly affects the outcome. Children tend to present with several complications at the onset of diagnosis. In present study, about 41% of repeated attach of respiratory tract infection of children. In previous study, pneumonia 77.4% of children had complication [20]. This might be due to CHD being able to cause several abnormalities of the lungs and which can impact gas exchange. In this study, about 20% of the children with CHD presented with congestive heart failure. These findings were higher than data reported by Mocumbi et al., reporting only 8.8% of patients with heart failure at the CHD diagnosis [23]. Heart failure is the most common consequence of CHD. A 3/1000/year incidence of heart failure has been reported in children with CHD and has become the main cause of mortality and the second cause of mortality and morbidities in adults with CHD [33].
About 12% of patients with CHD had pulmonary hypertension, a condition characterized by elevated pulmonary arterial pressure often resulting in right ventricular failure. Pulmonary hypertension was associated with worsening outcome in children with CHD [34].
Delay in diagnosis of CHD was distinguished among 95.4% of CHD cases. A cyanotic CHD was the most common lesion and had a significantly longer delay in diagnosis than cyanotic CHD. Most common factors contributing to delayed diagnosis of CHD were delayed due to health care provider, delayed in referral and delayed financial factors. Many factors including, illiteracy, inadequate health facilities, inappropriately trained health professionals at health facilities level, lack of antenatal and immediate postnatal screening program, improper referral system and financial issues were identified as causes of delay in diagnosis of CHD in our setup. Maternal education, place of child delivery and gestational age were independently associated with the delay diagnosis of congenital heart disease. The most common complications in this study were repeated history of respiratory tract infection due to delayed diagnosis of CHD. Therefore improving the basic socioeconomic indicators and establishing a proper screening and referral healthcare delivery system are help full.
Limitation of this study was shortage of literature related to this study and data collection time was not enough. There was a network problem on phone call during data collections time. If this study design was prospective study design the best one.
For health professionals
Health professionals at different levels should have adequate knowledge about screening of children during birth attending especially those who are at risk mothers.
For policymakers
Policymakers must include training on assessments of maternal fetal Echocardiography and newborn assessing before discharging from delivery room to home to decrease delay in diagnosis of CHD. Therefore recommend developing a policy of CHD screening for newborns in Ethiopia.
For researchers
Researchers can use this research while using prospective study design and this study is for the first time in our county so, it will be an extra need further doing.
I want to express my great thanks to SPHMMC, Department of Medical Surgical Nursing, and Postgraduates Cardiovascular Nursing Programs for its usual facilities and outstanding chances to attend master’s program in Cardiovascular Nursing. My deepest heartfelt gratitude goes to my advisors Sr. Hirut Megersa (MSc, PhD Fellow) and Sr. Tigist Tsegaye (BSc. MSc.) who has been a great help to develop this Thesis paper. In addition, I like to extend my appreciation to those who have helped me a lot in giving additional advice.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Hurisa T, Megersa H, Tsegaye T (2022) Delay in Diagnosis of Congenital Heart Disease and Associated Factors Among Pediatric Patients in Cardiac Center Addis Ababa, Ethiopia, 2021 G.C. Clin Pediatr. 7:207.
Received: 02-May-2022, Manuscript No. CPOA-22-16316; Editor assigned: 04-May-2022, Pre QC No. CPOA-22-16316 (PQ); Reviewed: 19-May-2022, QC No. CPOA-22-16316; Revised: 23-May-2022, Manuscript No. CPOA-22-16316 (R); Published: 02-Jun-2022 , DOI: 10.35248/2572-0775.22.7.207
Copyright: © 2022 Hurisa T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.