Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2020)Volume 9, Issue 3
Background: Depressions in person with physical disabilities are three times more common than in the general population. In Ethiopia, there are an estimated 15 million persons with disabilities. Despite the high burden of disability, very little is known about it; for this reason, the current study aimed at determining the magnitude of depression and its associated factors among adults with a physical disability.
Methods: The study is a cross-sectional type conducted on individuals with a physical disability registered in Gondar physical disability’s rehabilitation and vocational center. All individuals with a physical disability attending the rehabilitation center were enrolled in the study. Face to face interview technique was used to evaluate the existence of depression and its determinants. In this study, the Beck Depression Inventory scale II was used to assess the status of depression. A multivariate logistic regression model was employed to see the strength, as well as the direction of the association between Depression and independent variables.
Results: The study found that the frequency of depression was determined as 75.5%. Having a perceived internal stigma 5.03 (AOR=5.03 (95% CI: 2.30, 9.99), Poor social support (5.36 (AOR=5.36 (95% CI: 2.41, 10.8) and those who consume alcohol (2.77 (AOR=2.77 (1.24, 6.17) were associated likely to have depression.
Conclusion: In this study, depression found to be a major health problem among adults with a physical disability. Early detection and regular screening for depression to give timely treatment as well as make the training fruitful, designing educational programs to build the community’s awareness to providing good social support and creating a sense of confidence and self-reliance in people with a physical disability would be helpful.
Adults; Physical disability; Depression; Ethiopia
AOR: Adjusted Odds Ratio, CI: Confidence Interval, COR: Crude Odds Ratio, GOR: Odds Ratio, PwPD: People with Physical disability, GTPRVC: Gondar town Physical Rehabilitation and vocational training Center (GTPDRVTC), WHO: World Health Organization
Globally, More than 264 million people are affected by depression; it indicates that depression is taking the highest part on the overall global burden of disease that causes social and occupational impairment [1,2]. Having a physical disability is one of the major causes or a potential risk factor for developing depression [3,4]; as studies evidenced that people with a physical disability (PwPD) are at least three-fold higher to develop depression than people without disability [5,6].
Commonly, a physical condition that limits a person's activities, senses, or movements can be described as a Physical disability [7]. A report from the World health organization (WHO), Globally, about 15% of the world's population has some form of disability, out of which 210 million (70 percent) live in developing countries [8,9].
From kinds of literature, the prevalence of depression in adults with disabilities has been estimated at 24.9% to 41% [10,11]. Negative social and personal attitudes towards disability, illiteracy, unemployment, stressors related to the low economical status, substance use, and environmental barriers like services, systems, and policies that are either nonexistent or that hinder the involvement of them were possible risk factors to develop depression among PwPD [5,12-14]. Particularly, a combination of physical disability and depressive symptoms can have a negative impact on the individual ’ s cognition and social functioning as well as a mortality risk for suicide [15].
In Ethiopia, Based on the WHO’S Report on Disability, there are an estimated 15 million persons with disabilities, representing 17.6 percent of the population [16]. In the community, they are considered as ugly and the spirit works on them; As a result, a family with an individual who has a disability considers them they are a burden and would not be useful to the community, as well as they are intellectually impaired too [17]. Therefore, they are excluded from almost all sectors including employment and education [18]; for these reasons, almost all (95%) of them are under poverty and most live by begging, are cared for by their families, or die of neglect [16,19].
Taking the problem in advance, the Government of Ethiopia has adopted and implemented a number of laws, policies, and standards on people with disabilities, including their right to productive and decent work, together with the provision of necessary rehabilitation and support services [19]; Nonetheless, there is still some doubt about the functionality of the legal and policy environment in setting the stage for giving full recognition to PwPD [19]; especially, their mental health condition is majorly neglected. Even if, the problem has taken the highest place, a single study can’t rule out there depression status and possible associated factors; therefore, this study was aimed to determine their depression status and its determinants among PwPD.
Noticing the problem could help local decision-makers as it helps to re-design a comprehensive strategy and put on the ground to tackle the problem as early as possible. For the rehabilitation center, it might be helpful to transfer the training program effectively with a shorter period since having depression can significantly interfere with the individual's functionality. Furthermore, for the individuals; it helps to create awareness, build psychological wellbeing, and tackling the determinants, accordingly.
The study area, design, and population
A cross-sectional institution based study was conducted in two phases of data collection period, the first phase of the data collection was conducted from October 15-25, 2019. Then, the second phase was continued on April 01-10, 2019; since the training has been given in two phases per annum (half a year for each) for the selected different trainees. The study was carried out at Gondar town Physical Rehabilitation and vocational training Center (GTPDRVTC) found in Gondar town, 750km away from Addis Ababa, the capital of Ethiopia. The training center was established by Emperor Halesilasie in 1963 E.C. At a time, it was named as center of help and was serving elder individuals, orphans, and physically disabled persons. Since 1989 E.C changes its name to Gondar Rehabilitation Center and vocational training serves, as a center for Amhara regional state (ARS).
Nearly for the last 10 years, the center was rendering service for about 1501 individuals with a physical disability. It has a capacity of giving training for 100 to 150 individuals at a time for a half-year period, twice a year. The center providing services to individuals came from different zones, woredas, and sub-cities in the ARS. Amhara region is one of the nine ethnic divisions of Ethiopia, containing the second-highest density of the Ethiopian population by accounts for 27% [20].
Mainly, the center is delivering training on Width of clothing/ Tailor/, weaving sewing, information communication technology, electronics maintenance, and metal and woodwork. All PwPD (Impairment in upper, lower, or both extremities) in the rehabilitation center was considered as a source population, whereas those who are available in the study period were considered as a study population.
Inclusion and exclusion criteria
Those patients who were 18 and above years-old with a physical disability were included in the study, rather individuals with a diagnosed mental disorder and those who are seriously ill and can’t give the expected response were excluded in the study.
Sampling size determination and sampling technique
All individuals with a physical disability attending GTPDRVTC in the study period were included.
Data collection tools and procedures
English language to Amharic (local language) experts translated questionnaires were used to collect the entire data. The questionnaires were adapted from previously published articles and the tools were comprised of socio-demographic characteristics, measurements of substance use, and depressionrelated information. A face to face interviewing method was used to collect the data. The outcome variable was measured by using the Beck Depression Inventory-II scale; accordingly, those who scored > 14 in the BDI- -II scale were considered as having depression [21].
To measure social support status, the Oslo-3 Social Support Scale was used to the study participants. Accordingly, participants who scored 12-14, 9-11, and 3-8 were categorized as having good, moderate, and poor social support, respectively [22].
A 3-items tool on perceived stigma screening was used to assess the participants’ perceived stigma. A little medication was made for addressing individuals with a physical disability. Thus, a score of less than one indicates the absence of perceived stigma whereas a score one or more indicates the presence of perceived stigma [23].
The severity of the disability was measured by using a scoring grid that takes into account both the intensity of the difficulties (no difficulty, some difficulty, a lot of difficulties, or cannot do), and the frequency of the activity limitations (never, rarely, sometimes, often, or always), a score is assigned to each of the physical disability types (disability on upper, lower or both extremities).
Hence, a person who reports always being limited in his or her activities and being unable to do an activity will have the maximum score for that disability type. Accordingly, the most severe responses have higher scores, moderate responses have mid-range scores, and mild responses have lower scores [24]. Regarding substance use, use of at least any of the following substances: alcohol, Khat, and cigarette for the last one year including the training period that is assumed to affect the level of thought and increase the risk of depression [25]. To assure the quality of the data, training was given for data collectors regarding the techniques of interviewing as well as filling the checklist for two-hours. Three-degree holder nurses for data collection and One MSc holder psychiatry nurses for supervision were recruited. Finally, the completeness of questionnaires was checked regularly.
Data processing and analysis
Data were coded and entered into EPI info version 7 and exported into a Statistical Package for Social Science (IBM-SPSS) Version 21.0 for further analysis. The outcome variable, Depression was coded as ‘0’ and ‘1’ representing without and with the problem, respectively. Data summary measures like texts, tables, and figures were used to show the study findings. The binary logistic regression analysis was employed to identify the associated independent variables with Depression.
Accordingly, variables that had a p-value of ≤0.05 in the bivariable analysis were entered into the multivariable regression model to control the effects of confounders as well as to identify the significant factors. Finally, variables having a p-value of ≤ 0.05 in multivariate analysis were considered as statistically significant; adjusted odds ratio and p-value with a 95% CI were used to the interpretation of the data.
Socio-demographic variables
With a 100% response rate, a total of 224 study participants were enrolled in the study. The median age of participants was 26.3 (SD ± 5) years with a range of 25-34 years old. Of the participants, a bit greater than half (57.1%) were Female, a majority (82.1%) were orthodox in religion, just three quarter (75.9%) was single in marital status. Moreover, a significant majority (66.1%) of the participants were living in the Urban part of the state, a bit greater than a third (36.6%) completed secondary level of education and almost majority (40%) of the participants were unemployed (Table 1).
Table 1: Sociodemographic characteristics of the participants with a physical disability at Gondar rehabilitation center, 2019.
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Age | ||
| 18-24 | 94 | 42 |
| 25-34 | 102 | 45.5 |
| ≥ 35 | 28 | 12.5 |
| Sex | ||
| Female | 98 | 42.9 |
| Male | 128 | 57.1 |
| Religion | ||
| Orthodox | 184 | 82.1 |
| Muslim | 38 | 17 |
| Catholic | 2 | 0.9 |
| Marital status | ||
| Single | 170 | 75.9 |
| Married | 40 | 17.9 |
| Divorced | 12 | 5.4 |
| Widowed | 2 | 0.9 |
| Residency | ||
| Urban | 148 | 66.1 |
| Rural | 76 | 33.9 |
| Educational status | ||
| Unable to read and write | 56 | 25 |
| Primary education | 72 | 32.1 |
| Secondary education | 82 | 36.6 |
| Certificate and Diploma | 14 | 6.3 |
| Employment status | ||
| Employer | 8 | 3.6 |
| Private business | 34 | 15.2 |
| Daily labor | 22 | 9.8 |
| Student | 70 | 31.3 |
| Unemployed | 90 | 40.2 |
Injured body part
Among the participants, a large proportion (65.2%) of them had experienced the physical disability on the problem in lower extremity (Figure 1).
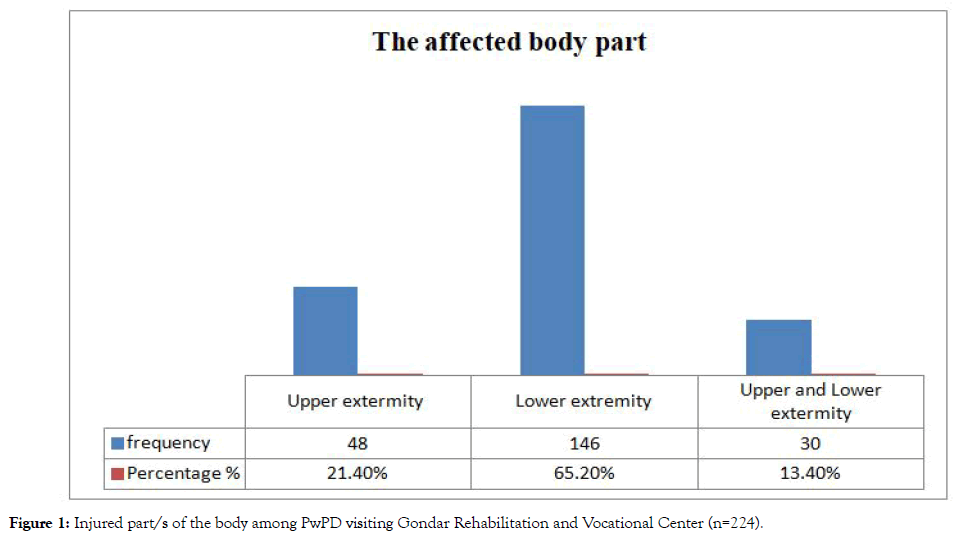
Figure 1: Injured part/s of the body among PwPD visiting Gondar Rehabilitation and Vocational Center (n=224).
Disability-related variables
Roughly a third (37.5%) of participants reported that the disability has happened from birth (congenital). In the severity of the disability, more than half (54.5%) rated their disability status as severe (Table 2).
Table 2: Disability-related variables of the participants with a physical disability at Gondar rehabilitation center, 2019.
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Causes of disability | ||
| Congenital | 84 | 37.5 |
| Car accident | 24 | 10.7 |
| War | 16 | 7.1 |
| Fire accident | 36 | 16.1 |
| Others* | 64 | 28.6 |
| The severity of a disability | ||
| Low | 16 | 7.1 |
| Medium | 86 | 38.4 |
| Severe | 122 | 54.5 |
Others*: Stick and fall down injury
History of chronic illness
Responses regarding the history of having Chronic illness, nearly a quarter 48 (21.4%) of participants had a chronic illness; Chronic heart-related diseases was rating the highest (14.3%) than Diabetic Mellitus (1.8%), Hypertension (0.9%) and HIV/ ADIS (4.5%), respectively.
Psycho-social variables
Related to getting good social support and having perceived internal stigma, just a half (50.9%) of the respondents had poor social support, whereas three quarter (75.9) of the study participants had perceived internal stigma regarding their disability (Table 3).
Table 3: Psycho-social variables of the participants with a physical disability at Gondar rehabilitation and vocational center, 2019.
| Variables | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Social /Family/Support | |||
| Good | 60 | 26.8 | |
| Medium | 50 | 22.3 | |
| Poor | 114 | 50.9 | |
| Perceived stigma | |||
| Yes | 170 | 75.9 | |
| No | 54 | 24.1 | |
History of substance use
In line with substance use, More than three quarter 180 (80.4%) of the participants had a history of alcohol consumption, especially a local drink “Tela.” Whereas, a small minority 32 (14.3%) and 30 (13.4%) of the respondents were smoking a cigarette and chewing khat (Chat), respectively.
Prevalence of depression among people with a physical disability
Nearly three quarters 70.5% (95% CI: 64.3% - 76.8%) of the participants with a physical disability had depression.
Factors associated with depression
Bi-variable and multivariate analyses were conducted to test the association between different independent variables and Depression. Variables that were associated (p ≤0.05) in the bivariable analysis were run in the multivariable analysis; perceived internal stigma, poor social support, and alcohol use were associated with depression among PwPD (Table 3).
The odds of developing depression among participants who had perceived internal stigma was 5.03 (AOR=5.03 (95% CI: 2.30, 9.99)) times higher than their counterparts. The likelihood of experiencing depression among participants who had poor social support was about five times higher than those participants who received good social support (5.36 (AOR=5.36 (95% CI: 2.41,10.8)). Moreover, the odds of developing depression among Alcohol users were nearly three times higher than those respondents who didn ’ t use alcohol (2.77 (AOR=2.77 (1.24, 6.17)) (Table 4).
Table 4: Bi-variable and multivariable factors associated with depression among people with a physical disability at Gondar rehabilitation and vocational center (n=224).
| Explanatory variables | Depression | COR | AOR | P-value | ||
|---|---|---|---|---|---|---|
| Yes | No | (95% CI) | (95% CI) | |||
| Residency | ||||||
| Urban | 96 | 52 | 1 | 1 | 0.69 | |
| Rural | 62 | 14 | 2.39 (1.23,4.69) | 2.76 (0.12,5.99) | ||
| Injured body part | ||||||
| Upper extremity | 24 | 16 | 1 | 1 | -- | |
| Lower extremity | 100 | 42 | 1.58 (0.76,3.28) | 1.88 (0.79,4.49) | 0.15 | |
| Upper and Lower extremity | 34 | 8 | 2.83 (1.04,7.67) | 1.87 (0.58,5.96) | 0.28 | |
| Severity of disability | ||||||
| Low | 8 | 8 | 1 | 1 | -- | |
| Medium | 56 | 30 | 1.86 (0.64,5.47) | 1.31 (0.37,4.61) | 0.67 | |
| High | 94 | 28 | 3.35 (1.15,9.75) | 2.66 (0.75,9.35) | 0.12 | |
| Perceived stigma | ||||||
| No | 24 | 30 | 1 | 1 | 0.01 | |
| Yes | 134 | 36 | 4.65 (2.42,8.91) | 5.03 (2.30,9.99) | ||
| Social support | ||||||
| Good | 32 | 28 | 1 | 1 | -- | |
| Medium | 32 | 18 | 1.55 (0.72,3.35) | 3.36 (1.32,8.55) | 0.01 | |
| Poor | 94 | 20 | 4.11 (2.04,8.28) | 5.36 (2.41,10.8) | 0.01 | |
| Alcohol consumption | ||||||
| No | 25 | 19 | 1 | 1 | 0.01 | |
| Yes | 133 | 47 | 2.15 (1.08,4.25) | 2.77 (1.24,6.17) | ||
In the current study, 75.5% of adults with physical disabilities were detected to have depression, which implies that it is a significant public health concern and demanding a welldesigned and comprehensive strategy. This finding is consistent with a study conducted in Iran 71% [26]. Nonetheless, it’s far higher than studies in Turkish 57.8% and Colombia 24% [3,27], This lack of clarity could be associated with study design such as sample size and measures of depression as well as the difference in cultural characteristics too [3,27].
An important finding observed in this study is the Perceived stigma, Perceived internal stigma positively predicted depression among PwPD. The finding is supported by kinds of literature [28,29]. This is reasonable that Physical disability either innate or acquired may lead them to experience feelings of inadequacy [30]. Moreover, the societies misconception about the cause and nature of disabilities (as a punishment or fate from God and it is contagious) or stereotyping (negative evaluation of a label) and prejudice (endorsement of the negative stereotypes) attitudes [31] are also lead them to experience emotional as well as thought disturbances that could have a predicator for developing the feeling of stigmatized [32,33]. In Ethiopia, Disability is an extremely taboo issue, and there is a general inclination to think of them as weak, hopeless, dependent, and unable to learn and the subject of charity, which leads them to develop a sense of stigmatized by others [34]. Therefore, perceived internal stigma could be a major obstacle and limit their opportunities for work and social functioning, which demand a strong effort of policymakers, local decision-makers, and other stakeholders to promote psychological support for the victims.
In the current study, Depression was significantly associated with participants who had poor social support. Similar results have been reported in various studies [35-37]. As Motl et al. and Lenze et al. reported, this situation can be explained by having a disability may lead them to develop depression via the psychosocial effects such as social activity restriction and poverty for the reason that of lack of attention and support by others [38,39]. In Ethiopia, society’s often linked the disability with a person’s immorality or curse [40]. As a result, as Brhena et al. stated, they are excluding from social events through lack of belongingness, acceptance, and recognition; therefore, they are more vulnerable to economic and social problems, difficult life experiences, and experiencing psychological problems [41]. Since the psychosocial benefit of social support among this segment of the population is crucial for better mental, physical and psychosocial wellbeing [42,43]; poor societal support could affect the individual ’ s overall health, troubles the day-to-day work-related activities, problems on the relationship, and financial productivity which demands strong governmental support to design different mechanisms by which PwPD can receive appropriate support service in the context of their family and community environment shall be created.
The study evidenced that the higher odds of experiencing depression were observed among those participants who had a history of alcohol consumption. The find is supported by a kind of studies [44-47]. This could be explained by PwPD have an increased risk for drug addiction owing to unemployment and poverty, increased risk of physical abuse, Social isolation, lack of access to education and increased risk of developing a mental illness [45,48]. As a result, they are prone to interfere with successful engagement in rehabilitation services, impair cognition, reduce the ability to follow self-care regimens, contribute to social isolation, poor communication, and the hastening of disabling diseases like depression [48]. Taking this in mind, the national responsible governmental bodies should be designed and implement accessible, targeted prevention programs as well as building treatment services and facilities for those substance abusers.
Doing the study on the overlooked filed that is mental health in this segment of the population by incorporating crucial variables like social support and perceived internal stigma are the good looks of the study. Therefore, it could be an alarming study to the responsible body’s pleasing to the eye on mental health. Nonetheless, The fact that the study was a cross-sectional survey conducted only on PwPD registered in GTRVC, the generalizability issue is in question, even if the participants came from different parts of the Amhara regional state. Furthermore, it would have been more novel if the study was conducted in the community based by incorporating people with a sensory disability and complemented by qualitative studies to explore possible reasons for having depression.
In a nutshell, the result of this study showed that depression among PwPD was significantly high. Those participants who had perceived internal stigma, poor social support and alcohol users were experienced depression more. To instill a sense of confidence and self-reliance among PwPD, the rehabilitation center shall be drawing education and motivational programs on mental health, in general. Likewise, to overcome the existing harmful traditional attitudes, norms, and practices concerning the determinants of and consequence of the problems in respect to Physical disability, the government and other NGO’s shall be re-design and implement appropriate and sustainable educational program launched to significantly raise the level of public awareness through mass media and other social media’s. Furthermore, for better training engagement and minimizing the chance of contracting depression because of Alcohol consumption, lunching different educational programs regarding accessible and targeted prevention programs as well as building treatment services and facilities for those substance abusers are highly recommended.
Ethical approval was obtained from the Institutional Review Board committee of University of Gondar, School of nursing. All process was started after securing written consent from the institutional board review and the rehabilitation center. Written informed consent was obtained from the study participant after adequately informed about the purpose, method & anticipated benefit of the study. As well, they were informed about their right to ask any question, refuse, and withdraw from the study, at any time.
DAG designed and conducted the study. DAG, DN and ZBT, analyzed data, developed, and approved the final version of the manuscript.
The authors appreciate the data collectors as well as the study participants.
Citation: Gebeyehu DA, Negaa D, Tezera ZB (2020) Depression in Adults with a Physical Disability: An Institution Based Cross Sectional Study. J Dep Anxiety. 9:365. doi: 10.35248/2167-1044.20.9.365.
Received: 30-May-2020 Accepted: 17-Jul-2020 Published: 24-Jul-2020 , DOI: 10.35248/2167-1044.20.9.365
Copyright: © 2020 Gebeyehu DA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.