Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2024)Volume 15, Issue 3
Background: Autoimmune bullous disorders can affect the skin, mucous membranes and nails. Dermoscopic nail changes in autoimmune bullous disorders either with clinically affected or subclinically affected nails have not been demonstrated up to date.
Aim: To study occurrence and percentage of dermoscopic nail changes in various autoimmune bullous disorders.
Materials and methods: One hundred participants were recruited in this study. Half of them (fifty patients) had different autoimmune bullous diseases and were grouped according to their nail affection into two groups, group 1: Patients with clinically affected nails, and group 2: Patients with clinically apparent normal nails (with subclinical changes). All parts of finger nails were examined by dermoscopy and were compared with fifty age and sex matched healthy volunteers.
Results: Dermoscopic nail changes were observed in 88% of patients with autoimmune bullous diseases and 44% of controls. In group 1: The most frequent dermoscopic findings were onychorrhexis 52%, splinter hemorrhage 40% and onychomadesis 40% while in group 2: 24% had no dermoscopic findings, 48% had splinter hemorrhage and it was significantly higher than group 1 (p<0.001), 28% had Beaus’ lines, then onycholysis and onchomycosis 24% for each. In both groups, onychomycosis and longitudinal striations were significantly higher in those ≥ 50 years. While, in group1 only, Beau's lines and onychorrhexis were higher in those ≥ 50 years old. Also, splinter hemorrhage and periungual blister were significantly higher among those with disease duration less than 1 year in both groups.
Conclusion: Signs of clinical and subclinical involvement of nails in autoimmune bullous diseases can be appreciated well with the help of the dermoscope even in clinically unaffected nails. Splinter hemorrhage, onycholysis, onychomycosis and Beaus’ lines were dermoscopic signs detected in clinically free nails so appropriate dermoscopic nail examination in patients with Autoimmune Blistering Diseases (AIBD) is mandatory to detect early nail changes where treatment should be instituted to prevent permanent damage of nails.
Dermoscopy; Autoimmune bullous diseases; Nail; Pemphigoid; Pemphigus
Autoimmune bullous diseases including pemphigus and the pemphigoid group are characterized by appearance of cutaneous and mucous membranes lesions, due to the production of pathogenic autoantibodies directed against different proteins of desmosomes (desmogleins) or basement membrane zone proteins [1]. All antigens of normal skin are also normally expressed in the proximal nail fold, nail matrix, and hyponychium including desmoglein 1 and 3 [2]. According to various studies, the reported prevalence of nail changes in Autoimmune Blistering Diseases (AIBD) ranges from 31%-72% [1,3]. Patients with Pemphigus Vulgaris (PV) may present with nail abnormalities, which occasionally can precede skin findings. Nail lesions often relapse just before generalized disease exacerbation or recurrence [4]. On thorough searching the literature till now, no study has concerned the dermoscopic evaluation of nails in patients with various autoimmune bullous diseases. In this study, we have evaluated the occurrence and percentage of dermoscopic nail changes in autoimmune blistering disorders either with clinically affected or apparently normal nails (subclinically) and compared them with an age and sex matched healthy control group.
Patients and methods
The study included 100 participants, 50 patients with different autoimmune bullous diseases attending the outpatient Clinic of Dermatology, Venereology and Andrology Clinic, Assiut University Hospital during the period from July 2021 to August 2022. Also, fifty age and sex matched healthy volunteers were recruited as a control group. An informed written consent was obtained from all participants. The study protocol was registered at ClinicalTrials. gov with ID NCT04092413. The Ethical Approval no. is 17100865 exclusion criteria were those patients with history of any other skin or systemic disease that may affect their nails.
A detailed history was taken from each patient to determine the age of onset, duration, and evolution of the disease, oral, genital involvement, and the presence of any nail changes. A complete systemic and dermatological examination was performed. After a thorough examination, all the patients were subjected to histopathological studies of bullous lesions. Nail changes were photographed and evaluated in each patient independently by two experienced dermatologists. According to the nail involvement whether present or absent, patients were classified in to two groups, group 1 with clinically affected nails and group 2 with apparently normal nails (subclinically affected).
Dermoscopic examination of the 10 finger nails was performed by Dlite Microscope: Digital and video USB microscope camera (1.3 megapixels) using 30X and 50X lenses, all parts of the nails were examined including nail plate, nail bed, hyponychium, lateral nail folds, distal edge of the nail plate and proximal nail fold. Dry examination (without any interface medium) was used to visualize nail plate changes such as pits, scales or surface irregularities.Also, wet examination (using alcohol gel) was used to increase the transparency of plate and penetration of light to examine nail bed changes such as onycholysis and splinter hemorrhage. The pattern of dermoscopic involvement in each nail was documented and photographed. Similarly, clinical and dermoscopic examination of nails of 50 healthy volunteers (control group) were done and any changes were documented. Data was collected and analyzed using SPSS (Statistical Package for the Social Science, version 20, IBM, Armonk, New York). Chi square test and Fisher's exact test were implemented on such data.
This study included 50 patients with different AIBDS on immunosuppressive therapy and 50 healthy volunteers. The age of the cases ranged between 20 years and 88 years with mean age ± SD was 45.06 ± 15.8. 54% of the cases were female and 46% of them were males. The duration of disease ranged between 0.17 years and 15 years with mean duration ± SD 2.76 ± 3.64. The most frequent autoimmune bullous disease (50 cases) in both groups was pemphigus vulgaris 52.0% (n=26) followed by bullous pemphigoid 18.0% (n=9) and pemphigus foliacous 18.0% (n=9). Each of dermatitis herpitiformis, pemphigoid gestationis and linear IgA bullous dermatosis was reported in only two patients. The most frequent dermoscopic findings among group 1 was onychorrhexis 52% (n=13) (Figure 1), splinter hemorrhage and onychomadesis 40% for each (n=10) and onycholysis 32% (n=8) (Figures 2-4).
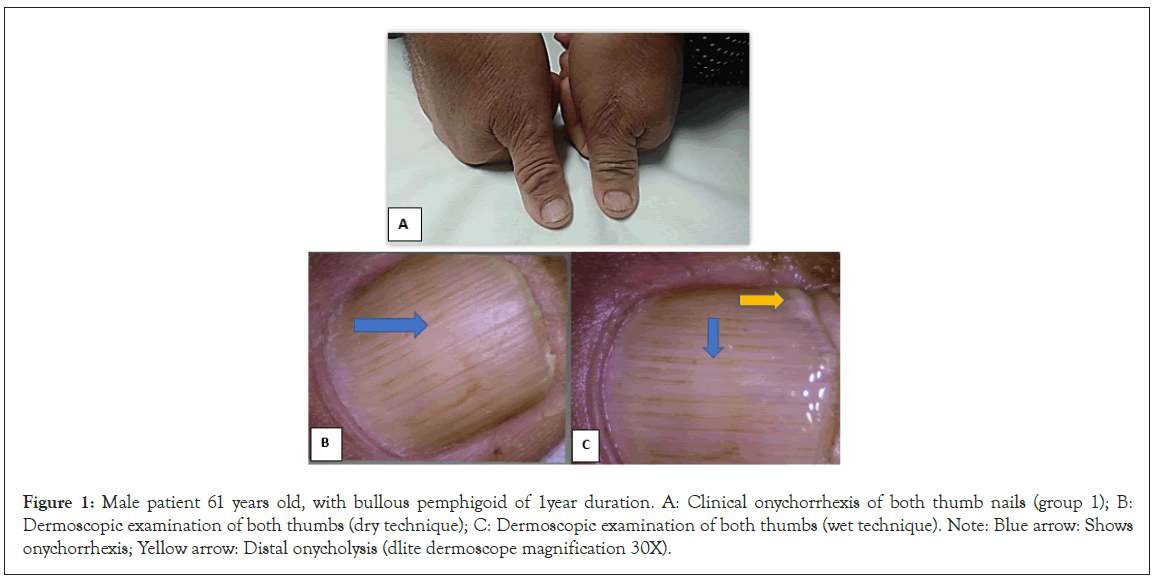
Figure 1: Male patient 61 years old, with bullous pemphigoid of 1year duration. A: Clinical onychorrhexis of both thumb nails (group 1); B: Dermoscopic examination of both thumbs (dry technique); C: Dermoscopic examination of both thumbs (wet technique). Note: Blue arrow: Shows onychorrhexis; Yellow arrow: Distal onycholysis (dlite dermoscope magnification 30X).
Figure 2: Male patient 56 years old, with pemphigus vulgaris of 3years duration. A: Clinical Beau's lines, onychomadesis of all finger nails and chronic paronychia of left index finger nail; B: Dermoscopic examination of two different fingers nails (dry technique); C: Dlite dermoscope magnification 30X. Note: Blue arrow: Shows Beau's lines; Red circle: Pitting; Yellow arrow: Onychomadesis.
Figure 3: Female patient 47 years old with pemphigus vulgaris of 1 year duration with clinically affected left thumb shows chronic paronychia and blackish discolouration; B: Dermoscopic examination of left thumb (dry technique); C: Nail tissue stained with PAS stain showing fungal hyphae. Note: Blue arrow: Shows chronic paronychia; Yellow arrow: Onychomadesis; Red arrow: Onychomycosis.
Figure 4: Male patient 52 years old, with pemphigus vulgaris of 3years duration. A: clinical distal onycholysis of some fingers; B: Dermoscopic examination of two different finger nails (dry technique). Note: Blue arrows: Shows distal onycholysis; Blue circle: Pitting; Red arrow: Beau's line; Yellow arrow: Onychorrhexis (dlite dermoscope magnification 30X).
Group 2 showed no dermoscopic findings in 24% of cases, while, splinter hemorrhage was the commonest dermoscopic finding among this group 48% (n=12), followed by Beau’s lines 28% (n=7), then onycholysis and onchomycosis 24% each. Nevertheless, splinter hemorrhage was significantly higher than group 1 (p<0.001). Some dermoscopic changes were discovered among clinically affected nails only (group 1) as onychorrhexis 52% (n=13), onychomadesis 40% (n=10), acute paronychia 24% (n=6), subungual hemorrhage 20% (n=5), periungual blisters 20% (n=5) and chronic paronychia 12% (n=3) (Table 1). Pitting and splinter hemorrhage were the only two findings in the control group 12% and 4% respectively.
| Nail findings | Group 1 (clinically) n=25 no. (%) |
Group 1 (dermoscopically) n=25 no. (%) |
Group 2 n=25 (dermoscopically) no. (%) |
Control group (dermoscopically) n=50 no. (%) |
P1 | P2 | P3 | P4 |
|---|---|---|---|---|---|---|---|---|
| No finding | 0 (0%) | 0 (0%) | 6 (24%) | 28 (56%) | <0.001 | 0.022 | <0.001 | 0.009 |
| Splinter hemorrhage | 5 (20%) | 10 (40%) | 12 (48%) | 2 (4%) | <0.001 | 0.569 | <0.001 | <0.001* |
| Onycholysis | 6 (24%) | 8 (32%) | 6 (24%) | - | - | <0.001 | - | - |
| Onychomadesis | 10 (40%) | 10 (40%) | 0 (0%) | - | - | 1 | - | - |
| Onychomycosis | 3 (12%) | 6 (24%) | 6 (24%) | - | - | 0.529 | - | - |
| Beau's lines | 6 (24%) | 7 (28%) | 7 (28%) | - | - | 1 | - | - |
| Onychorrhexis | 13 (52%) | 13 (52%) | 0 (0%) | - | - | <0.001 | - | - |
| Pitting | 2 (8%) | 3 (12%) | 0 (0%) | 6 (12%) | 0.192 | 0.235* | 1 | 0.170* |
| Subungual hemorrhage | 4 (16%) | 5 (20%) | 0 (0%) | - | - | 0.05* | - | - |
| Paronychia | - | - | - | - | - | 0.002* | - | - |
| Acute | 6 (24%) | 6 (24%) | 0 (0%) | - | - | - | - | - |
| Chronic | 3 (12%) | 3 (12%) | - | - | - | - | - | - |
| Periungual blister | 5 (20%) | 5 (20%) | 0 (0%) | - | - | 0.05* | - | - |
| Longitudinal striations | 2 (8%) | 5 (20%) | 5 (20%) | 10 (20%) | 1 | 1 | 1 | 1 |
| Leuconychia | - | - | - | 9 (18%) | - | - | - | - |
Table 1: Dermoscopic nail findings among patients with autoimmune bullous diseases and control group. Note: P1: p-value between clinical, subclinical cases and control group; P2: p-value between clinical and subclinical cases; P3: p-value between clinical cases and control group; P4: p-value between subclinical cases and control group; P-value was significant if ≤ 0.05: Chi-square test was used; (*): Fisher exact test was used.
Regarding those with pemphigus vulgaris (n=26), splinter hemorrhage was frequently observed in both groups 30.8% (group 1) and 38.5% ( group 2) and was significantly higher than control p=<0.001 (Figure 5), followed by onycholysis that was significantly higher in group 1 (38.5%) than group 2 (23.1%) and onychomycosis in group 1 (38.5%) and group 2 (30.8%), Beau’s lines was 30.8% in both groups, onychomadesis, onychorrhexis, subungual hemorrhage, paronychia and periungual blisters were detected in group 1 only (Table 2).
| Dermoscopic nail findings | Pemphigus vulgaris group 1 n=13 no. (%) |
Pemphigus vulgaris group 2 n=13 no. (%) |
Control n=50 no. (%) |
P1 | P2 | P3 | P4 |
|---|---|---|---|---|---|---|---|
| Splinter hemorrhage | 4 (30.8%) | 5 (38.5%) | 2 (4%) | <0.001 | 0.569 | <0.001 | <0.001* |
| Onycholysis | 5 (38.5%) | 3 (23.1%) | - | - | >0.001 | - | - |
| Onychomadesis | 7 (53.8%) | 0 (0%) | - | - | 1 | - | - |
| Onychomycosis | 5 (38.5%) | 4 (30.8%) | - | - | 0.529 | - | - |
| Beau's lines | 4 (30.8%) | 4 (30.8%) | - | - | 1 | - | - |
| Onychorrhexis | 6 (46.2%) | 0 (0%) | - | - | >0.001 | - | - |
| Pitting | 3 (23.1%) | 0(0%) | 6 (12%) | 0.192 | 0.235* | 1 | 0.170* |
| Subungual hemorrhage | 4 (30.8%) | 0 (0%) | - | - | 0.05* | - | - |
| Paronychia | 7 (53.8%) | 0 (0%) | - | - | 0.002* | - | - |
| Periungual blister | 4 (30.8%) | 0 (0%) | - | - | 0.05* | - | - |
| Longitudinal striations | 1 (7.7%) | 2 (15.0%) | 10 (20%) | 1 | 1 | 1 | 1 |
| Leuconychia | - | - | 9 (18%) | - | - | - | - |
Table 2: Dermoscopic nail findings among patients with pemphigus vulgaris and the control group. Note: P1: p-value between clinical, subclinical cases and control group; P2: p-value between clinical and subclinical cases; P3: p-value between clinical cases and control group; P4: p-value between subclinical cases and control group; p-value was significant if ≤ 0.05: Chi-square test was used; (*): Fisher exact test was used.
Figure 5: Female patient 50 years old with pemphigus vulgaris of 1 year duration, with clinically apparent normal nails. Dermoscopic examination of nails (dry technique) shows. Note: Blue arrow: Beaus’ lines; Yellow arrow: Distal onycholysis; Blue circle: Splinter haemorrhage; Red arrow: Longitudinal striations (sausage like appearance) (dlite dermoscope magnification 30X).
Among the pemphigus foliaceous patients, the most frequent finding was splinter hemorrhage in group 1 and group 2 (66.7%) for each. While in bullous pemphigoid, the most frequent finding was onychorrhexis (100.0%) in group 1 and splinter hemorrhage (33.3%) in group 2 (Figure 6 and Table 3).
| Type of AIBD | Group | Pemphigus vulgaris n=26 G1=13 G2=13 |
Pemphigus foliacous n=9 G1=3 G2=6 |
Bullous pemphigoid n=9 G1=6 G2=3 |
Dermatitis herpetiformis n=2 G1=1 G2=1 |
Pemphigoid gestationis n=2 G1=1 G2=1 |
Linear IgA bullous dermatosis n=2 G1=1 G2=1 |
p-value |
|---|---|---|---|---|---|---|---|---|
| Splinter haemorrhage | 1 | 4 (30.8%) | 2 (66.7%) | 2 (33.3%) | 0 (0.0%) | 1 (100.0%) | 1 (100.0%) | 0.4 |
| 2 | 5 (38.5%) | 4 (66.7%) | 1 (33.3%) | 0 (0.0%) | 1 (100.0%) | 1 (100.0%) | 0.06 | |
| Onycholysis | 1 | 5 (38.5%) | 1 (33.3%) | 2 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.89 |
| 2 | 3 (23.1%) | 2 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (100.0%) | 0.76 | |
| Onychomadesis | 1 | 7 (53.8%) | 1 (33.3%) | 2 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.66 |
| 2 | - | - | - | - | - | - | - | |
| Onychomycosis | 1 | 5 (38.5%) | 0 (0.0%) | 1(16.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.61 |
| 2 | 4 (30.8%) | 2 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.23 | |
| Beau's lines | 1 | 4 (30.8%) | 0 (0.0%) | 3 (50%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.57 |
| 2 | 4 (30.8%) | 2 (33.3%)) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (100.0%) | 0.66 | |
| Onychorrhexis | 1 | 6 (46.2%) | 0 (0.0%) | 6 (100.0%) | 1 (100.0%) | 0 (0.0%) | 0 (0.0%) | 0.03 |
| 2 | - | - | - | - | - | - | - | |
| Pitting | 1 | 3 (23.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.67 |
| 2 | - | - | - | - | - | - | - | |
| Subungual heamorrhage | 1 | 4 (30.8%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (100.0%) | 0.17 |
| 2 | - | - | - | - | - | - | - | |
| Paronychia | 1 | 7 (53.8%) | 1 (33.3%) | 0 (0.0%) | 0 (0.0%) | 1 (100.0%) | 0 (0.0%) | 0.15 |
| 2 | - | - | - | - | - | - | - | |
| Periungual blister | 1 | 4 (30.8%) | 0 (0.0%) | 1 (16.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.77 |
| 2 | - | - | - | - | - | - | - | |
| Longitudinal striations | 1 | 1 (7.7%) | 0 (0.0%) | 4 (66.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.05 |
| 2 | 2 (15.0%) | 0 (0.0%) | 2 (66.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.09 | |
| Number of dermoscopic nail findings (%) | 1 | 13 (100.0%) | 3 (100.0%) | 6 (100.0%) | 1 (100.0%) | 1 (100.0%) | 1 (100.0%) | - |
| 2 | 10 (76.9%) | 5 (83.3%) | 2 (66.7%) | 0 (0.0%) | 1 (100.0%) | 1 (100.0%) | 0.55 | |
| Total number of patients (%) | 1 | 13 (52%) | 3 (12%) | 6 (24%) | 1 (4%) | 1 (4%) | 1 (4%) | - |
| 2 | 13 (52.0%) | 6 (24.0%) | 3 (12.0%) | 1 (4.0%) | 1 (4.0%) | 1 (4.0%) | - |
Table 3: Percentage of clinical and subclinical dermoscopic nail findings among different types of autoimmune bullous diseases. Note: Group 1: Clinical cases p-value was significant if ≤ 0.05; Group 2: Subclinical cases Chi-square test was used.
Figure 6: Female patient 55 years old with pemphigus foliacous of 1year duration, with clinically apparent normal nails. Dermoscopic examination of both thumbs (dry technique) Note: Blue arrow: Beaus’ lines; Yellow arrow: Distal onycholysis; Blue circle: Splinter hemorrhages (dlite dermoscope magnification 30X).
Patients were grouped according to their ages into two groups (<50 years and ≥ 50 years). In both groups, longitudinal striations were significantly higher in those ≥ 50 years (G1: p-value=0.001, G2: p-value=0.009). While in group1 only, Beau's lines and onychorrhexis were higher in those ≥ 50 years old (p-value=0.021 and p-value=0.001 respectively), onychomycosis was significantly higher in those ≥ 50 years in group 2 only (p-value=0.047) (Table 4).
| Type of AIBD | Age (years) | p-value | ||||
|---|---|---|---|---|---|---|
| Group | <50 years G1: (n=16) G2: (n=13) % |
≥ 50 years G1: (n=9) G2: (n=12) % |
||||
| Splinter hemorrhage | No. | % | No. | % | ||
| 1 | 8 | 50 | 1 | 11.1 | 0.001* | |
| 2 | 5 | 38.5 | 7 | 58.3 | 0.009* | |
| Onycholysis | 1 | 4 | 25 | 4 | 44.4 | 0.317 |
| 2 | 4 | 30.8 | 2 | 16.7 | 0.409 | |
| Onychomadesis | 1 | 8 | 50 | 2 | 22.2 | 0.174 |
| 2 | - | - | - | - | - | |
| Onychomycosis | 1 | 1 | 6.3 | 5 | 55.6 | 0.06 |
| 2 | 1 | 7.7 | 5 | 41.7 | 0.047* | |
| Beau's lines | 1 | 2 | 12.5 | 5 | 55.6 | 0.021* |
| 2 | 4 | 30.8 | 3 | 25 | 0.748 | |
| Onychorrhexis | 1 | 4 | 25 | 9 | 100 | <0.001* |
| 2 | - | - | - | - | - | |
| Pitting | 1 | 3 | 18.8 | 0 | 0 | 0.166 |
| 2 | - | - | - | - | - | |
| Subungual hemorrhage | 1 | 4 | 25 | 1 | 11.1 | 0.405 |
| 2 | - | - | - | - | - | |
| Paronychia | ||||||
| Acute | 1 | 6 | 37.5 | 0 | 0 | 0.093 |
| Chronic | 2 | 2 | 12.5 | 1 | 11.1 | - |
| Periungual blister | 1 | 4 | 25 | 1 | 11.1 | 0.405 |
| 2 | - | - | - | - | - | |
| Longitudinal striations | 1 | 0 | 0 | 5 | 55.6 | 0.001* |
| 2 | 0 | 0 | 5 | 41.7 | 0.009* | |
Table 4: Dermoscopic nail findings in autoimmune bullous diseases according to the age of the patients. Note: p-value was significant if ≤ 0.05; chi-square test was used; fisher exact test was used.
Patients were also grouped according to the duration of the disease into two groups (<1 year and ≥ 1 year). In group 1: Splinter hemorrhage and periungual blister were significantly higher among those with disease duration >1 year (p-value=0.006 and p-value=0.016 respectively). While in group 2 no significant difference was noticed (Figure 7,8 and Table 5).
| Type of AIBD | Duration of disease | p-value | ||||
|---|---|---|---|---|---|---|
| Group | <1year G1: (n=13) G2: (n=12) |
≥1 year G1: (n=12) G2: (n=13 |
||||
| No. | % | No. | % | |||
| Splinter hemorrhage | 1 | 8 | 61.5 | 1 | 8.3 | 0.006* |
| 2 | 8 | 66.7 | 4 | 30.8 | 0.073 | |
| Onycholysis | 1 | 2 | 15.4 | 6 | 50 | 0.064 |
| 2 | 3 | 25 | 3 | 23.1 | 0.91 | |
| Onychomadesis | 1 | 6 | 46.2 | 4 | 33.3 | 0.513 |
| 2 | - | - | - | - | - | |
| Onychomycosis | 1 | 2 | 15.4 | 4 | 33.3 | 0.294 |
| 2 | 2 | 16.7 | 4 | 30.8 | 0.409 | |
| Beau's lines | 1 | 4 | 30.8 | 3 | 25 | 0.748 |
| 2 | 2 | 16.7 | 5 | 38.5 | 0.225 | |
| Onychorrhexis | 1 | 7 | 53.8 | 6 | 50 | 0.848 |
| 2 | - | - | - | - | - | |
| Pitting | 1 | 1 | 7.7 | 2 | 16.7 | 0.49 |
| 2 | - | - | - | - | - | |
| Subungual hemorrhage | 1 | 4 | 30.8 | 1 | 8.3 | 0.161 |
| 2 | - | - | - | - | - | |
| Paronychia | ||||||
| Acute | 1 | 5 | 38.5 | 1 | 8.3 | 0.06 |
| Chronic | 2 | 0 | 0 | 3 | 25 | - |
| Periungual blister | 1 | 5 | 38.5 | 0 | 0 | 0.016 * |
| 2 | - | - | - | - | - | |
| Longitudinal striations | 1 | 4 | 30.8 | 1 | 8.3 | 0.161 |
| 2 | 1 | 8.3 | 4 | 30.8 | 161 | |
Table 5: Dermoscopic nail findings in autoimmune bullous diseases according to the duration of disease. Note: p-value was significant if ≤ 0.05; Chisquare test was used; fisher exact test was used.
Figure 7: Female patient 42 years old with pemphigus vulgaris of 4 year duration, with clinically apparent normal nails. Dermoscopic examination of the thumb of the left hand (dry technique). Note: Blue arrow: Beaus’ lines; Orange arrow: Distal onychomycosis (dlite dermoscope magnification 30X).
Figure 8: Male patient 35 years old with pemphigus vulgaris of 3 year duration, with clinically apparent normal nails. Dermoscopic examination of nails (wet technique). Note: Blue arrow: Distal onycholysis (dlite dermoscope magnification 30X).
Autoimmune blistering disorders are relatively uncommon dermatoses and few literatures have studied their nail changes [1]. They frequently cause nail abnormalities, particularly paronychia and onychomadesis [5]. In the present study, we have examined the nails clinically and dermoscopically of 50 patients with various AIBDs, 25 had clinically affected nails and 25 had clinically apparently free nails and compared them with a healthy control group (n=50). In the present study 88% of patients had dermoscopic nail findings. Splinter hemorrhage was frequently observed both in group 1 and 2 (40% and 48% respectively). Among 26 cases with pemphigus vulgaris, interestingly, splinter hemorrhage was the most frequent dermoscopic feature (30.8% in group 1 and 38.5% in group 2). Also, it was observed in 6 cases with pemphigus foliaceus, 3 cases with bullous pemphigoid and two cases with linear IgA bullous dermatosis and just one case of pemphigoid gestationis. It was higher in patients with disease duration less than 1 year with significant difference in group 1 (p-value=0.006), so it can be considered as an initial dermosopic nail manifestation. It was found in 2 cases of the control group which is mostly traumatic.
Among group 1, 36% had acute and chronic paronychia when examined clinically and dermoscopically. It was reported in 53.8% in those with pemphigus vulgaris, one case with pemphigus foliaceus and another case with pemphigoid gestationis. This is nearly in accordance with Gopal et al. who reported paronychia as the most frequent clinical nail manifestation in 44% (11/25) of patients with pemphigus vulgaris [1]. Howevere, paronychia was not observed subclinically by the dermoscope in group 2. Paronychia occurs as a result of acantholysis of lateral nail fold epidermis [6]. Staphylococcus aureus and Candida albicans have been isolated in acute paronychia due to pemphigus vulgaris [7]. Onychorrhexis was the commonest finding in group 1, seen in 13 (52%) cases clinically and dermoscopically. It is the longitudinal ridging of the nail plate, associated with nail thinning, and indicates defective keratinization of the proximal nail matrix [8]. In the current study, it was a common dermosopic feature reported in pemphigus vulgaris patients with clinically affected nails (46.2%). It was also found in all patients with bullous pemphigoid (n=6) and one case with dermatitis herpetiformis. It was observed more frequently in the age group ≥ 50 years old (p-value<0.001). Gopal et al. reported onychorrhexis clinically in 30% of patients with autoimmune blistering diseases and also had noticed it in the older age group above the age of 45 years with p<0.001 [1].
Onychomadesis was reported only in group 1 of AIBDS cases clinically and dermoscopically (40%). It was observed in 53.8% of cases with pemphigus vulgaris, two cases with bullous pemphigoid and one case with pemphigus foliaceus. Onychomaedesis is the proximal detachment of the nail plate from the nail bed and occurs as a result of a severe underlying inflammatory process that causes complete arrest of nail matrix activity [8]. Benmously et al. reported clinical onychomadesis in 33% of pemphigus vulgaris cases [6]. Clinical onychomadesis was reported as an unusual nail sign in bullous pemphigoid by Benmously-Mlika et al. [9]. We have observed Beau's lines dermoscopically equally in both groups of AIBDS (28%) each and clinically in 6 cases of group 1(24%).
Gopal et al. found clinical Beau’s lines in only 6 cases (15%) of 40 patients with different autoimmune blistering diseases [1]. Beau's lines occur due to the temporary arrest of proximal nail matrix activity leading to the formation of transverse depressions [8]. We have reported it in pemphigus vulgaris in 4 cases with clinically affected nails and subclinically in another 4 cases (30.8%). Also, they were found subclinically in 2 cases with pemphigus foliaceus and one case with linear IgA bullous dermatosis and in 50% of bullous pemphigoid cases of with clinically affected nails.
In our study, distal subungual onychomycosis (confirmed by nail biopsy stained with PAS stain) was reported dermoscopically equally in both groups of AIBDS (24%) each and clinically in 3 cases only of group 1(12%). Tuchinda et al. reported that 24% of patients with vesiculobullous autoimmune disorders, on immunosuppressive therapy, had clinical onychomycosis [10]. Among those with pemphigus vulgaris 38.5% in group 1 and 30.8% in group 2 had onychomycosis. This may be explained by humidity of the periungual area and because our patients are on immunosuppressive treatment making them liable for fungal infection. Distal onycholysis was observed dermoscopically in 32% of group 1cases and in 24% of group 2 cases and it was observed clinically in 24% of group 1. Cao et al. reported clinical onycholysis in 21.5% of patients with different AIBDs [11], while it was seen in three (4%) cases only by the study by Kadu et al. [12]. It is the separation of the nail plate from nail bed [13]. It was seen in 5 patients with pemphigus vulgaris, 2 patients with bullous pemphigoid and one patient with Pemphigus foliaceus with clinically affected nails. It was found subclinically in 3 cases with pemphigus vulgaris, 2 cases with pemphigus foliaceus and one case with linear IgA bullous dermatosis.
Periungual blisters were observed clinically and dermoscopically in 20% in group 1, 4 patients with pemphigus vulgaris and one patient with bullous pemphigoid. Gopal et al. reported this finding clinically in 15% of patients with different AIBDs and all of them had pemphigus vulgaris [1]. Subungual hemorrhage was seen clinically in 16% and dermoscopically in 20% of group 1 only, 4 cases with pemphigus vulgaris and one case with linear IgA bullous dermatosis. This finding was reported clinically in 5 of 64 patients (7.8%) with pemphigus vulgaris by Schlesinger et al. [4] and also reported by Zhu and Wang in two patients with pemphigus vulgaris [14]. Longitudinal striations were reported clinically in 2 cases in group1 and dermoscopically in 20% in each group, one patient with pemphigus vulgaris and 4 cases of bullous pemphigoid with clinically affected nails. It was also observed subclinically in two cases with pemphigus vulgaris and two cases with bullous pemphigoid. This finding was also observed in the same percent in the control group (20%) mostly due to their old age. The least frequently observed nail manifestation dermoscopically was superficial pitting in 6% of all cases, all of them are AIBDS with clinically affected nails. Also, it was also observed in (12%) of the control group and was mostly of traumatic cause.
Clinical and subclinical nail changes in autoimmune bullous diseases can be appreciated well with the help of the dermoscope, so appropriate treatment can be instituted to prevent permanent damage of the nails. To the best of our knowledge, this is the first study to evaluate clinical and subclinical dermoscopic nail findings in patients with AIBD. However, the small sample size, lack of clinical correlation with disease severity and lack of long- term follow-up of patients with clinically invisible nail findings are limitations of this study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Hofny ERM, Hasan MS, Salah Y, Tawfik YM (2024) Dermoscopy of Nails Involvement in Autoimmune Bullous Diseases: A Case-Control Study. J Clin Exp Dermatol Res. 15:666.
Received: 03-May-2024, Manuscript No. JCEDR-24-31120; Editor assigned: 06-May-2024, Pre QC No. JCEDR-24-31120 (PQ); Reviewed: 20-May-2024, QC No. JCEDR-24-31120; Revised: 27-May-2024, Manuscript No. JCEDR-24-31120 (R); Published: 03-Jun-2024 , DOI: 10.35841/2329- 9509.24.15.666
Copyright: © 2024 Hofny ERM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited