Family Medicine & Medical Science Research
Open Access
ISSN: 2327-4972
ISSN: 2327-4972
Research Article - (2021)Volume 10, Issue 5
Background: Sars-COV-2, the virus responsible for COVID-19, has a diverse clinical presentation and course that is amplified across different populations. It intensifies existing health outcome disparities that minorities and individuals in lower socioeconomic groups face when compared to the general population. However, the particular elements among these groups that contribute to health disparities with COVID-19 infections are unclear.
Objective: To examine the relationship between various Social Determinants of Health (SDH) such as ethnicity, financial class, primary language, age and zip code have on the course and progression of COVID-19 infections.
Design: A retrospective cohort analysis of data from patients who tested positive for the coronavirus admitted to the Emanate Health hospital system across all three campuses at Queen of the Valley Hospital, Inter-Community Hospital and Foothill Presbyterian Hospital. We extracted data from the hospital electronic medical records (EMR) and analyzed the following aspects of SDH including zip code, financial class, ethnicity, primary language and age as related to length of stay and mortality rate at Emanate Health.
Participants: Patients (18 years of age or older) admitted to the Emanate Health hospital system in the San Gabriel Valley, California between 3/17/2020-6/30/2020 (n=400) who tested positive for the novel coronavirus via nasopharyngeal, oropharyngeal and/or serologic testing based on availability.
Results: Statistical significance was noted for the SDH parameters of insurance status, primary language and ethnicity with respect to insurance. Medicare patients had the longest average length of stay in contrast to self pay patients with the lowest average days (P <0.0001). Hospital length of stay increased with increasing age when grouped by ages 19-29, ages 30-49, ages 50-69 or ages 70+ (p value <0.0001). English was the primary language of 75.25% of patients but mortality rate was higher for patients whose primary language was Spanish. The average length of stay for Hispanics when classified by financial class was statistically significant (p =0.0002) as well as the average hospital length of stay for Non-Hispanics when classified by financial class (p <0.0001).
Conclusions: The environment in which people are born, live and age is long known to govern a wide degree of health outcomes. Our data specifically highlights the differences in the course of COVID-19 infections amongst people with different social determinants of health and how COVID-19 further unveiled these existing social disparities. We should be cognizant of the large Hispanic/Latino population that’s makes up the San Gabriel Valley and take heed of these particular socioeconomic factors that drive poorer health outcomes.
Poorer health outcomes inflict minorities, especially those in lower socioeconomic groups (defined by income, education, area of residence and occupation), more often when compared to the rest of the population. COVID-19 rapidly swept the globe into a pandemic most of the year 2020 and even more rapidly uncovered the health disparities that exist among different populations in the U.S [1]. The novel coronavirus (SARS-CoV2) responsible for COVID-19 spreads via respiratory transmission from person to person with a wide ranging clinical presentation spanning from asymptomatic transmission to a severe acute respiratory distress syndrome requiring long hospital admissions for supplemental oxygen, mechanical intubation, medical management and sometimes death [2].
The Centers for Disease Control and Prevention state individuals at high risk for serious illness with COVID-19 include older adults and those with underlying medical conditions, primarily cancer, chronic kidney disease, chronic obstructive pulmonary disease, immunocompromised states, obesity with BMI>30, serious heart conditions, sickle cell disease, smoking, pregnancy and type II diabetes (Centers for Disease Control, 2020 [3]). Many of these comorbid conditions are known to disproportionately affect minority populations (Health Disparities by Race and Ethnicity, 2020 [4]). The increased risk of developing and therefore, chronic management of underlying conditions particularly within lower socioeconomic status populations may largely contribute to the inferior health outcomes seen within these groups when compared to others. However, we must also examine how elements such as geography, race, insurance, zip code and healthcare utilization contribute to health outcomes. We analyzed the hospital length of stay and mortality rate with COVID-19 infections within these various factors at our hospital system, Emanate Health, in the East San Gabriel Valley region of Los Angeles County.
In this retrospective cohort study, we analyzed de-identified patient information extracted from the hospital electronic medical records from 3/15/2020-6/30/2020 of all patients (n=400) who were admitted to Emanate Health (at any of the three campuses: Queen of the Valley Hospital, Inter-Community Hospital and Foothill Presbyterian Hospital) with a positive COVID-19 test via SARS-CoV-2 NAAT (nasopharyngeal and/or oropharyngeal, and serological). We carried out a one way analysis of variance (ANOVA) to compare various social determinants of health including zip code, race, ethnicity, financial class and primary language as related to length of stay and mortality with COVID-19.
Patients (ages 18 years or older) admitted to the hospital were grouped into a financial class which included health insurance with Medi-Cal (n=129), Medicare (n=159), capitated insurance (n=12), insured (68), self pay (n=12) or other (n=20). Financial classes in the other group included exclusive provider organization (EPO), CVHP Self-Insured EPO (EPOSI), Other Non-Government (OTC), Other Governmental (OTG), CVHP Self-Insured PPO (PPOSI), and Workers Compensation (WC). The length of stay for these different groups was statistically significant with a p value <0.0001 (Figure 1). The length of stay in the intensive care unit was also statistically significant (p value <0.0001) (Figure 2).
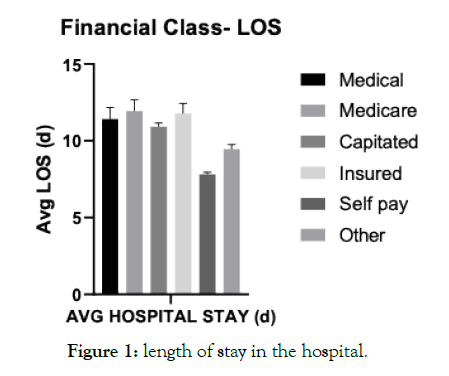
Figure 1. length of stay in the hospital.
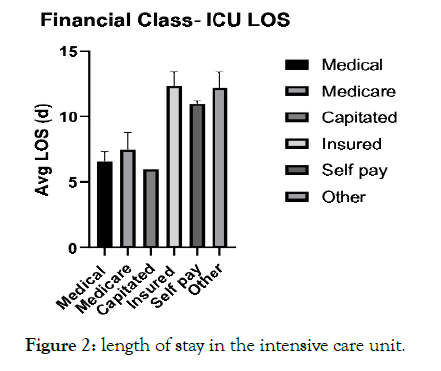
Figure 2. length of stay in the intensive care unit.
Hospital length of stay increased with age when grouped by ages 19-29 (n=16), ages 30-49 (n=78), ages 50-69 (n=189) or ages 70+ (n=117). There was a significance among these groups with a p value <0.0001 (Figure 3).
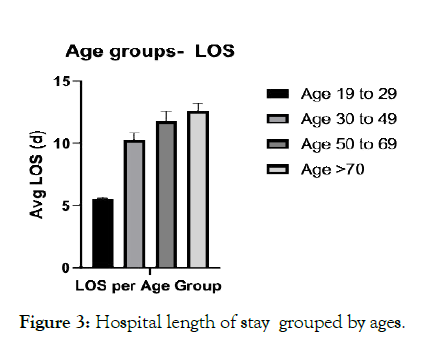
Figure 3. Hospital length of stay grouped by ages.
English was the primary language of 75.25% of patients but mortality rate was higher for patients whose primary language was Spanish (Figure 4). Of patients admitted with COVID-19, the primary language was English for 391 patients, Spanish for 91 patients, and Other (Tagalog, Filipino, Cantonese, Vietnamese) for 8 patients.
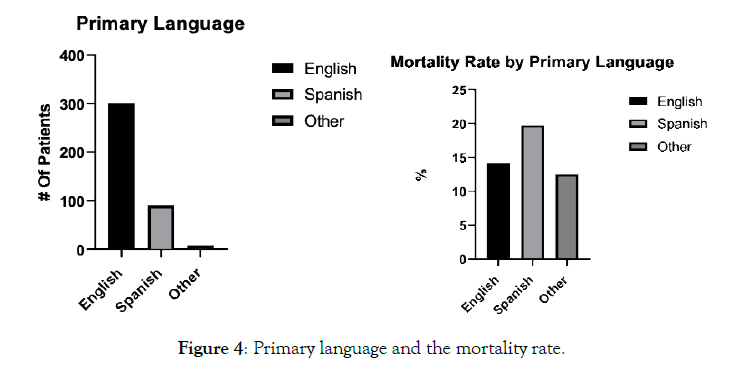
Figure 4. Primary language and the mortality rate.
The average length of stay in the hospital for Hispanics was 11.25 days and 12.05 days for Non-Hispanics (p =0.2473) (Figure 5). The average length of stay for Hispanics when classified by financial class was statistically significant (p =0.0002). Hospital length of stay for Hispanic patients with Medi-Cal was 10.8 days, Medicare 11.7 days, capitated 10.9 days, insured 12.3 days, self pay 7.8 days and other 10.7 days (Figure 6). Hispanics who were insured had the longest average length of stay compared to Non-Hispanics with Medi-Cal who had the longest average length of stay. The average hospital length of stay for Non-Hispanics when classified by financial class was statistically significant (p <0.0001). Hospital length of stay for Non-Hispanic patients was 14.1 days, Medicare 12.4 days, capitated insurance 11 days, insured 10.3 days, other 6.67 days (Figure 7).
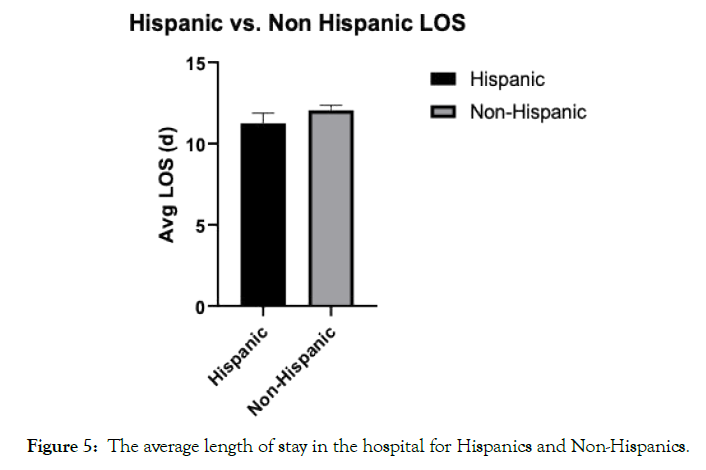
Figure 5. The average length of stay in the hospital for Hispanics and Non-Hispanics.
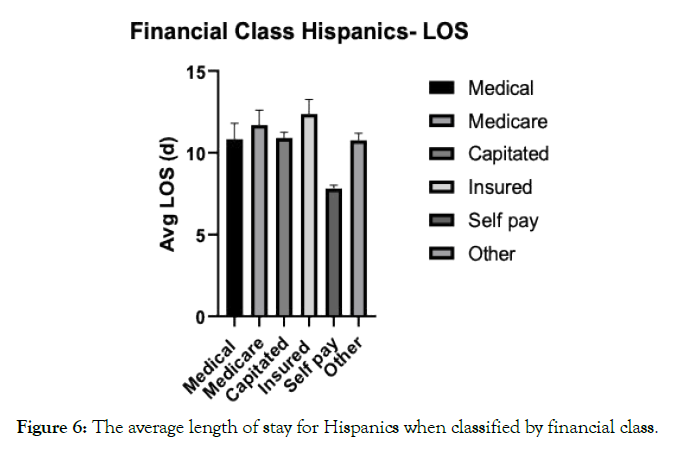
Figure 6. The average length of stay for Hispanics when classified by financial class.
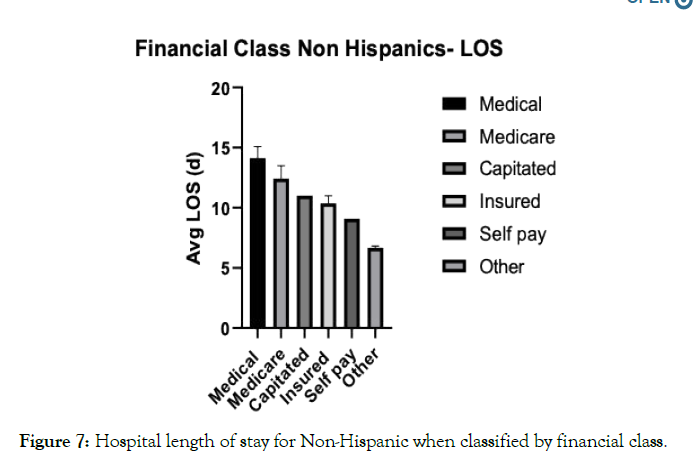
Figure 7. Hospital length of stay for Non-Hispanic when classified by financial class.
Admitted patients were classified into five zip codes in the surrounding area of the three hospitals including Glendora (zip codes 91740/91741), Azusa (zip code 91702), Covina (zip codes 91724/91723/91722), West Covina (zip codes 91790/91791/91792), Baldwin Park (zip code 91706) and other (addresses in other cities in California or homeless patients). Glendora zip code admissions had a n=31, Azusa zip code admissions had a n=51, Covina zip code admissions had a n=45, West Covina zip code admissions had a n=54, Baldwin Park admission zip codes had a n=62 and other zip codes had a n=157.
The environment in which people are born, live and age governs a wide degree of subsequent health outcomes. In 2019, The United States Census Bureau noted Hispanics/Latinos comprise 18.5% of the nation’s population and African Americans comprise 13.4% of the nation’s population in comparison to Caucasians making up 76.3% of the population. Data from the American Public Media research lab through July 22, 2020 showed that Latinos are 2.5 times as likely to die from COVID-19 across the country when adjusted for age (APM Research Lab, 2021 [5]). California is 39.3% Latino, but Latinos make up 54.9% of COVID-19 cases in the state and 46.1% of deaths as of January 20, 2021(California Department of Public Health, 2021). This is in comparison to Caucasians who constitute 38% of the state’s population, 19.8% of cases and 31.9% of deaths. Given the large 4,200 square mile range of Los Angeles County, the county is divided into 8 Service Planning Areas (SPAs) for targeted health services by the Department of Public Health. San Gabriel Valley is designated SPA 3, comprised of 46.3% Latino, 21.2% White, 28.6% Asian and 3.7% African American (Key Indicators of Health, 2017 [6]).
Emanate Health is the largest nonprofit health care provider for residents of the East San Gabriel Valley, which has 903,864 residents (8.8% of the LA county population [7]), through their three campuses at Queen of the Valley Hospital in West Covina, Inter-Community Hospital in Covina and Foothill Presbyterian Hospital in Glendora. Emanate Health serves a demographic that is 54.9% Hispanic/Latino, 25.2% Asian, 15.7% White and 32% living below 200% of the federal poverty level (Community Health Needs Assessment Report, 2019 [8]). In our study, admissions were higher for patients from Baldwin Park and West Covina compared to Glendora. Baldwin Park is made up of 74.5% Hispanic, 19.2% Asian and 3.9% White and the median household income is $65,904 (California Demographics, 2020 [9]). West Covina is made up of 53% Hispanic, 28.6% Asian and 11.5% White with a median household income of $82,938. Glendora is made up of 47.9% Caucasian, 34.4% Hispanic and 11.3% Asian with a median household income of $96,132. These outcomes could be connected to our significant results of Hispanic and Non- Hispanic patients’ length of stay in relation to financial class. Ultimately, people are likely to have a combination of several social factors that leads to the varying outcomes seen within the healthcare system.
In 2017, 7.1% of the population in San Gabriel Valley was diagnosed with heart disease, higher when compared to LA County (6.6%) and California overall (6.6%). Additionally, 9.3% of the population was diagnosed with type II diabetes in 2017 compared to 12.1% in LA County; however, more patients (3.7%) were hospitalized with uncontrolled diabetes when compared to LA County (3.4%). Uncontrolled diabetes exacerbating the pathophysiologic effects of COVID-19 infections in these patients may be a potential contributor, given the compared higher admission rate with uncontrolled diabetes and lower diagnosis rate of diabetes. This may be due to decreased healthcare utilization and access, preventative/ healthy behaviors and linguistic barriers. Access to primary care was reported in 4.8% of the San Gabriel Valley population, compared to 5.7% in LA County (Community Health Needs Assessment Report, 2019). San Gabriel Valley reported slightly less access to healthy foods compared to LA County. These differences cannot be discounted when considering that the course of certain chronic conditions such as type II diabetes is largely influenced by the access to education on dietary choices and medical therapy for long term blood glucose regulation; much of which is attained through access to a medical provider. Furthermore, a study done in 2018 showed that minorities (including Asians, African Americans and Hispanics) all had increased odds of undiagnosed diabetes and less access to healthcare compared to Caucasians (Kim, Racial and Ethnic Disparities in Diagnosis of Chronic Medical Conditions in the USA, 2018 [10]).
In our data, most patients spoke English as their primary language but the mortality rate was higher for patients with Spanish as their primary language. Cultural miscommunication and individuals feeling uncomfortable disclosing vulnerable information in the presence of an interpreter pose a threat to the doctor patient relationship and subsequent outcomes in patients whose primary language is not English. In one retrospective chart review study, hospitalized patients who did not speak English were less likely to have documentation of informed consent for common invasive procedures despite on-site professional interpreter services [11]. This health inequality could have been further threatened by the limited resources during the time of this study in the initial months of the COVID-19 pandemic and efforts to limit exposure of health care personnel resulting in decreased use of interpretation services.
Beyond the underlying health conditions disproportionately affecting this population, COVID-19 further amplifies health disparities by nature of the virus being highly transmissible, critical or deadly for some and novel to all immune systems (Coronavirus disease (COVID-19): Similarities and differences with influenza, 2020 [12]). Public health officials ordered sheltering at home as a means to slow the spread of the virus, a mandate which is not a sustainable option for many minorities. Minority groups are more likely to be essential workers and work in service or transportation industries and unable to quarantine at home (US Bureau of Labor Statistics, 2019 [13]). In the US, the Hispanic population makes up 21% of essential workers, with 28% of the food/agriculture industry and 40% of industrial/commercial facilities. An additional notable cause of social determinants is the challenge of being unable to adequately physically distance when in close living arrangements that causes health inequality. The average household size for Hispanics is 3.1 people compared to an average household size of 2.4 people for Caucasians (Beyond the Numbers, 2017).
When assessing the various financial classes, patients with Medicare had a longer average length of stay. This can be attributed to the complexity seen in the cases of patients who are ages 65+ or have kidney disease as they are more likely to be immunocompromised and have more comorbidities that require medical attention compared to the general population. Self pay patients had a lower average length of stay. Some consideration should be made that doctors are encouraged to prepare safe discharge plans for these patients quickly given the rising costs of all elements involved in a hospital stay. In one study that controlled for comorbidities, age, sex, race/ethnicity; patients without insurance had significantly shorter hospital length of stay compared to patients with either private insurance or Medicaid [14]. Increased age was associated with an increased average length of stay, a finding that is reasonable given the likelihood of medical comorbidities increases with age. However, a large portion of this population has Medicare benefits which poses challenges to minorities who are unable to afford out of pocket or additional expenses that may not be covered such as prescription drugs, dental care and long-term care (RA, 2004).
Our study limitations include a smaller sample size for some of the evaluated factors including patients with capitated insurance making up 12 of the total 400 patients from the study. Due to the multitude of zip codes for patients admitted to the Emanate Health hospital, only several of the zip codes immediately surrounding our hospitals were selected for statistical analysis. Moreover, the study sample represents an approximate three month period at the start of the COVID-19 pandemic which may not be a full representation of the population demographics affected by COVID-19 after this time period. Our hospital demographics were mostly Hispanic, which can skew some of the percentages and statistics. Data was extracted from the hospital electronic medical record and subsequently limited to accuracy of the information that was input.
As a country, we have a myriad of access to research, technology and pharmacotherapies in comparison to many other parts of the world but continue to have the highest health care costs among developed countries. COVID-19 further exposed the gaps in health quality among different socioeconomic groups. Until we address the social inequalities that are accelerating such varying health outcomes, increasing costs and ethical concerns will continue to threaten our health care system.
Linda Waddell, Stella Hua
Citation: Barati P, Chen-Joea C, Shalikar H, Martin C, Velasquez J, Lascala N, et al. (2021) Detrimental Impact of Social Determinants of Health on Hospitalized Patients with COVID-19. Fam Med Med Sci Res 10:5, doi: 10.35248/2327-4972.21.10.276.
Received: 05-Mar-2021 Accepted: 24-May-2021 Published: 31-May-2021 , DOI: 10.35248/2327-4972.21.10.276
Copyright: © 2021 Barati P, et al. This is an open access article distributed under the term of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.