Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2024)Volume 15, Issue 3
Objective: This study aimed to evaluate the diagnostic accuracy of dermoscopy in patients with some hypopigmented lesions.
Material and methods: 150 patients with hypopigmented skin lesions were included in the study, of which 22 were excluded due to previous treatments. Finally, 128 patients with hypopigmented skin lesions and a possible diagnosis of cutaneous discoid lupus erythematosus, morphea, extragenital lichen sclerosis, and idiopathic guttate hypomelanosis were biopsied after dermoscopic examination to confirm the diagnosis.
Results: The patients evaluated were as follows: Discoid lupus erythematosus (19 cases), morphea (25 cases), extragenital lichen sclerosis (4 cases), and idiopathic guttate hypomelanosis (13 cases) and 67 other diagnoses as control groups were considered separately to compare dermoscopic parameters in each group. The most common dermoscopic findings in discoid lupus erythematosus were telangiectatic vessels in 68.4% of patients. The sensitivity and specificity of dermoscopy in diagnosing were 94.7% and 35.5%, respectively. The most common findings in morphea were white fibrotic beams in 56% of patients. The sensitivity and specificity of dermoscopy in diagnosing morphea, considering only one variable, were 100% and 33%, respectively. The most common finding in extragenital lichen sclerosis was bright white-yellowish plaque in 100% of cases. The most common finding of idiopathic guttate hypomelanosis was nebuloid pattern in 69.2% of patients. The sensitivity and specificity of dermoscopy in diagnosing idiopathic guttate hypomelanosis were 100% and 38.7%, respectively.
Conclusion: The results of this study show that dermoscopy has high sensitivity and low specificity in patients with hypopigmented lesions.
Diagnostic accuracy; Dermoscopy; Hypopigmented lesions; Discoid lupus erythematosus; Morphea; Extragenital lichen sclerosus; Idiopathic guttate hypomelanosis
Hypopigmented lesions are amongst the most frequent complaints in dermatology patients. These lesions are commonly observed in children and adults, with a prevalence of at least 1 in 20 individuals. The prevalence of various hypomelanotic lesions depends on patient characteristics, geography, family history, and exposure to environmental factors [1]. Some of the important macular hypopigmented skin lesions include vitiligo, pityriasis alba, Lichen Sclerosis Atrophicus (LSA), achromic pityriasis versicolor, Idiopathic Guttate Hypomelanosis (IGH), nevus depigmentosis, morphea and Discoid Lupus Erythematosis (DLE) [2]. Diagnosis of these skin lesions, like many others, is primarily based on visual findings. Dermatologists often face situations where the possibility of multiple diagnoses can be challenging and require further steps to validate the diagnosis. Techniques commonly used for diagnosis may be invasive, semi-invasive, and non-invasive [3].
Dermoscopy or skin surface microscopy, or epiluminescence microscopy is a non-invasive technique that uses radiant light and Emerson oil to expose the superficial layers of the skin and structures close to the skin surface [4]. Although skin biopsy is the gold standard [5], but in cases where a definite diagnosis is made by dermoscopy, invasive procedures would be unnecessary [6]. Due to the nature of hypopigmented diseases and the aesthetic, psychological, economic, and social effects, especially on people with darker skin types, early diagnosis and proper management could be helpful to stop the progression of the disease and to prevent other issues [1]. In this study, we tried to evaluate the diagnostic accuracy of dermoscopy by changing brightness in some hypopigmented lesions compared to histopathology.
Study design and participants
This prospective study was conducted at dermatology clinic. All patients admitted to the dermatology clinic with a complaint of hypopigmented skin lesions from 2019 to 2020 were enrolled in this study. Inclusion criteria were age over two years, having at least one hypopigmented lesion, and informed consent to enter the study. The exclusion criteria were the treatment of lesions over the last three months. Patients had the right to refuse to enter the study, and not participating did not interfere with their treatment and care. The names and information of patients remained confidential. Patients did not incur any new costs. The risk of infection among patients, especially by contact dermoscopy, was minimized by disinfecting the lenses with isopropyl alcohol before and after each patient examination [7,8].
Test methods
Patients with hypopigmented skin lesions who met the inclusion criteria after obtaining informed consent were examined under dermoscopy. Lesions were evaluated with a HEINE NC2 dermatoscope made in Germany. Imaging was taken from dermoscopy of patients with iPhone SE 2020. The brightness of the images was changed by Fusion [2,9,3], software since intense light makes some diagnostic patterns indistinctive, and changing the brightness would improve the quality of the observed patterns, especially in hypopigmented lesions. Dermoscopic and demographic findings of patients were included in the pre-designed checklist. The selection of dermoscopic variables was based on the data available in the previous studies.
All patients with the clinical diagnoses of lichen sclerosus et atrophicus, idiopathic guttate hypomelanosis, discoid lupus erythematosus, or morphea went under incisional biopsy sampling and the pathology findings were examined by an experienced pathologist who was unaware of dermoscopic findings. Dermoscopic findings were then compared with histopathological ones (Figures1-3).
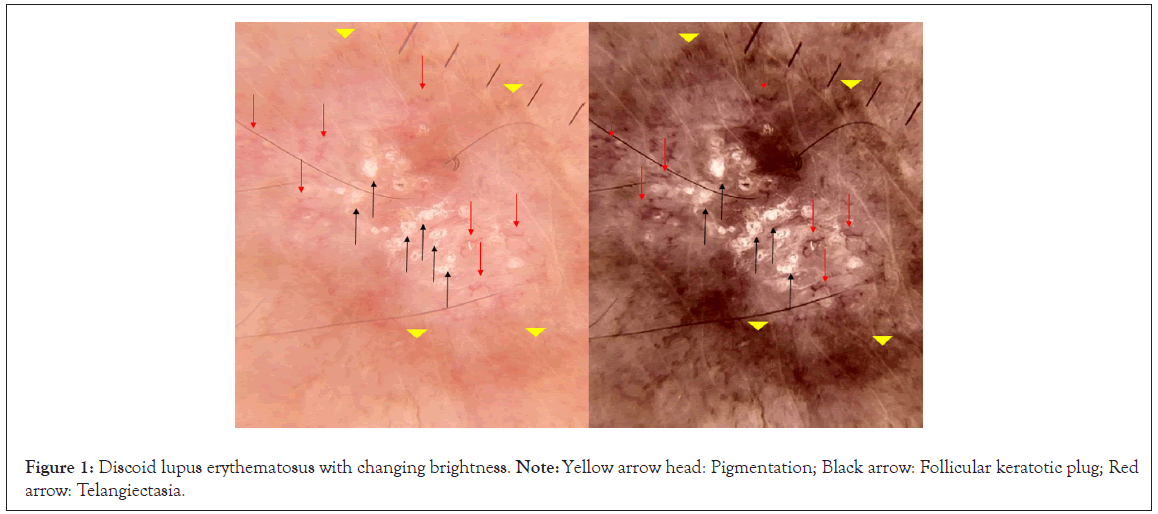
Figure 1: Discoid lupus erythematosus with changing brightness. Note: Yellow arrow head: Pigmentation; Black arrow: Follicular keratotic plug; Red arrow: Telangiectasia.
Figure 2: Discoid lupus erythematosus with changing brightness. Note: White arrow: Pigmentation; Yellow arrow: White scale; Red circle: Structureless whitish area.
Figure 3: Morphea with white fibrotic beams.
Statistical analysis and sample size calculation
Considering the first type error of 5%, the sensitivity rate of 86% and the acceptable error of 0.06% (e=0.07*p), and the 15% sample drop, the required number of samples was equal to 150 patients. For data analysis, we summarized the data using descriptive statistics. In this study, we described our observations using absolute and relative frequencies. In addition, Chi-square was used for assessing categorical variables, and SPSS23 for data analysis, a p-value of <0.05 was considered as the significance level.
150 patients were primarily enrolled in our study, and 22 patients were excluded from the study due to using topical or systemic treatments during the past three months. Among the 128 patients included, 53 (41.4%) were male. 73 patients with skin phenotype 3 (57%), 46 with skin phenotype 4 (35.9%), 6 with skin phenotype 2 (6.4%), and 3 with skin phenotype 5 (2.3%) were distinguished. 19 patients had a definite diagnosis of discoid lupus erythematosus, 25 of morphea, 13 of idiopathic guttate hypomelanosis, 4 of lichen sclerosus et atrophicus, and 67 had other diagnoses (eg. vitiligo, post-inflammatory hypopigmentation and intraepithelial neoplasia) (Table 1).
| Variables | Abundance | Percentage |
|---|---|---|
| Gender | ||
| Female | 75 | 58.60% |
| Male | 53 | 41.40% |
| Skin phenotype | ||
| 2 | 6 | 4.60% |
| 3 | 73 | 57% |
| 4 | 46 | 35.90% |
| 5 | 3 | 2.30% |
| Diagnosis | ||
| DLE | 19 | 14.80% |
| LSA | 25 | 19.55% |
| Morphea | 4 | 3.10% |
| IGH | 13 | 10.10% |
| Other | 67 | 52.30% |
| Total | 128 | 100% |
Table 1: Frequently distribution of gender, skin phenotype, diagnosis.
Dermoscopic findings of discoid lupus erythematous
Among the included patients, 33 had a possible diagnosis of discoid lupus erythematosus and underwent dermoscopy, of which 19 (57.6%) had a definite diagnosis of discoid lupus erythematosus based on pathology. Among the patients with a definite diagnosis, the most common sites of involvement in discoid lupus erythematosus patients were the face (100% of patients), followed by the forearm (21%) and the trunk (10.5%). These patients' most common skin phenotypes were type 3 (42.1%) and type 4 (42.1%). The most common dermoscopic findings in discoid lupus erythematosus patients were, telangiectatic vessels in 13 patients (68.4%), white scales in 11 patients (57.9%), follicular keratotic plug in 6 patients (31.3%), pigmentation in 5 patients (26.3%), structureless whitish areas in 3 patients (15.8%), follicular red dot and perifollicular whitish halo each in one patient (5.3%). Among the dermoscopic variables, follicular keratotic plug was observed in 31.6% of patients in the discoid lupus erythematosus group and none in the control group. This difference was statistically significant between the two groups (p<0.02). From a total of 19 diagnosed patients, 1 patient had no dermoscopic findings (5.3%), 6 patients had 1 parameter (31.6%), 7 patients had 2 parameters (36.8%), 3 patients had 3 parameters (15.8%), and 1 patient had 4 parameters (5.3%) and one patient had all 7 parameters (5.3%) (Table 2).
| Dermoscopic variable | Sensitivity | Specificity | Statistical significance |
|---|---|---|---|
| Telanigectatic vessel | 68.4% | 57.1% | 0.14 |
| White scale | 57.9% | 64.30% | 0.20 |
| Follicular keratotic plug | 31.6% | 100% | 0.02> |
| Pigmentation | 26.3% | 85.7% | 0.4 |
| Structureless whitish area | 15.8% | 100% | 0.11 |
| Follicular red dot | 5.3% | 92.9% | 0.82 |
| Perifollicular whitish halo | 5.3% | 100% | 0.38 |
Table 2: Specifity and sensivity of dermoscopic variables in discoid lupus erythematosus.
Dermoscopic findings of morphea disease
43 patients had a possible diagnosis of morphea, of which 25 patients had a definite diagnosis of morphea, and 18 patients had other diagnoses. Among the patients with a definite diagnosis, in terms of phenotype, 16 patients (64.0%) had skin phenotype 3,7, (28.0%) had skin phenotype 4, and 2 patients (8%) had skin phenotype 2. The most common sites of involvement in the morphea group were the trunk (72% of patients), followed by the forearm (28% of patients), and the most common dermoscopic findings in this group were white fibrotic beam (56%), linear irregular vessel (41.7%), brownish dot (40%), and structureless brownish area (36%). Among these variables, white fibrotic beam and linear irregular vessel were observed only in 4 (22.2%) and 2 (11.1%) patients from the control group, respectively. This difference was statistically significant between the two groups (p<0.05). From a total of 25 patients with a definite diagnosis of morphea, 8 patients had one finding, 6 patients had two findings, 7 patients had three findings, 2 patients had four and 2 patients had five dermoscopic variables (Table 3).
| Dermoscopic variables | Sensitivity | Specificity | Statistical significance |
|---|---|---|---|
| Erythematous areas | 28% | 83.3% | 0.38 |
| Linear branching vessels | 16% | 88.9% | 0.64 |
| Linear irregular vessels | 41.7% | 88.9% | 0.03 |
| Dotted vessels | 8% | 77.8% | 0.184 |
| Comma-like vessels | 0% | 100% | - |
| Hairpin vessels | 0% | 100% | - |
| White fibrotic beams/white clouds | 56% | 77.8% | 0.02 |
| Crystalline structures | 0% | 100% | - |
| Bright white/white-yellowish patches | 0% | 100% | - |
| Unfocused large purple vessels | 0% | 100% | - |
| Yellowish structureless areas | 0% | 100% | - |
| Yellowish-white keratosis follicular plugs | 0% | 100% | - |
| Comedo-like follicular openings | 0% | 100% | - |
| Structure less brownish areas | 36% | 88.9% | 0.06 |
| Reticular brownish areas | 12% | 88.9% | 0.9 |
| Brownish dots | 40% | 66.7% | 0.655 |
| Scaling | 0% | 100% | - |
| Rainbow effect | 0% | 100% | - |
| Erosions | 0% | 100% | - |
| Hemorrhagic spots | 0% | 100% | - |
Table 3: Specifity and sensivity of dermoscopic variables in morphea disease.
Dermoscopic findings in lichen sclerosus et atrophicus disease
In the lichen sclerosus et atrophicus group, 8 people with a possible diagnosis were included in the study, of which 4 had a definite diagnosis of lichen sclerosus et atrophicus. Skin phenotypes prevalence in the definite diagnosis group was as follows, phenotype 3 (75%) and phenotype 4 (25%). The most common dermoscopic finding in the lichen sclerosus et atrophicus group was a bright white-yellowish plaque in 100% of patients, followed by an erythematous plaque in 50% of patients. Out of a total of 4 patients with a definite diagnosis of lichen sclerosus et atrophicus, 2 patients (50%) had 2 variables, one patient (25%) had 3 variables, and one patient (25%) had 4 dermoscopic variables (Table 4).
| Dermoscopic variable | Sensitivity | Specificity | Statistical significance |
|---|---|---|---|
| Erythematous areas | 50% | 100% | 0.1 |
| Linear branching vessels | 25% | 100% | 0.28 |
| Linear irregular vessels | 25% | 75% | 1 |
| Dotted vessels | 0 | 50% | 0.1 |
| Comma-like vessels | 0% | 100% | - |
| Hairpin vessels | 0% | 100% | - |
| White fibrotic beams/white clouds | 0 | 100% | - |
| Crystalline structures | 0% | 100% | - |
| Bright white/white-yellowish patches | 100% | 75% | 0.02 |
| Unfocused large purple vessels | 0% | 100% | - |
| Yellowish structureless areas | 0% | 100% | - |
| Yellowish-white keratosis follicular plugs | 25% | 100% | 0.28 |
| Comedo-like follicular openings | 0% | 100% | - |
| Structureless brownish areas | 0% | 100% | - |
| Brownish dots | 0% | 100% | - |
| Scaling | 0% | 100% | - |
| Rainbow effect | 0% | 100% | - |
| Erosions | 0% | 100% | - |
| Hemorrhagic spots | 0% | 100% | - |
Table 4: Specifity and sensivity of dermoscopic variables in lichen sclerosus atrophicus disease.
Dermoscopic findings in idiopathic guttate hypomelanosis
44 patients with a possible diagnosis of idiopathic guttate hypomelanosis were studied, of which 13 people had a definite diagnosis of idiopathic guttate hypomelanosis. In the group diagnosed based on pathology, seven patients had skin phenotype 2 (53.8%), five patients had phenotype 4 (38.5%), and one patient had phenotype 5 (7.7%). The most common sites of involvement in the group of idiopathic guttate hypomelanosis patients were the forearm (61.5%) and leg (23.1%). The most common dermoscopic finding in the idiopathic guttate hypomelanosis group was the nebuloid pattern in 9 patients (69.2%), followed by the petaloid pattern in 6 patients (46.2%), feathery pattern in 3 patients (23.1%), and ameboid pattern in 1 patient (7.7%). Out of 13 patients with a definite diagnosis of idiopathic guttate hypomelanosis, 7 patients (53.8%) had 1 variable, and 6 patients (46, 2%) had 2 variables (Table 5).
| Dermoscopic variable | Sensitivity | Specificity | Statistical significance |
|---|---|---|---|
| Nebuloid | 69.2% | 38.7% | 0.617 |
| Petaloid | 46.2% | 96.8% | 0.0003> |
| Feathery | 23.1% | 100% | 0.006> |
| Ameboid | 7.7% | 100% | 0.118 |
Table 5: Specifity and sensivity of dermoscopic variables in lichen sclerosus atrophicus disease.
Accuracy
To check the accuracy of the diagnosis, a comparison was made between the group of patients diagnosed with discoid lupus erythematosus and the group who biopsied with the diagnosis of discoid lupus erythematosus, but the pathological diagnosis was not discoid lupus erythematosus as a control group. Out of 19 discoid lupus erythematosus patients diagnosed by pathology, 18 had at least one dermoscopic finding (94.7%), and in the non-patient group, 9 out of 14 patients (64.3%) had at least one dermoscopic finding. The difference between the two groups was statistically significant (p<0.025). In general, dermoscopic sensitivity in discoid lupus erythematosus diagnosis is 94.7% and its specificity is 35.5%. By increasing the number of dermoscopic variables from one to two, sensitivity becomes 63.2%, and specificity reaches 78.6%. In general, dermoscopy had a sensitivity of 100% and a specificity of 33% in diagnosing morphea, considering at least one finding.
Further, the difference in the presence of at least one finding between the two groups was statistically significant (p<0.002). By increasing dermoscopic findings from one to two findings, dermoscopic sensitivity became 68% and specificity reached 72%. Also, the difference between the two groups in terms of the presence of symptoms was statistically significant (p<0.009). Dermoscopy had 100% sensitivity and 25% specificity in diagnosing lichen sclerosus et atrophicus, considering seeing even one variable, but the significance of this finding was not statistically comparable due to the small number of cases between the two groups. By increasing the number of dermoscopic variables from 1 to 2, sensitivity and specificity reached 25% and 75%, respectively. Finally, dermoscopy had 100% sensitivity and 38.7% specificity in the diagnosis of idiopathic guttate hypomelanosis considering at least one variable, and the presence of findings was statistically significant between the idiopathic guttate hypomelanosis and control groups (p<0.009). By increasing the number of dermoscopic variables from one to two, the sensitivity becomes 46.2%, and the specificity reaches 96.8%. The difference between the two groups in terms of the presence of findings was significant (p<0.000).
Johann Saphier first used the term "dermatoscopy". In 1991, Friedman, et al. coined the term dermoscopy for this technique [7]. In the study conducted by Al-Refu, [2], in Jordan, by dermoscopic examination of hypopigmented macular lesions, it was concluded that hypopigmented lesions could have certain characteristics in microscopy, which were non-specific and should be used cautiously with consideration to the clinical condition, patient history, and macroscopic examination. Our findings show that dermoscopy has proper sensitivity and specificity regarding hypopigmented lesions.
Discoid Lupus Erythematosus (DLE) is the most frequent subtype of cutaneous lupus erythematosus. In the study by Lallas, et al. [8], which was conducted as a multicenter study in Italy, Greece, and Serbia, the dermoscopic findings of discoid lupus erythematosus were white peri-follicular halo (69.1%), follicular keratotic plaque (67.3%) and telangiectasia (52.7%) (Figure 4). In this study, the most common dermoscopic findings were telangiectatic vessels (68.4%), white scales (57.9%), and follicular keratotic plaque (31.3%). In our study, the least frequent finding in discoid lupus erythematosus patients was peri-follicular white halo (5%). This low frequency may be due to the smaller sample size or limiting the sample to patients with hypopigmented lesions only. In the mentioned study, the peri-follicular white halo was developed in early lesions, and was completely similar to peri-follicular fibrosis observed in the histopathological examination, while the areas without white structures were observed in late and advanced lesions, which corresponded to diffuse fibrosis in the papillary dermis [8]. In the present study, the relation between histopathological parameters and dermoscopic findings, and also the duration of lesions' existence, were not investigated, and the pathological findings were limited to the correct or incorrect diagnosis of discoid lupus erythematosus. In a study by Fathy H, et al. [9], conducted in Egypt, discoid lupus erythematosus suspected lesions were examined in both scalp and non-scalp areas. Most frequent dermoscopic findings were whitish scales (89.3%), arborizing blood vessels (85.7%), follicular plugging (82.1%) and pigmentation (82.1%) [9]. In this study, the samples were limited to extra-scalp hypopigmented lesions and, the sensitivity and specificity of dermoscopy considering the presence of even one dermoscopic variable in hypopigmented discoid lupus erythematosus lesions were 94.7% and 35.5%, respectively, which had not been investigated in other studies.
Figure 4: Discoid lupus erythematosus with changing brightness. Note: Red arrow: Follicular red dot.
Morphea and cutaneous lichen sclerosus are two common sclerotic/ scleroatrophic inflammatory dermatoses (Figures 5 and 6).
Figure 5: Morphea with changing brightness Note: Green arrow: White fibrotic beams; White circle: Structureless brownish area; Base: Erythematous area.
Figure 6: Morphea with changing brightness Note: Black arrow: White fibrotic beams; Yellow arrow head: Structureless brownish area.
Their clinical manifestations are different based on the stage of the disease; they are characterized by inflammatory patches in the active phase that gradually develops central sclerosis or scleroatrophy (in cutaneous lichen sclerosis). The late stages are characterized by atrophic lesions with or without hypopigmentation or hyperpigmentation and loss of hair follicles/sweat glands. In a study by Errichetti, et al. [10], which was carried out to compare the dermoscopic findings of morphea with lichen sclerosis outside the genitalia, the dermoscopic findings of lichen sclerosis were white fibrotic beam (66.7% sensitivity and 100% specificity). In the current study, the highest sensitivity was related to the white fibrotic beam pattern (56% sensitivity and 77.8% specificity), which was also statistically significant (p<0.02). The lower specificity in the present study could be due to the difference in the selection of the case and control groups; in Errichetti, et al. [10] study, the control group consisted of lichen sclerosus et atrophicus patients, while in the present study, the patients who entered the study with a possible diagnosis of morphea but different pathology, had been considered as the control group. In the later study, the most reliable finding for the diagnosis of extra-genital cutaneous lichen sclerosus et atrophicus was the white, white-yellow patch (sensitivity 88.6% and 100% specificity) and white-yellow keratotic follicular plaque (88.6% sensitivity and 100% specificity) [10]. The findings of this study were in line with the results of our study, but due to the small number of samples, it wasn't possible to check the sensitivity and specificity accurately. In the mentioned study, the trunk was the most common site of involvement in morphea and extragenital lichen sclerosis [10]. In our study, the trunk was also the most common site of involvement, with 72% in morphea and 100% in lichen sclerosus et atrophicus. The average duration of lesions in the morphea group was 7.7 months and in the lichen sclerosus et atrophicus group was 4.1 months [10]. In the present study, considering 5 cases of missing data in the morphea group and 1 case in the lichen sclerosus et atrophicus group due to recall bias, this period is 15.25 months and 16 months, respectively.
Idiopathic guttate hypomelanosis is a common leukodermic dermatosis that commonly affects the elderly population. The disorder is clinically characterized by multiple, round to oval hypopigmented spots that are colorless white and usually have 0.2 to 2 cm diameter [11], (Figure 7).
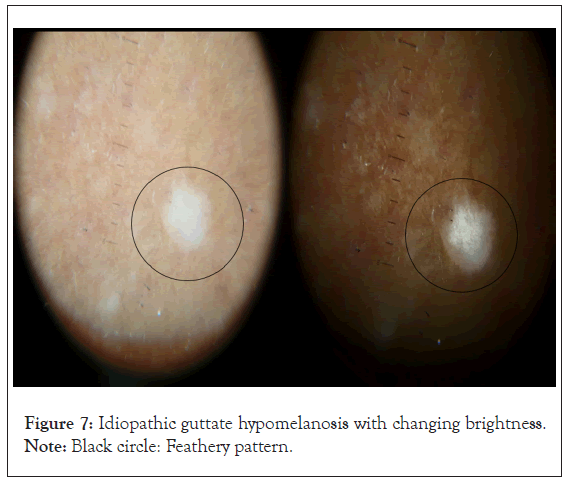
Figure 7: Idiopathic guttate hypomelanosis with changing brightness. Note: Black circle: Feathery pattern.
In a study by Ankad, et al. [12], the author examined lesions with a suspicion of idiopathic guttate hypomelanosis. Their diagnosis was further confirmed by histopathology. Nebuloid, petaloid, feathery, and ameboid patterns were the most frequent in dermoscopy. In this study, unlike the mentioned study, the most common dermoscopic findings were nebuloid, petaloid, feathery and ameboid patterns, respectively, but only petaloid and feathery patterns were significantly different between the idiopathic guttate hypomelanosis and the control group. The petaloid pattern’s sensitivity and specificity were 46.2% and 96.8%, respectively, and the feathery pattern’s sensitivity and specificity were 23.1% and 100%. These findings have not been investigated in other studies. Al-Refu K, et al. [2], investigated hypopigmented lesions using dermoscopy, and the dominant finding in all cases was numerous shiny white porcelain macules with distinct and indistinct borders. This finding was in line with the findings of this study. In the study by Harish, et al. [13], the most common dermoscopic findings in 100 examined patients were ameboid (58.2%), feathery (19.1%), petaloid (14.5%), and nebuloid (8.2%) patterns [13]. This was contrary to the findings of our study and could be due to the small sample size or interpretive bias caused by a lack of the correct dermoscopic terminology standards for hypopigmented lesions (Figure 8).
Figure 8: lichen sclerosus et atrophicus bright white patch with changing brightness Note: Red arrow: Linear branching vessel.
This study concluded that, first, due to the small number of samples in extragenital lichen sclerosus, it was impossible to carry out a detailed statistical analysis, so it is recommended that studies on this disease be multicenter in the future. Second, considering that changing the brightness of the dermoscopic image in order to have a better view of the dermoscopic patterns was the first time in the studies, it is felt that there isn't a standard index to compare with other studies, and it is recommended to conduct more studies by changing the brightness of images that have been taken.
Funding statement
None.
Conflict of interests
All authors declare that they have no conflict of interests.
[PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Gholizadehfard N, Sobhan M, Roshanaei G, Alirezaei P, Maroufi SP (2024) Diagnostic Accuracy of Dermoscopy in some Hypopigmented Lesions on Patients Referred to the Farshchian (Sina) Hospital. J Clin Exp Dermatol Res. 14:663.
Received: 01-Apr-2024, Manuscript No. JCEDR-23-30757; Editor assigned: 05-Apr-2024, Pre QC No. JCEDR-23-30757 (PQ); Reviewed: 19-Apr-2024, QC No. JCEDR-23-30757; Revised: 26-Apr-2024, Manuscript No. JCEDR-23-30757 (R); Published: 03-May-2024 , DOI: 10.35841/2329-9509.24.15.663
Copyright: © 2024 Gholizadehfard N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.