Journal of Bone Research
Open Access
ISSN: 2572-4916
ISSN: 2572-4916
Case Report - (2023)Volume 11, Issue 4
A systemic, musculoskeletal, non-inflammatory disorder, Diffuse Idiopathic Skeletal Hyperostosis (DISH), is characterized by ossification of various ligaments and enthuses. Most commonly it is prevalent in the elderly population, who are over the age of 50 years. Recent hypotheses suggest ossification of the anterior longitudinal ligament to be the most common site however, the pathophysiological mechanism is unclear. In this article, we discuss the case of a 58 years old gentleman who presented with restricted movements associated with pain in the neck and left shoulder and the comorbid condition of hypoparathyroidism with basal ganglia calcification. With a detailed clinical examination, investigations and inter disciplinary approach, a diagnosis of DISH was made. DISH, also referred to as forester’s disease, is a rare entity that mainly manifests as back pain along with stiffness, resulting in gradual loss of motion. One of the presentations can be dysphagia due to large osteophytes leading to mechanical obstruction. Inter disciplinary treatment approach and surgical excision of osteophytes in these cases lead to excellent results.
Forestier’s disease; Diffuse idiopathic skeletal hyperostosis; Hypoparathyroidism; Basal ganglia calcification
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is a systemic condition with the most prominent clinical feature being gradual ossification of ligaments and entheses. It is said that the presence of bony bridges along the anterolateral spine (minimum of three sites), is the most common presentation. In the year 1950, the case was first reported by Forestier and his student, rotes-Querol, abd termed as “ankylosing hyperostosis”. Based on collective (clinical and radiological) features other names were suggested, like ‘spondylitis deformans’, ‘senile vertebral ankylosing hyperostosis’, ‘spondylitis ossificans ligamentosa’ and ‘spondylosis hyperostotica’. Resnick and Niwayama in 1976 coined the term ‘Diffuse Idiopathic Skeletal Hyperostosis (DISH)’. Otherwise, in recent times based on the aetiology and systemic nature of the disease the term DISH is widely accepted. DISH is more common in males than in females. The global prevalence of DISH varies from 2.9% to 42%, depending on race. Population based research has shown that the overall prevalence rate is between 2.5% and 28.0%, with significant increases in age and gender predisposition being the main reason for the rise in rates. Compared to the black, Asian, and native American communities, the white population may have a higher prevalence of DISH [1-3]. In general population, the incidence of DISH varies between 6% and 12%. The pathogenesis of DISH remains elusive and insights about aetiological factors are not reported in the literature. However, environmental changes with vitamin A and fluoride exposure, polymorphism of HLA genes, and various drugs like acitretin; etretinate; isotretinoin are some factors being reported. But recent theories emphasize the pathologic calcification of spine i.e., anterior longitudinal ligament to be a common feature in the diagnosis of DISH. Here in this article, we discuss a unique case report of DISH which has co-existing features of hypoparathyroidism with basal ganglia calcification [4,5].
A 58 years old male patient visited our center; a private hospital in Cochin, Kerala, India, with a chief complaint of restricted movements associated with pain in the neck and left shoulder. The symptoms were insiduous in onset and gradually progressive over a period of 10 years. It started as mechanical left knee pain with difficulty in movements, including squatting and difficulty in bending the left knee more than the right knee. The patient had difficulty in raising his left hand above the shoulder due to restricted movements of the left shoulder joint. He had restriction of left shoulder elevation beyond 60 degrees. The deep tendon reflex was sluggish in the lower limbs. The patient also had restricted movement of the neck associated with pain. The eye movements, neck muscles, and deep tendon reflexes of the upper limb were normal. He had lost interest in day to day activities. There was normal verbal fluency, bowel or bladder movements and sleep. The patient had no loss of fine balance and no depression.
Suspecting a diagnosis of early Parkinson’s disease, a clinical examination with the Unified Parkinsonian Disease Rating Scale (UPDRS) was conducted, and a score of 13/199 was achieved, ruling out Parkinsonism [6]. The detailed neurological examinations showed the patient was lacking the symptoms of Parkinson’s disease such as loss of balance, tremor, verbal changes, loss of automatic movements, etc. Hence, the Parkinsonism was ruled out effectively [7-9]. The patient was a known case of hypoparathyroidism with basal ganglia calcification for the last 10 years, and she was on regular calcium supplements since then. The patient was advised neck physiotherapy, to continue calcium supplements and skeletal muscle relaxant, baclofen (liofen 10 mg) (Figure 1).
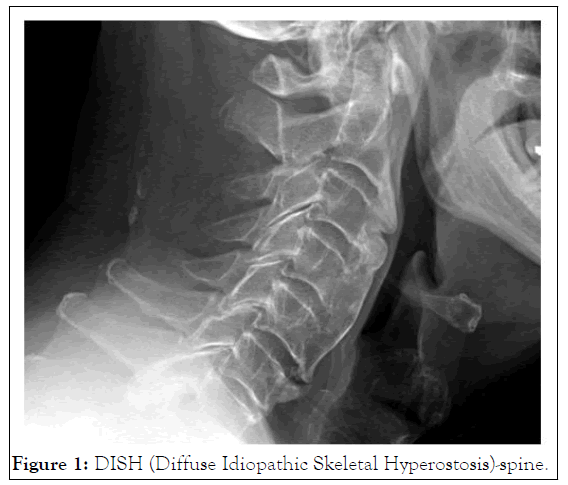
Figure 1: DISH (Diffuse Idiopathic Skeletal Hyperostosis)-spine.
Upon conducting a detailed clinical examination, Schober’s test was found to be positive, associated with restricted neck and hip movements. All the clinical and radiological features were more consistent with DISH than ankylosing spondylitis, since it is a comparatively early-onset condition and there were no classic information [10-13]. Hence, the patient was worked up for radiological investigation. Cervical spine showing flowing ossification over the anterior longitudinal spine anterior longitudinal ligament and marked spondylotic changes; marginal osteophytes predominant on left side at L1-L2 level along with subchondral sclerosis mild subchondral sclerosis in bilateral sacroiliac joints; overcoverage of acetabulum in both hips with lateral center edge angle 660 on the right side and 740 on the left side; (pincer type of femeroacetabular impingement) with the joint space was relatively preserved; significantly narrowing of interphalangeal joint space of both thumbs.
The patient was evaluated for further follow-up in the department of endocrinology. On medical history evaluation, ultrasonography neck showed multiple small well defined solid cystic nodule hyperechoic and spongiform nodules with peripheral hypoechoic halo and vascularity involving both lobes measuring 14 mm × 52 mm in the right lobe with TIRAD score of II and peripherally calcified thyroid nodule 5 mm in right lobe with TIRAD score of III. CT brain showed calcification of bilateral caudate nucleus, lentiform nucleus (predominantly globus pallidus), corona radiata and dentate nucleus. Also, FALX showed patchy calcification/calcified meningioma. Blood serological investigation showed PTH-5.8 pg/ml, Ca-8.28 mg/dl. With these findings, reconfirming the diagnosis of long standing hypoparathyroidism with basal ganglia calcification associated with features of DISH.
Forestier’s disease, DISH, is mainly a non-inflammatory musculoskeletal disorder affecting the entheses by its calcification/ossification. It is a multi-factorial disease but the main cause is unclear. Many internal and external factors have been discussed in the literature. Emphatically, the disease development is associated with obesity, systemic hypertension, type 2 diabetes, up regulation of IGF-1 (Insulin like Growth Factor-1) and hyperuricemia. In several literature studies, elevated levels of vitamin A have also been reported genetic studies in Japan showed polymorphism in the COL6A1 gene (susceptible gene in Ossification of the Posterior Longitudinal Ligament (OPLL) posterior longitudinal ligament). Similarly, altered activity of BMP2 (Bone Morphogenetic Protein 2) and BMP4 mRNA was observed due to increased mechanical stress in OPLL affected patients. It is also reported that decreased levels of Dickkopf-1 (DKK-1) were observed in patients affected with extensive ossified spinal bridges. Elevated levels of PGDF (Platelet Derived Growth Factor) and TGFß1 (Transforming Growth Factor beta 1) in turn which stimulates excess NFkß was observed in DISH. In a few cases, the left side of the thoracic spine was affected by ossification more than right side. This finding postulates that pulsating the right aorta prevents ossification of the enthuses [14-16].
There are varied types of signs and symptoms reported by individuals suffering from the disease. The quality and degree of pain differ among patients depending upon the pathologic ossification sites. These include dysphagia, airway obstruction, and multiple joint pain, especially in the thoracic and lumbar regions. The hallmark of DISH is a pain in the thoracic region due to the ossification of the anterolateral part of the thoracic spine. The ossification of extra-spinal sites and entheses are also noted which include hands, elbows, knees, and pelvis. But most of the DISH diagnosed patients are asymptomatic. It is important to differentiate DISH from osteoarthritis. The elbow, metacarpophalangeal joints, bone cartilage intersection sites, and enthuses ossification sites like quadriceps tendon and calcaneal spur are rarely involved in osteoarthritis. Also, recently had given a diagnostic criterion at an early stage of DISH based on CT findings.
The disease should be differentiated from other common ailments occurring in geriatric population like Ankylosing Spondylosis (AS) and Ossifying Arthritis (OA). DISH and AS share common features like ossification of enthuses and ligaments but the mechanism of ossification differ (inflammatory mechanism in AS). The ossification of sacro iliac joint is not involved in AS. Also, the absence of obliteration of the apophyseal joint, and association of HLA-B27 is not seen in AS. Other diseases include seronegative spondyloarthropathies, charcot’s spine, endocrine disorders like acromegaly, hypoparathyroidism, dermatological disorder (psoriasis), and inflammatory disorders (reactive arthritis). Hypoparathyroidism can lead to ectopic calcification, in which the basal ganglia is a site that in turn leads to slower movements and tremors. In our case, the clinical findings are by these previous reports.
Various therapeutic approaches have been reported in the management of DISH. It is aimed at the prevention of further progression of the disease, mainly in the management of musculoskeletal manifestations of DISH and its comorbidities. Diet modification with low carbohydrates and saturated fat, physiotherapy, increased physical activity and weight reduction is tried as a conservative approach. Local infiltration of corticosteroids, NSAIDs, capsaicin and systemic NSAIDs is tried as a drug delivery approach. In extreme cases, surgical removal of cervical osteophytes can be tried. Patients having comorbidities like systemic hypertension should avoid medications like thiazide diuretics and beta-blockers as these drugs cause insulin resistance [17-19]. They can be safely prescribed with ACE inhibitors, alpha adrenergic antagonists and calcium channel blockers. Surgical approaches namely decompression and stabilization of spine to prevent further progression of disease i.e., to avoid pathological fractures, neurological defects, and lumbar stenosis [20,21].
DISH requires a comprehensive approach with inter disciplinary therapeutic modalities. But the insights into the pathogenesis are elusive. Early diagnosis is required for the prompt treatment of the disease. More prospective and advanced studies are required to elicit a clear mechanism for the disease condition.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Alam TS (2023) Diffuse Idiopathic Skeletal Hyperostosis with Hypoparathyroidism and Basal Ganglia Calcification: A Rare Clinical Entity. J Bone Res. 11:237.
Received: 22-Nov-2022, Manuscript No. BMRJ-22-20321; Editor assigned: 24-Nov-2022, Pre QC No. BMRJ-22-20321 (PQ); Reviewed: 08-Dec-2022, QC No. BMRJ-22-20321; Revised: 27-Mar-2023, Manuscript No. BMRJ-22-20321 (R); Published: 04-Apr-2023 , DOI: 10.35248/2572-4916.23.11.237
Copyright: © 2023 Alam TS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.