Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2022)
Objective: Healthcare institutions must give offer to supply the Personal Protective Equipment (PPE) to medical staff. A variety of skin diseases may result from prolonged contact with this equipment.
Design: The study is shed light on the cutaneous abnormal reactions to the PPE among the medical workers and offers solutions.
Methods: This cross-sectional study involved doctors, dentists, pharmacists, and nurses in the high-risk Ramadi General Teaching Hospital and low-risk Private Clinics, Anbar Governorate, Iraq. Between 4 July till 10 August 2020.
Results: A quantitative descriptive research included age, gender, the duration and type of used masks, gloves, Goggles/face shield, and/or gown. About 23 questions described the adverse skin reactions chiefly that involve the skin. A total of 196 participants were recruited for the online questionnaire, including (49.5%) doctor, (15.3%) dentist, (16.8%) pharmacist, and (18.4%) nurse, with a significant involvement between 20-29 years old age. The use of the mask and glove were associated significantly with an adverse skin reaction, like a wound, dry lips, Acne and/ or folliculitis, hand dryness, erythema, itching, wrinkle, nail fracture. While workers who regularly used gowns had a negative correlation with adverse skin reactions including erythema with pruritus of trunk and shoulders, miliaria and pityriasis versicolor.
Conclusions: PPE may develop mild dermatological adverse effects. This needs early diagnosis and treatment. There are many dermatological advices that may be helpful to avoid these unwanted effects.
Medical staff; PPE; Masks; Adverse effects
Healthcare institutions must offer priority to the gaining and supply of "Personal Protective Equipment" PPE, and arrange for suitable teaching to the medical staff in its use [1,2]. The medical staff must be provided by PPE because of the strength of the infection and the patient's contamination rank is unclear [3]. Health organizations should have measures and strategies that describe the correct order of dress in and take off the PPE in a safe method, after performing hand hygiene, the order for donning the PPE is "a gown, mask, goggles, face shield, and gloves" [4,5]. The continued contact with masks and eye goggles/face shield may cause a variety of dermatological diseases, including contact wheals, pressure wheals, contact dermatitis, and worsening of the previously existing dermatological disease [6]. This skin problem were originally due to the occlusive effect of PPE, maceration, rubbing, epidermal barrier impairment, and contact response, all of which may exacerbate a present cutaneous disease [6,7]. The most frequently reported adverse cutaneous outcomes of extended PPE use were skin inflammation, redness, papules, and scaling, with the most commonly affected sites being the face especially the nose, cheeks, forehead, and hands [8].
A localized facial miliaria and headache were reported secondary to a facial mask [9,10]. The wearing an N95 mask by the medical staff has shown that they complained of pruritus of the face associated with dermatitis or even acne [11]. The most popular unwanted effects of using gloves were dryness of the hands, pruritus, and erythematous rash [12]. The defensive cloth and gown were reported many unwanted cutaneous responses included urticarial, pruritus, and erythematous skin rash [12]. Many studies reported that oral Zinc, Vitamin D3, and Vitamin C were used as prophylaxis against COVID-19 infection by many health care workers [13-15]. With the existing worldwide pandemic, this study designed to high light on the skin unusual responses to the "personal protective equipment" PPE among the medical staff and offers advices as a solutions.
This cross-sectional study conducted for the medical staff that involved doctors, dentists, pharmacists, and nurses in the high-risk Ramadi General Teaching Hospital and low-risk Private Clinics, Between 4 July till 10 August 2020. A self-administered online survey written in English and Arabic completed by all participants. The web-based questioner designed as Google form, containing questions and options were reviewed by a biostatistics expert and two dermatologists, therefore possible misinterpretation, grammar and mistakes were corrected as far as possible. This research was approved by the Ethics Approval Committee, College of Medicine, University of Anbar (Reference no.: 37, Date: 9 August 2020), and a written consent form was obtained from each individual before enrollment into the study, and digital photographs were sent through Gmail.
A thorough quantitative descriptive research included age (that divided in to 5 age groups), gender, and job were documented. All the persons who participated in the study should answer questions contained previous dermatological problems or its clinical features that they had complained before using of PPE (twenty three questions), and the type of skin, whether it is oily, dry or normal (mixed). Also asked about oral drug intake within the last month that which included (general tonics, zinc, vitamin D3, vitamin C, hydroquinone, and antibiotics), besides the use of topical emollient cream or topical sunscreen. The second dimension of the questionnaire for PPE included the type of masks (N95, surgical, clothe), gloves (latex or vinyl), Goggles/face shield, and/or protective clothing (gown). Also reported the duration of using each protective tool per day, besides the duration of days per week during 30 days period. Questions described the adverse skin reactions chiefly that involve the skin of the face, hands, and the trunk.
Statistical analyses
Descriptive analyses were used to study baseline characteristics. The data were analyzed using Microsoft Excel 2010 and SPSS version 22. The hypothesis was tested using Chi-square tests. A P-value<0.05 was considered to represent a significant difference.
A total of 196 participants were recruited for the online questionnaire. Among them, there were 122 (62.2%) males and 74 (37.8%) females. The adverse skin reactions caused by sex had no significant difference (Table 1). Their mean (± SD) age was 34.3 ± 9.3 years (range 23-65 years), and the age was divided into 5 groups, with significant involvement between 20-29 years old age group in (42.8%) of staff (Figure 1). Their occupation, including 97 (49.5%) doctor, 30 (15.3%) dentist, 33 (16.8%) pharmacist, and 36 (18.4%) nurse. In general, the skin texture of participants was 94 (48%) oily, 44 (22.4%) dry and 58 (29.6%) normal (mixed). The reported dermatological diseases within the 3 months before the use of the PPE were seen in 81(39.3%) members, while 115 (60.7%) had not skin diseases.
| Gender | Yes (%) | No (%) | Not use PPE (%) | Total |
|---|---|---|---|---|
| Skin disease of the face after using the mask | ||||
| Male | 74(58.7) | 48(68.6) | 0 | 122 |
| Female | 52(41.3) | 22(31.4) | 0 | 74 |
| Total | 126(64.2) | 70(35.7) | 0 | 196 |
| P-value= 0.173 | ||||
| Skin disease of the hands after using the gloves | ||||
| Male | 49(40.2) | 65(53.3) | 8(6.6) | 122 |
| Female | 42(56.8) | 27(36.5) | 5(6.8) | 74 |
| Total | 91(46.4) | 92(46.9) | 13(6.6) | 196 |
| P-value= 0.064 | ||||
| Skin disease of the body after using the gown | ||||
| Male | 30(63.8) | 52(59.1) | 40(65.6) | 122 |
| Female | 17(36.2) | 36(40.9) | 21(34.4) | 74 |
| Total | 47(23.9) | 88(44.9) | 61(31.1) | 196 |
| P-value= 0.701 | ||||
Table 1: The relation between gender and adverse skin reaction after using PPE.
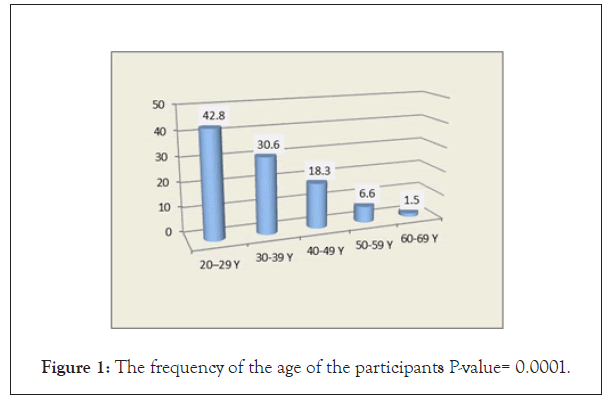
Figure 1: The frequency of the age of the participants P-value= 0.0001.
Protect mouth and nose by face masks
In this study, all the medical staff used a mask, either N95, Surgical mask, Clothe mask, or N95 +surgical mask in (28.1%, 43.4%, 4.6%, and 24.0% respectively) of workers. The duration of using the mask had significant proportion at 3-8 hours/day, and 3-5 days/ week in (67.9%, 46.9% respectively) of staff (Table 2). However, the proportion of the type of masks and the appearance of the adverse skin reaction was not significant, P-value= 0.625 (Table 3). Besides that, the proportion of skin reaction of the face in men was 58.7% and was a significantly higher than that of women's medical staff (41.3%). This study reported that the skin disease of the face affected 42.1% of the doctors and this was significantly higher than the other participated occupations (Table 4). Among the 126 (64.3%) worker who reported adverse reactions of the face, including wound at the attached site of the mask or mask bond (Table 5).
| Hours per day | Mask N=196 | Gloves N=187 | Gown N=138 | Goggles/Face shield N=66 |
|---|---|---|---|---|
| 3hours | 21 (10.7%) | 41 (21.9%) | 28 (20.3%) | 15 (20.3%) |
| 3-8hours | 133 (67.9%) | 115 (61.5%) | 83 (60.1%) | 44 (60.1%) |
| more 8hours | 44 (22.4%) | 31 (16.6%) | 30 (217%) | 15 (20.3%) |
| P-value | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| Days per week | Mask N=196 | Gloves N=187 | Gown N=138 | Goggles/Face shield N=66 |
| ≤ 2 days | 47 (24%) | 45 (24.1%) | Gown N=138 | 28 (37.8%) |
| 3-5 days | 92 (46.9%) | 90 (48.1%) | 60 (43.2%) | 32 (43.2%) |
| 6-7 days | 57 (29.1%) | 52 (27.8%) | 26 (22%) | 14 (18.9%) |
| P-value | 0.0001 | 0 | 0.001 | 0.027 |
Table 2: Frequency of using the mask, gloves, gown, goggle/face shield, and its relation to the time.
| Type of the mask | Skin disease of the face | |||
|---|---|---|---|---|
| No (%) | Yes (%) | No (%) | Total (%) | |
| N95 | 55 (28,1) | 37 (67.3) | 18 (32.7) | 55 (100) |
| Surgical | 85 (43.4) | 57 (67.1) | 28 (32.9) | 85 (100) |
| Clothe | 9 (4.6) | 5 (55.6) | 4 (44.4) | 9 (100) |
| N95 +surgical | 47 (24.0) | 27 (57.4) | 20 (42.6) | 47 (100) |
| Total | 196 (100) | 126 (64.3) | 70 (35.7) | 196 (100) |
| P-value = 0.625 | ||||
Table 3: The relation between the types of masks and adverse skin reactions of the face.
| Adverse skin reaction | Doctor (%) | Dentist (%) | Pharmacist (%) | Nurse (%) | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| Skin disease of the face after using the mask | |||||||||
| Yes | 53 (42.1)* | 20 (15.9) | 22 (17.5) | 31 (24.6) | 126 | ||||
| No | 44 (62.9) | 10 (14.3) | 11 (15.7) | 5 (7.1) | 70 | ||||
| Not use PPE | 0 | 0 | 0 | 0 | 0 | ||||
| Total | 97 (49.5) | 30 (15.3) | 33 (16.8) | 36 (18.4) | 196 | ||||
| P-value=0.009 | |||||||||
| Skin disease of the hands after using the gloves | |||||||||
| Yes | 37 (40.7)* | 6 (6.6) | 18 (19.8) | 30 (33.0) | 91 | ||||
| No | 50 (54.3) | 24 (26.1) | 12 (13.0) | 6 (6.5) | 92 | ||||
| Not use PPE | 10 (76.9) | 0 | 3 (23.1) | 0 | 13 | ||||
| Total | 97 (49.5) | 30 (15.3) | 33 (16.8) | 36 (18.4) | 196 | ||||
| P-value=0.000 | |||||||||
| Skin disease of the body after using the gown | |||||||||
| Yes | 15 (31.9)* | 4 (8.5) | 2 (4.3) | 26 (55.3) | 47 | ||||
| No | 55 (62.5) | 20 (22.7) | 6 (6.8) | 7 (8.0) | 88 | ||||
| Not use PPE | 27 (44.3) | 6 (9.8) | 25 (41.0) | 3 (4.9) | 61 | ||||
| Total | 97 (49.5) | 30 (15.3) | 33 (16.8) | 36(18.4) | 196 | ||||
| P-value=0.000* | |||||||||
Table 4: The relation between the occupation and adverse skin reaction due to using of PPE.
| Dermatological disease | Number | % |
|---|---|---|
| After using the mask N=196 | ||
| The wound at the attached site of the mask or mask bond | 51 | -26 |
| Dry lips | 48 | -24.5 |
| Acne and/or folliculitis (Perioral itchy erythematous papules) | 24 | -12.2 |
| Herpes simplex | 22 | -11.2 |
| Perioral dyspigmentation | 18 | -9.1 |
| Aphthous ulcer | 15 | -7.6 |
| Perioricular erythema, wound, and scale | 15 | -7.6 |
| Pressure hair loss by mask or its bond (scalp, mustache, beard) | 14 | -7.1 |
| Pigmentation where mask attached | 13 | -6.6 |
| After using the gloves N=183 | ||
| Dryness and fissure | 41 | -22 |
| Hand erythema+ itching | 25 | -13.4 |
| Wrinkle | 20 | -10.7 |
| Nail fracture | 17 | -9.1 |
| Pigmentation | 6 | -3.2 |
| Paronychia | 4 | -2.1 |
| Loss pigment | 3 | -1.6 |
| Vesicles | 2 | -1.1 |
| After using the gown N=138 | ||
| Erythema and pruritus of trunk and shoulders | 32 | -23.2 |
| Miliaria | 15 | -10.8 |
| Pityriasis versicolor | 6 | -4.3 |
| After the use of the goggle/face shield, No dermatological diseases | ||
Table 5: The frequency of dermatological diseases after using the mask, gloves, gown, and goggle/ face shield.
Keep clean hands by gloves
Medical care activities require using of a single couple of non-sterile gloves made of either latex or latex-free, Among 183 (93.4%) who often used gloves, 152 (81.2%) of staff used the latex-free glove, and the proportion was significantly more than that who used latex glove that used in 53 (28.2%) of staff. The duration of using of the gloves had significant proportion at 3-8 hours/day, and 3-5 days/ week in (61.5%, 48.1% respectively) of staff (Table 2). Using the latex glove was associated significantly with an adverse skin reaction of the hand in (61.8%) of workers in comparison with that who using the latex free glove (47%). However, there were 46.4% of individuals developed adverse skin reaction after using the glove, and 46.9% of them were not complained of hands skin problems. There was no significant proportion of skin reaction of the hands in both sexes (Table 1). Also, this study reported that the skin disease of the hand affected 40.7% of the doctors and this was significantly higher than the other participated occupations (Table 4). The reported dermatological diseases of the hands after using the gloves were shown in Table 5.
Keep clean skin and cloth gowns
Of the 138(70.4%) of medical staff wore disposable protective clothing, and the duration of using of the gown had significant proportion at 3-8 hours/day, and 3-5 days/week in (61.1%, 43.2% respectively) of staff (Table 2). Among 138(70.4%) of workers who regularly used gowns, 23.9% developed adverse skin reactions of the body and this was statically a significant with negative correlation. The skin reaction of the body in men was 63.8% and was a significantly higher than that of women's participants (36.2%) (Table 1). Also, the skin disease of the body involved 31.9% of the doctors and this was significantly higher than the other medical occupations (Tables 4 and 5).
Goggles/face shield
Of the 74(37.8%) of medical staff used goggles/face shield without any reported adverse skin problems, and the duration of using it ranged between (1 ≥ 8) hours/day, and (1-7) days/week, with a significant proportion at 3-8 hours/day in (60.1%) of staff, and significant proportion at 3-5 days/week in (43.2%) (Table 2).
Discussion
COVID-19 infection is extremely contagious, thus the medical staff must realize the purpose of PPE, such as "masks, gloves, face- shield and protective clothing", and its role as part of a system to reduce disease spread from patients to staff [3,5,16]. Therefore, the workers were developed many adverse skin reactions, and they seek for dermatological advice. For this situation, the author considered studying the dermatological drawbacks that may be caused by the use of PPE to offer solutions, and this will reduce the tension, stress of medical staff, and they will be more active and helpful for their patients. The skin complications among medical staff were primarily due to the occlusive effect of PPE, friction, epidermal barrier impairment, contact reactions, aggravation of existing skin disease [8]. Significant involvement of the young age group between 20-29 years (42.8%), because they consider as the first defense medical line, and this is younger than that reported in other study [12]. The use of emollient cream and sunscreen for the face led to the development of skin disease with a significant negative correlation in (38.8%) of a worker, the exogenous causes like detergents, use of cosmetic products with occlusive dressings may influence the skin pH. Changes in the pH are reported to play a role in the pathogenesis of skin diseases [17]. People have an oily skin texture, and use of bad quality emollient, in addition to that, they are wearing a mask can aggravate the facial skin disease. The present research shows a significant correlation among workers using the mask and adverse skin reaction of the face. This is in agreement with the previous report [8]. However, the effect of the masks' types on skin reaction was not significant, while a series of researchers have found the related adverse responses of health care workers wearing an N95 mask [18]. The skin reaction of the face in men was significantly higher than that of women, and the doctors were more committed and meticulous to wear PPE and affected more than other medical staff. This results unlike that reported in other study [12]. In general, the man has an oily skin texture, hairy skin, careless for their skin, and more distressing in work than the woman. The reported facial skin changes caused by the mask or mask bond in (64.3%) of a worker, including wound at the attached site, dry lips, acne, and/or folliculitis. The occlusion had been reported to induce acne because of the rupture of micro comedones that are not visible to the naked eye [19]. And this is the first work that mentioned the herpes simplex and pressure hair loss of the occipital area is aggravated by the mask. The pruritus occurred due to wearing a mask for a very long time, an extremely humid environment, irritating contact dermatitis to the mask material, or due to the acne or folliculitis.
To decrease adverse skin reactions successfully, the staff should use the salicylic acid soaps for oily skin, topical lubricant for dry texture skin [20] reduce the tightness of the bond of the mask, and add a surgical mask to mark the inside of the N95 mask. Generally, there was no significant correlation between the adverse skin reaction and using the glove. Among (81.2%) of the medical staff prefer the latex-free glove, while (28.2%) used latex glove. However, the adverse skin reaction of the hand was associated significantly with using the latex glove in (61.8%) of workers, and (47%) of individuals using the latex-free glove. A previous study reported that (88.5%) of workers who frequently used latex gloves complained of adverse skin reactions [12]. The most common adverse responses of using gloves in this study were dryness and fissure, hand erythema, itching, wrinkle, nail fracture, pigmentation, paronychia. It was nearly similar to the skin abnormal responses of wearing gloves in previous studies [12,18]. Of course, some reasons led to the emergence of the hands' skin adverse reactions, including hypersensitivity to latex, [21] impair Skin barrier function, [22] and irritant contact dermatitis [23]. So the solution is the use of To decrease adverse skin reactions successfully, the staff should use the salicylic acid soaps for oily skin, topical lubricant for dry texture skin [20] reduce the tightness of the bond of the mask, and add a surgical mask to mark the inside of the N95 mask. Generally, there was no significant correlation between the adverse skin reaction and using the glove. Among (81.2%) of the medical staff prefer the latex-free glove, while (28.2%) used latex glove. However, the adverse skin reaction of the hand was associated significantly with using the latex glove in (61.8%) of workers, and (47%) of individuals using the latex-free glove. A previous study reported that (88.5%) of workers who frequently used latex gloves complained of adverse skin reactions [12]. The most common adverse responses of using gloves in this study were dryness and fissure, hand erythema, itching, wrinkle, nail fracture, pigmentation, paronychia. It was nearly similar to the skin abnormal responses of wearing gloves in previous studies [12,18]. Of course, some reasons led to the emergence of the hands' skin adverse reactions, including hypersensitivity to latex, [21] impair Skin barrier function, [22] and irritant contact dermatitis [23]. So the solution is the use of hypoallergic non-latex glove, and the author prefers with cotton glove wore under the occlusive glove, Dry hands after the wash before wearing gloves. If there is no improvement in the condition, they can add a good quality hands emollients and moisturizers. The adverse skin reactions of the body in (23.9%) workers who regularly used gowns. Males were 63.8% of workers who that significantly higher than females (36.2%). The doctors suffered from body reaction in (31.9%) of medical staff, and usually, they do not seek dermatological advice during the COVID-19 pandemic. These data-less common than that reported in a previous study which found (60.7%) of workers had adverse skin reactions of the body due to wearing a gown, and that the female affected more than male [12]. The logical explanations for the emergence of these cases among medical staff, including skin barrier impairment [22], a mild complaint, or they unworried for their skin, men differ from women, they have profuse sweating, hairy and oily skin texture. To overcome these dermatological problems, the author gave advice, including the regular change of gown, reduce its tightness on the body during employment, use thin cotton clothes with hypo- allergic powder under the gown, and bath with shampoo contains mild antiseptic and anti-fungal for the body a twice/week.
There are many limitations to be recognized. The small impending medical staff employed in the high-hazard areas. Emotional stress and sleep disturbances that could have contributed to the development skin diseases associated with use PPE. Assessment of the temperature of the room and humidity may have predisposed to the skin disease with the use of PPE. The recall bias could affect the self-administered questionnaire.
The skin disease was present but unnoticed by the participant, and may be aggravated by PPE. Lastly, the body mass index, facemask contours, facial hair thickness and the body muscle were not assessed. Younger medical worker (between 20-29 years) uses facial mask, latex gloves may develop mild dermatological adverse effects, it needs early diagnosis and treatment, while the latex-free gloves, gown, and face shield have no significant skin abnormal response. There is medical advice that may be helpful to avoid these unwanted effects.
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
Citation: Alkubaisi TA (2022) Does Personal Protective equipment Lead To Skin Damages? J Clin Exp Dermatol Res. 13:599.
Received: 15-Feb-2022, Manuscript No. JCEDR-22-15856; Editor assigned: 17-Feb-2022, Pre QC No. JCEDR-22-15856 (PQ); Reviewed: 02-Mar-2022, QC No. JCEDR-22-15856; Revised: 07-Mar-2022, Manuscript No. JCEDR-22-15856(R); Published: 14-Mar-2022 , DOI: 10.35248/2155-9554.22.13.599
Copyright: © 2022 Alkubaisi TA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.