Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Research Article - (2019)Volume 8, Issue 4
Background: Type 2 diabetes mellitus is a major public health problem which affects the large number of people worldwide. Diabetes mellitus patients are at high risk of experiencing drug therapy problems due to different factors. Involvement of pharmacists in the management of diabetes mellitus has been shown to reduce the incidence of drug therapy problems.
Objectives: To assess the prevalence of drug therapy problems, pharmacists’ intervention and determinants of drug therapy problems in the management of type 2 diabetes mellitus patients.
Methods: Facility based prospective cross sectional study was conducted among ambulatory type 2 diabetes mellitus patients at Madda Walabu University Goba Referral Hospital from April 1, 2017 to June 30, 2017. Data was analyzed using SPSS version 22. Descriptive statistics was performed to determine the proportion of drug therapy problems and pharmacist acceptance rate. Logistic regressions analysis was performed to identify determinants of drug therapy problems. A p-value of less than 0.05 was considered as statistically significant.
Result: A total of 216 type 2 diabetes mellitus participants were included, of these 52.8% were males. The mean age of study participants was 57.07 ± 13.126 years. Among the study participants, 88% have at least one drug therapy problems. Needs additional drug therapy was the most frequent (50.2%) followed by non-compliance (21.7%). Metformin with glibenclimide and insulin were the most frequently prescribed anti diabetic drugs accounts for 40.3% and 27.8%, respectively. The recommendation done by pharmacists were 94%, the most common intervention done was to add new drug (50.2%). The acceptance rate for the interventions done was 72.6%.
Conclusion: The prevalence of drug therapy problems among type 2 diabetes patients was high. Statin and metformin use not optimized. The involvement of clinical pharmacists in problems intervention should be promoted to decrease drug related risk and increase medication adherence of the diabetic patients.
Diabetes mellitus; Drug related problem; Pharmacist intervention; Determinants
ADA: American Diabetic Association; DM: Diabetes Mellitus; DTP: Drug Therapy Problem; MWUGRH: Madda Walabu University Goba Referal Hospital; SPSS: Statistical Package for the Social Science; T2DM: Type 2 Diabetes Mellitus
Diabetes mellitus is a serious, chronic metabolic disorders that characterized by high sugar level either when the pancreas does not produce enough insulin, or when the body cannot effectively use insulin [1]. Type 2 diabetes mellitus (T2DM) accounts about 90% of all diagnosed cases of diabetes among adults [2].
The prevalence of diabetes mellitus (DM) is 8.8% globally and 7.1% in Africa region among the adult population. It has been gradually increasing for the past three decades and is growing most rapidly in low and middle-income countries [3,4].
The four major groups of antidiabetic agents are: Biguanides which reduce gluconeogenesis in the liver include metformin, Insulin secretagogues which stimulate the pancreas to secrete insulin such as sulfonylureas, Insulin sensitizers which improve sensitivity of peripheral tissues to insulin such as thiazolidinediones and Insulin analogues which provide insulin exogenously [2].
In the absence of contraindication metformin is the first and most widely used pharmacological treatment. It lowers blood sugar levels and help to reduce cardiovascular risk without increased risk of hypoglycaemia and weight gain [5,6].
Cardiovascular risk preventives (statins, antiplatelets) and antihypertensive agents significantly improve the outcome of T2DM. Rennin angiotensin aldosterone system blockers are encouraged to control blood pressure in DM patients with proteinuria or microalbuminuria [7].
Pharmacotherapy has a potential to delay onset of diabetes and its complication, despite these medications are available for the management of diabetes often goal not achieved, because of a failure of to initiate, to stick with a therapy [8].
Drug therapy problem(DTP) is any undesirable event experienced by a patient that involves, or is suspected to involve, drug therapy, and that interferes with achieving the desired goals of therapy and requires professional judgment to resolve [9]. Drug therapy problems(DTPs) may arise at all stages of the medication process from prescription to follow up of the treatment [10].
About fourteen different classifications on DTPs were found published with a different focus. To date there is no consensus and uniform methods of classification of DTPs [11,12]. However, according to Robert J. Cipolle all DTPs can be categorized in to seven types. These are needs additional drug therapy, unnecessary drug therapy, dose too low, ineffective drug therapy, dose too high, adverse drug reaction and non-compliance [13].
Drug therapy problems are significant public health problems worldwide and have been significantly increased over the past few decades [14]. It was estimated that around 5–10% of hospital admissions were due to drug related problems, in which 50% of them are avoidable [15,16]. Approximately 25% of patient’s drug related hospitalizations in Canadian hospital over 70% of these causes were preventable [17]. Each year in Australia, medicationrelated problems account for an estimated 140,000 admissions to hospital annually and an estimated annual economic burden of $380 million [18].
Drug therapy problem in T2DM is one of the factors which affect the outcome of therapy and safety medical care. It is a clinical problem, unless intervention done on the spot of the problems occurrence and it must be identified and resolved in a manner similar to other clinical problems [14]. DTP in diabetes mellitus patients cannot be resolved or prevented unless the cause of the problem is clearly understood [19].
• To assess the prevalence of drug therapy problems among T2DM patients at ambulatory follow up clinic
• To determine clinical pharmacist’s intervention and the acceptance rate among T2DM patients attending ambulatory follow up clinic
• To identify determinants of drug therapy problems among T2DM patients at ambulatory clinic of the hospital.
Hospital based prospective cross sectional study was employed at the outpatient chronic illness follow up clinic in Madda Walabu University Goba Referral Hospital (MWUGRH) from April 1, 2017 to June 30, 2017. A total of 216 T2DM participants were included in the study.
Inclusion criteria
Type 2 diabetes mellitus
Patients who had received at least one antdiabetic drug
Patients who provided informed consent
Patients who were greater than 18 years’ old
Exclusion criteria
Patients with incomplete medical records
Critically ill patients
Study variables
Dependent variable
Drug therapy problems
Independent variable
Socio demographic characteristics, disease related variables, medication related variables
Data collection instrument and procedure
Data was collected by interviewing participants and reviewing patient medical records. Data was collected by two Pharmacists, two Nurses with bachelor degree and one master science in clinical pharmacy. Drug related problems were identified by evaluating the appropriateness of medication orders in terms of indication, dosage, safety and effectiveness. The existence of DTPs was identified using Ethiopian treatment guide line and ADA guidelines of DM treatment [1,20]. The identified DTPs were classified as unnecessary drug therapy, needs additional drug therapy, ineffective drug, dosage too low, adverse drug reaction, dosage too high and noncompliance.
The nurses involved in the vital sign measurement and data collection from the chart. The pharmacists were involved in identification of drug therapy problems and patient counselling for adherence. The master holder clinical pharmacist approved the identified problems and intervention was made by discussion with the responsible physician working in the outpatient clinic. The change made for pharmacist interventions were documented in patient chart.
Data quality management and analysis
The principal investigator had provided training to data collectors. Data was entered into Epi-Data version 4.0.2.101 and exported to the SPSS version 22 (SPSS Inc., Chicago, IL, USA) for analysis. Descriptive statistics was performed to determine the proportion of drug therapy problems by its category. Bivariate and multivariate logistic regression analysis were performed to identify determinants associated with DTPs. Statistical analyses were performed with a p value of less than 0.05 which is considered as significant.
Ethical consideration
Ethical clearance and approval of the study was obtained from Jimma University ethical review board, Institute of Health before starting the actual data collection. Subsequent permission was granted from MWUGRH to access data and interview patients. Each participant was asked to sign a written informed consent before data collection.
Operational definitions
Drug therapy problem: Any undesirable event experienced by a patient which involves, or is suspected to involve, drug therapy, and that interferes with achieving the desired goals of therapy [9].
Polypharmacy: When greater than or equal to 5 drugs are prescribed for the patient [21].
Glycaemic control: Regulation and maintenance blood glucose levels within normal ranges.
Good control: When the average FBS is 70-130 gm/dl, whereas >130 mg/dl is poor [20].
Intervention: When pharmaceutical care plan designed, communicated and the identified problems suggested to be solved
Pharmacist intervention: A recommendation suggested by clinical pharmacist for changing in the patients’ therapeutic management [22].
Accepted: When the suggested problems were recognized and solved.
Intervention accepted but not implemented: When the suggested problems were recognized, but the problems not solved during intervention.
Socio-demographic characteristics of the study participants
A total of 216 participants were included in the study, of these more than half of them (52.8%) were males. The mean age of study participants was 57.07 ± 13.126 years with range of 30-96 years. About 25.9% of patients were overweight. Among the participants 81.5% were married. 29.6% of the participants had no formal education and 22.2% of them were farmers. Equal number of participant (94.9%) not used tobacco as well as not chews chat, but 9.7% of participants were alcohol drinkers (Table 1).
| Socio-demographic characteristics | Variables | Frequency (%) |
|---|---|---|
| Sex | Female | 102(47.2) |
| Male | 114(52.8) | |
| Age | Mean ± SD* | 57.07 ± 13.126 |
| ≤ 44 years | 48(22.2) | |
| 45-59 years | 75(34.7) | |
| ≥ 60 years | 93(43.1) | |
| Body mass index | ≤ 24.9 | 152(70.4) |
| 25-29.9 | 56(25.9) | |
| ≥ 30 | 8(3.7) | |
| Marital status | Married | 176(81.5) |
| Single | 11(5.1) | |
| Divorced | 17(7.9) | |
| Widowed | 12(5.6) | |
| Religion | Orthodox | 134(62) |
| Muslim | 76(35.2) | |
| Protestant | 6(2.8) | |
| Educational status | No formal education | 64(29.6) |
| Grade 1-8 | 87(40.3) | |
| Grade 9 -12 | 27(12.5) | |
| Diploma & above | 38(17.6) | |
| Occupation | Employed | 33(15.3) |
| Merchant | 41(19) | |
| Farmer | 48(22.2) | |
| House wife | 50(23.1) | |
| Retired | 36(16.7) | |
| Tobacco users | - | 11(5.1) |
| Alcohol | - | 21(9.7) |
| Chat chewers | - | 11(5.1) |
| *Standard deviation | ||
Table 1: Socio demographic characteristics of T2DM patients in Madda Walabu University Goba Referral Hospital South-East east Ethiopia,2017.
Disease related characteristics
More than half (63%) of participants had hospital admission and 38.4% had family history of diabetes mellitus. The mean duration of DM was 6.02 ± 4.879 years ranging from 1-27 year. Among participants 67.1% had at least one co-morbid disease. Complication was reported in 20.3% cases. From the participants’ poor glacemic control, uncontrolled blood pressure and dyslipedemia reported in 70.4%, 29.6% and 9.7% patients respectively (Table 2).
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| Admission history since | - | - |
| DM* diagnosis | - | 136(63.0) |
| Family history of DM* | - | 83(38.4) |
| DM duration in year | Mean ± SD | 6.02 ± 4.879 |
| ≤ 4 years | 99(45.8) | |
| 5-9 years | 75(34.7) | |
| ≥ 10 years | 42(19.4) | |
| Number of co-morbidity | One | 43% |
| Two | 21 | |
| Three | 3 | |
| ≥ four | 1 | |
| No co-morbidity | 32 | |
| Type of co-morbidity | 145(67.1) | |
| Hypertension | 120(82.8) | |
| Asthma | 15(10.3) | |
| Dyspepsia | 22(15.6) | |
| Dyslipidemia | 22(15.6) | |
| Heart failure | 23(15.7) | |
| Other** | 9(6.2) | |
| Complication | 45(20.3) | |
| Neuropathy | 25(55.6) | |
| Retinopathy | 10(22.2) | |
| Nephropathy | 10(22.2) | |
| Other*** | 5(11.1) | |
| Average FBS¥ | ≤ 130gm/dl | 64(29.6) |
| >130gm/dl | 152(70.4) | |
| Blood pressure | <140/90 mmHg | 152(70.4) |
| ≥ 140/90 mmHg | 64(29.6) | |
| Lipid control | Normal | 105(48.6) |
| Dyslipidaemia | 21(9.7) | |
| Not available | 90(41.7) | |
| Renal function test | Normal | 151(69.9) |
| Impaired | 12(5.6) | |
| Not available | 53(24.5) | |
| Liver function test | Normal | 37(17.1) |
| Impaired | 11(.5) | |
| Not available | 178(82.4) |
Table 2: Disease related variables among T2DM patients in Madda Walabu University Goba Referral Hospital South-East East Ethiopia, 2017.
Medication related characteristics
Among the participants, 25% had taken two medications and 24.5% participants received single medication. Of the total participants 24.1% taking more than or equal to five medications per day, the mean number of medication was 2.89 ± 1.6 and ranging from one to seven medications. Metformin with Glibenclamide were the most frequently prescribed antidiabetic medication (40.3%), insulin was the most frequent prescribed (27.8%) single medication. Out of patients received antihypertensive medication, 53.1% of them had on enalapril. Of the total participants 36% had received lipid lowering medication, simvastatin was the commonly prescribed lipid lowering medication (83.3%) and 35.6% patients received aspirin as antiplatelet. Among concurrently prescribed medications other than anti-diabetics, antihypertensive, statin and antiplatelet, GIT drugs were 21.4 % (Table 3).
| Variables | Characteristics | Frequency (%) |
|---|---|---|
| Medication taken/day | Mean ± SD | 2.89 ± 1.600 |
| <Five | 164(75.9) | |
| ≥ Five | 52(24.1) | |
| Doses taken per day | Mean ± SD | 1.92 ± 423 |
| Antidiabetics | Metformin | 42(19.4) |
| Insulin | 60(27.8) | |
| Glibenclamide | 18(8.3) | |
| Metformin + Glibenclamide | 87(40.3) | |
| Insulin + Metformin | 7(3.2) | |
| Metformin + Glibenclamide + insulin | 2(0.9) | |
| Antihypertensive | Enalapril | 52(53.1) |
| Enalapril + Calcium channel blockers | 25(25.5) | |
| Enalapril + beta blockers | 7(7.1) | |
| Others* | 14(14.3) | |
| Lipid lowering medication | Simvastatin | 65(83.3) |
| Atorvastatin | 13(16.7) | |
| Antiplatelet | Aspirin | 77(35.6) |
| Other drug | Anti asthmatic | 11(19.6) |
| GIT drugs* | 12(21.4) | |
| Cardiovascular drug** | 12(21.4) | |
| Antipains*** | 10(17.9) | |
| Antibiotics**** | 2(3.6) | |
| Other drugs***** | 9(16.1) | |
| History of drug allergies | - | 4(1.9) |
Table 3: Medication related variables among T2DM patients in Madda Walabu University Goba Referral Hospital, South-East East Ethiopia, 2017.
Drug therapy problems
Among the participants, 88% had at least one drug therapy problem, with the mean number of 2.06 ± 0.861; the maximum numbers of DTPs were four but half of the participants (50%) had two DTPs. A total number of 446 DTPs were identified across the seven categories. Need additional drug therapy were the highest (50.2%), followed by non-compliance to medication (21.7%). Dose too low, ineffective drug therapy and adverse drug reaction accounted 12.3%, 6.3% and 5% respectively. Unnecessary drug therapy and Dose too high were the least involved categories of DTPs. 3.6% and 0.7% percent respectively (Figure 1).
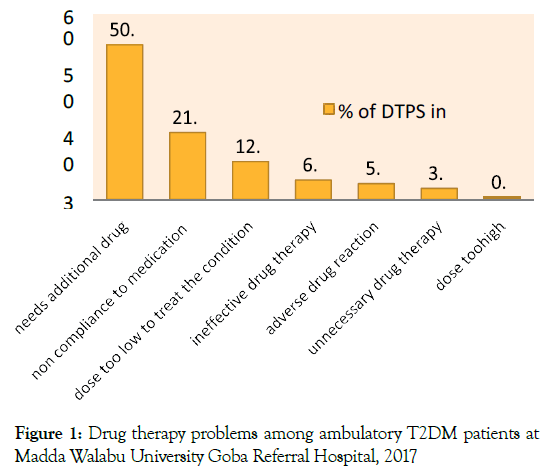
Figure 1. Drug therapy problems among ambulatory T2DM patients at Madda Walabu University Goba Referral Hospital, 2017
Causes of drug therapy problems
Requirement of preventive drug therapy was the leading cause for needs additional drug category (65.5%) and lack of understanding of the instruction (37.1%) was the frequent causes of problems for non-compliance drug therapy problems (Table 4).
| Category of DTPs | Causes for DTPs | Frequency (%) |
|---|---|---|
| Need additional therapy | 224(50.2) | |
| Preventive drug therapy required | 149(66.5) | |
| To attain synergistic/additive effect | 45(20.1) | |
| A medical condition that requires treatment | 30(13.4) | |
| Non compliance | 97(21.7) | |
| Does not understand the instruction | 36(37.1) | |
| Forgets to take medications | 20(20.6) | |
| Drug product too expensive for the patient | 22(22.7) | |
| Cannot swallow or self-administer the drug product appropriately | 1 | |
| The drug product is not available for the patient | 18(18.6) | |
| Dose too low | 55(12.3) | |
| The dose is too low to produce the desired effect | 54(98.2) | |
| The dosing is too infrequent to produce the desired effect | 1 | |
| Ineffective drug therapy | 28(6.3) | |
| Not the most effective for the medical problem | 28 | |
| Adverse drug reaction | 23(5.2) | |
| Safer drug product required due to risk factors | 16 | |
| Drug interaction causes an undesirable reaction that is not dose-related | 1 | |
| The drug product causes an undesirable reaction that is not dose-related | 6 | |
| Unnecessary drug therapy | 16(3.4) | |
| Multiple drug products are used for a condition that needs single drug therapy | 7 | |
| No valid medical indication for the drug therapy at this time | 9 | |
| Too high dosage | 3(0.7) | |
| The dose given is too high | 3 | |
Table 4: Causes of DTPs among T2DM patients in Madda Walabu University Goba Referral Hospital, South-East East Ethiopia, 2017.
Medications involved as the cause of DTPs
For the total 446 causes of DTPs, different class of medicines involved 455 times. Of the mediation indicated for T2DM and co existing conditions statin and metformin were the most frequently involved as the cause of DTPs, 33.6% and 20% respectively. Glibenclamide was the single least involved drug as the cause of DTPs (7%). Other drugs than the group of antidiabetic, antihypertensive, cholesterol lowering and blood thinners were the least (4.3%) (Table 5).
| Drugs involved as a cause of DTPs | Frequency (%) |
|---|---|
| Statin | 150(33.6) |
| Metformin | 89(20) |
| Anti-hypertensive | 66(14.8) |
| Insulin | 52(11.7) |
| Antiplatelet | 48(10.8) |
| Glibenclamide | 31(7) |
| Other drugs as the cause of DTPs | 19(4.3) |
Table 5: Common drugs involved in each category of DTPs among T2DM patients in Madda Walabu University Goba Referral Hospital, South-East East Ethiopia, 2017.
Pharmacists’ recommendations and interventions acceptance rate
Among the total 446 DTPs identified 94% intervention was done by pharmacists. The remaining (6%) of the identified DTPs were solved by the other health care teams before the intervention of the pharmacists. Half of the suggestions provided were addition of new drugs, followed by pharmaceutical counseling for adherence and dose adjustment 21.7% and 13% respectively (Figure 2). Of the interventions done for the problems, the acceptance rate was 72.6%, unknown status of acceptance 11.7% and not accepted for the interventions done were 15.7% (Table 6).
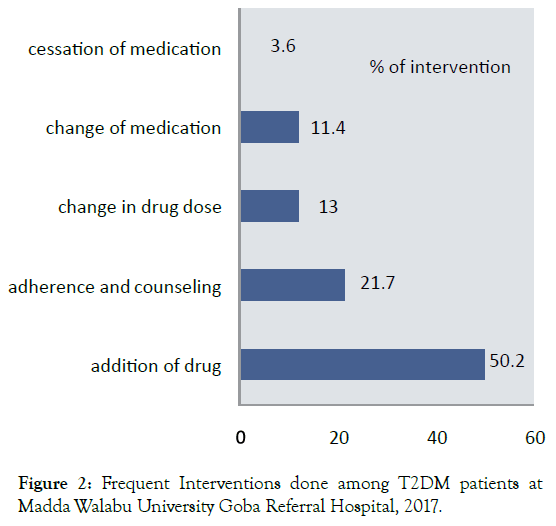
Figure 2. Frequent Interventions done among T2DM patients at Madda Walabu University Goba Referral Hospital, 2017.
| Intervention and acceptance rate | Frequency (%) |
|---|---|
| Intervention by pharmacist | 419(94) |
| By other health care team* | 27(6) |
| Acceptance | |
| Intervention accepted | 304 (72.6) |
| Intervention not accepted | 66 (15.7) |
| Accepted but not implemented | 49 (11.7) |
| *General practitioner, Nurses | |
Table 6: Intervention and acceptance rate of DTPs among T2DM patients in Madda Walabu University Goba Referral Hospital, South-East East Ethiopia, 2017.
Determinants associated with DTPs in logistic regressions
Even if five variables were associated with DTPs, only age group and hypertension were significant independent predictors on multivariable logistic regression analysis. Accordingly, it was found that the likely hood of having DTPs increases as the age of the patient increases. Patients with the age group of 46-59 years old were 3.5 times more likely to have DTPs [AOR, 3.537; 95% CI, 1.207-10.364; p=0.021], whereas those above 60 years old were 5.467 times more likely to have DTPs when compared to those less than 45 years old [AOR, 5.467; 95% CI, 1.599-18.693; p=0.007]. Similarly, patients with hypertensive disease were seven times more likely to experience drug therapy problems than their counter parts [AOR, 7.349; 95% CI, 2.020-26.735; p=0.002].
However, it also found that patients with medication greater than or equal to five were association to have DTPs, but not statistically significant [AOR, 1.306; 95% CI, 0.115-14.899; p=0.083] compared to those less than five medications per day (Table 7).
| Variables | COR (95% CI) | p value | AOR (95% CI) | p value | |
|---|---|---|---|---|---|
| Age ≤ 45 | 1 | - | 1 | - | |
| Age 46-59 | 5.750(2.058-16.068) | 0.001 | 3.537(1.207-10.364) | 0.021 | |
| Age ≥ 60 | 11.125(3.461-35.764) | 0 | 5.467(1.599-18.693) | 0.007 | |
| Family history | Yes | 1.810(.726-4.513) | 0.203 | 1.672(.612-4.572) | 0.316 |
| No | 1 | - | 1 | - | |
| ≥ Five medication | 9.173(1.211-69.449) | 0.032 | 1.306(.115-14.899) | 0.83 | |
| ˂ Five medication | 1 | - | 1 | - | |
| DM duration ≤ 4years | 1 | - | 1 | - | |
| DM duration 5-9years | 1.736(.706-4.271) | 0.23 | .856(.286-2.557) | 0.78 | |
| DM duration ≥ 10years | 8.500(1.093-66.115) | 0.041 | 1.957(.203-18.887) | 0.562 | |
| Co-morbidity | Yes | 4.757(1.998-11.324) | 0.001 | .792(.238-2.629) | 0.703 |
| No | 1 | - | 1 | - | |
| DM complication | Yes | 7.534(.992-57.195) | 0.051 | 4.031(.495-32.797) | 0.192 |
| No | 1 | - | 1 | - | |
| Hypertension | Yes | 12.288(3.563-42.382) | 0.001 | 7.349(2.020-26.735) | 0.002 |
| No | 1 | - | 1 | - | |
Table 7: Logistic regression analysis of the association between independent variables and DTPs among T2DM patients at South-East Ethiopia, 2017.
Among the study participants, 88% encountered at least one or more drug therapy problems. From the seven categories, a total of 446 DTPs were identified. The result of this study is relatively similar with the Huri et al., studies (90.5% and 90%) which had at least one drug therapy problem [23,24]. Similarly, Rao et al., study of Australia sample (90%) of participants had drug therapy problems [25].
The result of this study is higher number of DTPs than Al-Taani et al. [26] 81.2%, Minnesota [25] 70% and Cipolle et al. [27] 84% had at least one DTPs. The difference might be due to these studies were done in multicentre setting, large sample population were used and Participants who received atleast two glycemic control drugs included. Participants included in this study were those who had atleast one antidiabetic drugs. Good glycemic control and for further prevention of diabetic related risks more than one drug might be required, for example participants on insulin only needs metformin additionally for synergetic and extra benefit. Likewise, in the study unit the comprensive pharmaceutical care was not implemented previously to minimise the existence of drug therapy problems. This contributes for higher DTPs in our setting.
On the other hand, the result of this study is lower than Ogbonna et al. [28] 94% and the study in Switzerland almost all (100%) participants had at least one DTPs [29]. The discrepancies exist that would be attributed to a retrospective study method was used and participants who had took four or more drug therapy were the inclusion criteria in the above studies: those patients receiving complex drug regimen vulnerable for the existence medication related problems and would have more DTPs. Study settings, study populations and drug therapy problems classification methods variations also had a cause for the discrepancy.
From the seven classes of DTPs, half percent (50.2%) were under need additional drug therapy category. This was in line with the study by Cipolle et al. [27] which reported needs additional drugs as the most frequent problem (33%) [27]. Similarly, the study done in Australia and Minnesota sample reported needs additional drug was the most frequent problems [25].
In the Minnesota sample 59% the cause for needs additional drug therapy were indicated to prevent the onset of new medical conditions, however in this study around two third (65.5%) from those needs additional drug therapy the cause was requirement of preventive drug therapy [25]. The variation could be due to the utilization of risk preventative drugs, like statin, anti-platelet, antihypertensive and optimum utilization of metformin for control of diabetes and cardiovascular risk prevention was low in the study setting.
The second most common drug therapy problem in this study was non-compliance accounting 27% of the total DTPs, which is nearly similar result with the study done in Nigeria (26.1%) had compliance problem [30]. Non adherence to medication helps to cause complication and poor glycemic control. Study done at Tripoli, medication adherence accounts (36.1%) for poor glycaemic control [31]. Unnecessary drug therapy (4.5%) and dose too high (0.8%) was the least frequently involved categories DTPs.
The most frequent prescribed drug was glibenclimade with metformin (40.3%) followed by insulin injection (27.8%). Unlike this Ogbonna et al., study and Onah et al. study in Nigeria, Metformin was the most commonly prescribed antidiabetics agent [28-30]. The discrepancy might be the utilization of metformin not optimized according to the guide line in the study setting. Among the class of medication involved in DTPs the premier was statin (33.6%) and metformin (20%) followed by antihypertensive (14.8%). This was related with the study done in Malaysia, this could be the use of statin for cardiovascular risk prevention not to the optimum and not based on the intensity of the statin [24]. Likewise, the use of antihypertensive per the guide line as recommended for the diabetes mellitus patients not well practiced.
Among the DTPs identified pharmacists’ intervention was done for 94%, the rest six percent of the problems were solved by the other health care team before pharmacist recommendation. This was nearly similar to the study done in Chua et al (87.3%) recommendations were done by pharmacists [32]. Likewise, study done in India, almost all interventions were addressed by clinical pharmacists [22].
The most frequent suggestion given in this study was addition of new medicine (50.2%), it was different from studies done by Shareef et al. [22] in which clinical pharmacist frequent suggestion were on cessation of drug (17.98%) and clinical pharmacist interventions in India, 25.17% of frequent suggestion were cessation of drug [33]. These studies were the same prospective study design but the variation was due to the sample population difference included in the study, in the above studies admitted T2DM participants were included in the study. Patients admitted in the ward might be exposed unnecessary drug and pharmacists’ suggestions for termination of the problems might be higher than participants in the outpatient setting. Ambulatory patients visit the clinic for refill of previous diagnosis; lack of further investigation during each facility visit patients might not receive the medication for new diagnosis as well as for the prophylaxis therapy.
The overall physicians’ acceptance rates for suggestions given was 72.6% of the total recommendations, 11.7% of the intervention unknown status of acceptance and intervention not accepted were 15.7%. This finding was virtually similar to Chua et al., study in which 77.9% of changes recommended by the pharmacists were accepted [32]. The result of this study higher than the study by Shareef et al. [22] which only 58.20% of the recommendations was accepted.
Likewise, the study done in India, the acceptance rate of suggestions and the changes in drug therapy was 52.38% [33]. The disagreement might be resulted from these two studies were undergone in ward patients, patients were at critical and unstable conditions the acceptance rate of regimen change might not be noticeable.
Age group and hypertension were remained as independent determinants of drug related problems on logistic regression. Accordingly, the likely hood of occurrence of DTPs was increasing as age of the respondent increases. Participants found within the age group of 45-59 years about three times more likely to have DTPs than those below 44 years old [AOR, 3.537; 95% CI, 1.207- 10.364; p=0.021], whereas the factor increased to five times for elderly patients age greater than 60 years [AOR, 5.467; 95% CI, 1.599-18.693; p=0.007]. Association of advanced age with DTPs has agreed with scientific ground as it results in multiple disease conditions requiring additional drug for the prophylaxis and being forgetfulness prone for poor adherence and to have DTPs. This finding was in line with a study done in Florida, and in Jordan, but the study done in Malaysia Correspondingly, prevalence of hypertension had independent predictor of DTPs with significance of p value<0.002 levels [23,34,35]. The likely hood to had DTPs was seven times higher than patients who did not had hypertension [AOR, 7.349; 95% CI, 2.020-26.735; p=0.002]. Different studies were reported hypertension was the most prevalent co-morbid condition responsible DTPs [24-27]. This might be due to problem of selecting antihypertensive drug compiling to diabetes mellitus to the optimum dose, complex drug taking schedule which contribute non-compliance, adverse effect and cardiovascular risk that necessitate need of additional drug therapy which collectively result in increasing the chance of DTPs occurrence.
The major limitation of this study was, it is limited by chance of recall bias in adherence assessment as it was based on respondent’s self-report, missing of some data by chart review and lack of adequate organ function tests, only one study center and short study period of time had some of the limitations.
This study showed that majority of type 2 diabetes mellitus included in the study had at least one drug related problem showing optimal medication management in type 2 diabetes mellitus patients was a major challenge in clinical practice. Metformin with glibenclimide was the frequent prescribed drug for the participants. Need additional drug therapy due to underutilization of statin, metformin and antihypertensive for optimum utilization and cardiovascular risk prevention, the health care team working in DM clinic should be optimized underutilized medicines based on the guide line. Noncompliance and dose too low were the most common categories of drug related problems identified. Advanced age and hypertensive co morbidity were independently determining the occurrence of drug therapy problems. The study highlights the impact of clinical pharmacist in multidisciplinary health care team, which demonstrated that pharmacist interventions resulted in greater improvements in many drug therapy problems to achieve diabetes mellitus treatment goal.
The authors declared that they have no competing interests
The authors’ responsibilities were as follows. AM Participated in the design of the study, writing of results and discussion, performed the statistical analysis, drafting the manuscript and wrote the paper. TT performed analysis and interpretation of data as well as manuscript drafting. BB Participated in the design of the study, performed the statistical analysis and has been involved drafting of the manuscript. All authors read and approved the final manuscript.
The authors would like to thank Jimma University for approval of ethical clearance and technical and financial support for this study. The authors’ truthfully gratitude also go to, Madda Walabu University Goba Referral Hospital staffs, all data collectors and supervisors for actively participating during data collection and entire time.
Citation: Argaw AM, Hiwet TTG, Derse BB (2019) Drug Therapy Problems and Determinants among Ambulatory Type 2 Diabetes Mellitus Patients: Pharmacists’ Intervention in South-East Ethiopia. Endocrinol Metab Syndr 8:303. doi: 10.35248/2161-1017.19.8.303
Received: 18-Sep-2019 Accepted: 02-Oct-2019 Published: 09-Oct-2019 , DOI: 10.35248/2161-1017.19.8.303
Copyright: ©2019 Argaw AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited